The aim of this study is to compare performance of two biopsy approaches in patients with at least one previous negative prostate biopsy (PB): classical transrectal biopsy (ClTB) versus cognitive registration biopsy (COG-TB).
Material and methodsA retrospective study of 205 patients with at least one negative PB. 144 (70.2%) patients underwent a prior mpMRI and 61 (29.8%) patients did not.
Nodule classification was carried out according PI-RADS version 2. Peripheral zone (PZ) grouped pZa, pZpl and pZpm areas, transition zone (TZ) Tza, Tzp and Cz areas, and anterior zone (AZ) AS areas.
COG-TB was conducted in patients with previous mpMRI (144); while in the remaining 61 (29.8%) patients a ClTB of PZ and TZ was performed.
Statistical analysis was performed using Chi square and T-student tests for qualitative and quantitative variables, respectively. Multivariate analysis was carried out in order to identify predictive variables of prostate cancer.
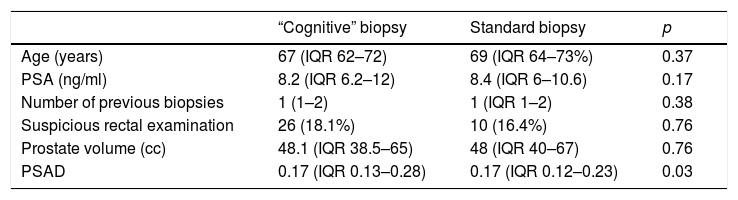
ResultsMedian patient age was 68 (IQR 62–72) years, median PSA was 8.3 (IQR 6.2–11.7) ng/ml and median previous biopsies was 1 (IQR 1–2). Digital rectal examinations (DRE) findings were normal in 169 (82.4%) patients and suspicious in 36 (17.6%) patients (cT2a-b in 34 patients and cT2c in 2). