This paper sought to evaluate individual exposure to air pollution by quantifying the carbon in alveolar macrophages (AMs) and its relationship to lung function. We also examined the proximity of participants’ residences to the Presidente Dutra highway (PDH) in adolescents with asthma from Taubaté, São Paulo, Brazil.
MethodsThis descriptive study examined fifty 13- to 14-year-old adolescents with asthma identified by the International Study of Asthma and Allergies in Childhood (ISAAC) in Taubaté. These adolescents underwent spirometry and sputum induction via the inhalation of 3% hypertonic saline (HSS). Sputum was collected after each nebulisation, and forced expiratory flow in one second (FEV1) was measured. The collected sputum was stored and transported to the laboratory; it was then processed and analysed for ultrafine particles (≤100nm). This analysis was correlated with the residence location and FEV1 of each adolescent.
ResultsA total of 39 adolescents completed the study. The comparison of the carbon fraction within macrophages (CA/MA) showed no differences according to residence in relation to the PDH (p=0.758). After adjustment, a mixed linear model with FEV1 as the dependent variable and CA/MA, location, and evaluation condition as the predictors found that the interactions among the variables were not significant.
ConclusionsThe amount of carbon present within the AMs of adolescents with asthma was not correlated with either lung function or residence location. Evaluations of the topography and local climatic conditions in Taubaté should be considered in future studies.
Air pollution has been identified as an important risk factor for the development and onset of asthma.1,2 An increased risk of allergic rhinitis and asthma related to factors such as urbanisation, and changes in lifestyle among other factors has been reported, especially in industrialised countries.3–5 This evidence has been primarily reported in studies that have compared urban and rural populations.6
Currently, approximately 50% of the world's population lives in urban areas, and these people are exposed to progressively higher levels of air pollutants.7 The harmful effects of exposure to intense motor vehicle traffic on human and animal airways lead to the development of allergic diseases and inflammatory reactions.8,9 These effects are the consequences of exposure to air pollutants such as volatile compounds and particulate matter (PM).
PM is a complex mixture of solid and liquid particles of varied sizes that are suspended in the air and contain heavy metals and polycyclic aromatic hydrocarbons. PM, mainly MP2.5, is the environmental pollutant most often associated with damage to human health8 in both clinical-epidemiological and experimental studies.8 Sulphur dioxide (SO2), ozone (O3), carbon monoxide (CO), carbon dioxide (CO2), nitrogen dioxide (NO2), heavy metals (Cd, Cu, Cr, Pb, Ni, Mn, and Zn) and polycyclic aromatic hydrocarbons are the main pollutants in the atmosphere. The effects of these pollutants are influenced by other factors such as wind, humidity, temperature, and the time they remain in the atmosphere.10
The detrimental effects of these pollutants depend to a large degree on the aerodynamic diameter of their particles because certain physical properties affect their ability to reach various levels of the respiratory tree. Smaller particles are more likely to reach the more distal portions of the airways, and very small particles are able to reach the alveoli.10
Children and the elderly are more vulnerable to the harmful effects of environmental pollutant gases, and increased exposure to air pollution reduces life expectancy.9 The World Health Organization (WHO) has estimated that approximately 20,000 deaths occur each year in Brazil as a result of exposure to environmental pollutants.11 Therefore, evaluations of exposure to air pollutants are important to improve population health and establish environmental control measures.12
Several methods are used to evaluate exposure to atmospheric pollution.34 The quantification of black carbon (BC) or ultrafine particle (≤100nm) within alveolar macrophages (AMs) might partially represent individual exposure to air pollution, especially in places where it is difficult to monitor environmental pollutant gases.13
This study sought to evaluate adolescents with asthma living in Taubaté and their exposure to air pollution by quantifying the BC within their AMs; we also examined the correlations between exposure and both lung function and residence location.
MethodsThis study was conducted in Taubaté, São Paulo in south-eastern Brazil (population: 299,423 inhabitants).14 Located 142km from the state capital, Taubaté is located on the Rio de Janeiro-São Paulo axis. It is a highly industrialised area and the second largest industrial centre of this central region. It is bisected by one of the major heavy vehicle-flow highways in the country, the Presidente Dutra Highway (PHD).15 A total of fifty 13- to 14-year-old adolescents with asthma previously identified by the International Study of Asthma and Allergies in Childhood (ISAAC) protocol were enrolled in this study.35 Briefly, 1039 adolescents completed the ISAAC written questionnaire, and 212 were identified as having asthma via an affirmative answer to the question “Did you experience wheezing over the last year?”.16 Of these adolescents, 50 were randomly selected and invited to participate in the current study. All of these adolescents were students at public or private schools and were categorised based on the proximity of their residence to the PDH, where far=more than 1000m; near=between 200 and 1000m; and very near=less than 200m.17
The lung function of these adolescents was evaluated before and after inhaling a beta2-agonist agent. The adolescents who were clinically stable or had a forced expiratory volume in the first second (FEV1)≥50% inhaled 10ml of 3% hypertonic saline (HSS) via a Pari® jet nebuliser. To obtain a sufficient quantity of sputum (i.e., ≥0.5ml)18 nebulisations were repeated four times on average in 5-minute intervals: A=5th minute, B=10th minute, C=15th, and D=20th minute. FEV1 was measured at these time points. If a decrease greater than 20% was detected, then the test was stopped, and the adolescent was treated with the inhaled beta2-agonist agent. After each nebulisation, the adolescent was instructed to cough and spit into a sterile polypropylene container. The adolescents were also asked about their use of drugs and tobacco.19
The sputum was stored in thermal bags with ice packs and transported to the Laboratory of Air Pollution (University of São Paulo, SP) in an average of 1.5–2h in accordance with recommendations.20 Then, the sputum was processed and analysed according to the recommended standards.18,21,22 Soon after sputum processing, 2–3 slides were prepared for each adolescent, and the best slide was selected for scanning and carbon counting within the macrophages. Panoramic Viewer (3D Histech) and Image ProPlus (Media Cybernetics) were used for this purpose. Then, the mean particle ultrafine area corresponding to the total carbon area (CA) over the total MA was determined. The data were stored individually in an Excel spreadsheet for analysis.
The Ethics Committees for Research at the Federal University of São Paulo and the University of Taubaté, SP, Brazil approved this study. Parents or guardians and all adolescents signed the free informed consent and assent documents, respectively.
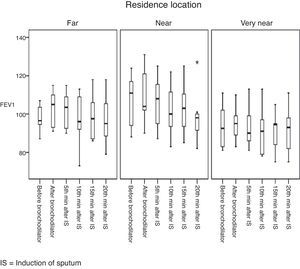
Data analysesThe adolescents’ characteristics were analysed using descriptive statistics. Absolute and relative frequencies were presented as categorical variables, and summary measures (i.e., means and standard deviations) were used for the continuous variables. The quartiles, minimums, and maximums are represented in a boxplot.
The comparison of the mean BC fractions by residence location in relation to the PDH was performed using analysis of variance (ANOVA). In addition, the effects of the carbon fraction and location relative to the PDH on FEV1 were evaluated using a mixed linear model36 that considered the adolescents as random effects. Both ANOVA and the mixed linear model assume data normality, which was verified using the Kolmogorov–Smirnov test. The mixed linear model verified the presence of interactions between the FEV1 evaluation condition and the effects of location and BC as well as the interaction between BC and location using likelihood ratio tests. The effects of the evaluation conditions were compared using contrasts.
The linear association between FEV1 and the variations in FEV1 (relative to FEV1 before bronchodilator; BBD) was evaluated using Pearson's correlation.
A significance level of 5% was adopted for all statistical tests.
The descriptive analysis and correlations were performed using SPSS 20.0. The mixed linear model was obtained using STATA 12.
ResultsOf the 50 adolescents with asthma, 39 (18 males) provided appropriate slides for the final analysis. All of the adolescents denied using tobacco or drugs. Fig. 1 shows the distribution of these adolescents by the location of their residence relative to the PDH: far=41%, near=33.3%, and very near=25.6%. The CA/MA did not differ by the location of the residence in relation to the PDH (Table 1).
Summary measures of CA/MA among adolescents with asthma according to location in relation to the President Dutra Highway.
| Distance | N | Mean±SD | Interval | Median | 1st–3rd quartile |
|---|---|---|---|---|---|
| Far | 16 | 0.45±0.31 | 0.11–1.17 | 0.31 | 0.22–0.61 |
| Near | 13 | 0.41±0.38 | 0.09–1.39 | 0.23 | 0.16–0.57 |
| Very near | 10 | 0.35±0.23 | 0.06–0.81 | 0.30 | 0.17–0.53 |
| Total | 39 | 0.41±0.31 | 0.06–1.39 | 0.31 | 0.19–0.53 |
CA/MA=carbon area/macrophage area, SD=standard deviation.
ANOVA: F(2, 36)=0.28, p=0.758.
Table 1 shows the mean FEV1 values at each time point and residence location. We ensured that adolescents started inhaling 3% HSS, presenting a mean FEV1 value above 90% of the predicted value; moreover, this value stayed constant through the end of the 4th triggering. Despite this protocol, we noticed higher FEV1 values before and after bronchodilation and at the 5th minute compared with the 10th, 15th and 20th minutes, regardless of the distance of the residence from the PDH (Fig. 1). Although we observed a decreasing trend regarding FEV1 across the sequence of inhalations, this trend was not significant. We call attention to an adolescent who lived near the PDH who presented a discordant FEV1 value 20min after the induction of sputum (identified by the asterisk).
Next, the mixed linear model was adjusted using FEV1 as a dependent variable and CA/MA, location of residence, and evaluation condition as well as the interaction between evaluation condition and CA/MA, the interaction between evaluation condition and time, and the interaction between CA/MA and location of residence as predictors (Table 2). This analysis showed no interaction between CA/MA and residence location, which does not elucidate whether the effect of the level of carbon with regard to FEV1 differs by location. Similar results occurred in relation to the interaction between the evaluation condition and CA/MA as well as between the evaluated condition and residence location (Table 2). Finally, no interaction was found between CA/MA and residence location, remaining significant only after FEV1 decreased due to the time after each nebulisation with HSS (Table 2).
Likelihood ratio tests for the mixed linear model.
| Model | Likelihood ratio tests | |||||
|---|---|---|---|---|---|---|
| Likelihood nL | DF | p | Chi | DF | p | |
| Location+carbon fraction+evaluation condition+evaluation condition×location+evaluation condition×AC/AM+location×AC/AM | −750.42 | 28 | 0.004 | – | – | – |
| Location+AC/AM+evaluation condition+evaluation condition×location+evaluation condition×AC/AM | −750.42 | 26 | 0.002 | 0.01 | 2 | 0.994 |
| Location+AC/AM+evaluation condition+evaluation condition×location | −753.65 | 21 | 0.002 | 6.45 | 5 | 0.265 |
| Location. AC/AM and evaluation condition of FEV1 | −762.40 | 11 | 0.003 | 17.5 | 10 | 0.064 |
| Location and evaluation condition of FEV1 | −762.41 | 10 | 0.001 | 0.01 | 1 | 0.903 |
| Evaluation condition of FEV1 | −762.70 | 8 | <0.001 | 0.58 | 2 | 0.746 |
nL=natural logarithm; N=205; CA/MA=carbon fraction (carbon area/macrophage area); Chi=Chi-square test; DF=degrees of freedom of the model.
No positive Pearson's correlation coefficient was found between the FEV1 values and CA/MA at all times of evaluation, nor was a relationship found between the carbon mean and the variations in FEV1 (in relation to FEV1 after bronchodilation) at all evaluations (data not shown).
DiscussionOver the last 250 years, air pollution has been present worldwide since the Industrial Revolution accelerated the exhaust-emission process that had previously been limited to household vegetable and mineral fuels and intermittent volcanic emissions.9
With the Industrial Revolution, production using technologies dependent on fossil fuels such as coal began to intensify, and health problems have appeared in the population due to air pollution. With the increase in urban-industrial activities and the creation of large and populous urban centres came an increase in the concentrations of pollutants and the spatial coverage of these substances affecting local residences.23
The effects of air pollution on individual health vary according to age. The susceptibility of newborns and the elderly to exposure to a single chemical can vary over the stages of growth and development. Children of different ages can react with different sensitivity patterns to certain chemicals and, in some cases, might be less sensitive than adults.24
Globally, children are exposed to situations of human vulnerability that must be considered when analysing the possible health effects of exposure to environmental pollutants. Indicators such as income, level of education, access to health and sanitation services, leisure, and the family life cycle can trigger or aggravate risk factors, making children more vulnerable.25
The degree and type of interaction with the environment varies according to age, cultural patterns, and housing areas. Children who live in large urban centres are more susceptible to the effects of the pollutants characteristic of these locations, such as the air pollution due to an excess of vehicles and nearby factories; the contamination of objects, furniture, food, and air by intradomiciliary pesticides; and the inhalation of chemicals used to clean homes or those present in paint and the interior walls of houses.26
Early air-quality standards established higher pollutant concentration levels. However, improvements in epidemiological resources have revealed that air pollutants can have deleterious effects on human health even at concentrations below the safety limit established by law.37
To evaluate the effects of air pollution on a population, it is important to choose an accurate and reliable method for assessing exposure to environmental pollutants. The current results might help control pollutants and provide data for the establishment of more effective measures via health policy actions.38 One method for evaluating the individual exposure of children and adolescents to pollutants due to motor vehicle traffic is the quantification of ultrafine carbon particles within AMs.13,36
In a previous study, we documented a more marked prevalence of asthma and rhinitis among adolescents living in Taubaté who resided near or very near the PDH. This location was identified as a risk factor for asthma.16 Despite this finding, the current study sampled the same population but did not document differences in the quantity of BC in the AMs of adolescents with asthma according to residence location in relation to the PDH.
This null result might be because of the variability in the PM concentration and consequent BC level due to wind and the local climate; thus, the highest concentrations might not be located closest to the PDH. The city's air quality not only depends on the amount of pollution released by emission sources but also on how the atmosphere concentrates and disperses these pollutants. The pollutant dispersion and removal phenomena might be controlled by regional atmospheric features (e.g., the state, speed, and direction of the wind and rain), local aspects of the urban climate (e.g., heat islands and air circulation), and urban surface characteristics (e.g., natural and built-up topography that interferes with the wind field, streets, buildings, and land use).27 In conditions of high atmospheric stability, pollutant gases can travel over long distances and lead to situations of higher concentrations at ground level, even when no nearby pollution sources exist. The dispersion and concentration of a pollutant in the atmosphere primarily depends on weather conditions and only secondarily depends on the parameters and conditions under which this emission is produced at the source (i.e., the speed and temperature of the gases).32 Weather conditions are important factors for defining air pollution levels to influence the length of stay of a pollutant in the place of its release because the contaminant is affected by variables such as wind speed and direction, precipitation rate, temperature, air instability, and others as soon as it is emitted into the Earth's atmosphere. The relationship between pollutants and climatological variables determines whether contaminants remain in the air in their initial state, whether they change their composition, or whether they are dispersed to a new location. At a micro-scale, other characteristics of the region such as its topography, the existence of buildings, soil type, and the quantity and type of vegetation also determine the path of the pollutants emitted into the atmosphere. These local features have the ability to modify the microclimate of a region and can lead to the formation of phenomena such as heat islands. These climatic local changes in relation to external extremities can create a microclimate that favours pollutant dispersion, deteriorating the air quality in a specific location.23 Another hypothesis is that the irritation caused by atmospheric pollutants in children, particularly those with asthma, can result in significant bronchial obstruction. Consequently, higher concentrations of BC cannot be inhaled by residents who live near the PDH.28
In addition, we did not observe a relationship between the amount of carbon and the changes in lung function in the sample. Thus, 100% of the sample had baseline FEV1 values above 80% of the predicted values, suggesting that these adolescents generally had stable lung function at the time of sputum collection. This finding complicates the correlation between disease severity and CA/MA with regard to this group.
A decrease in FEV1 was observed among all adolescents after the beginning of the 3% HSS inhalation for sputum induction; however, only seven adolescents needed to stop the nebulisation because of a greater than 20% decrease in FEV1 (i.e., 82.1% of the adolescents continued induction and produced a suitable amount of sputum as was reported in previous studies using the same method).38,39
Our study did not show that the individual exposure of adolescents with asthma to BC was higher in the group who lived near/very near the PDH compared with the group who lived farther away. Furthermore, no correlation was found between impaired lung function and inhaled PM, defined here as the mean BC in the studied adolescents. Similarly, Grigg et al.31 showed a weak correlation between CA/MA and exposure to PM10 according to the child's place of residence and a negative correlation between the mean of carbon and FEV1 in their studied patients.
ConclusionsWe did not document relationships between the amount of carbon present in the AMs of adolescents with asthma and either their lung function or place of residence. Although the quantification of carbon is an important technique for evaluating individual exposure to air pollutants, few studies have been performed to assess children and adolescents. Furthermore, other issues, including evaluations of topography and local climatic conditions, must be taken into account when conducting future studies in Taubaté.
Ethical disclosuresConfidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Protection of human subjects and animals in researchThe authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.
Conflict of interestThe authors declare that they have no conflicts of interest.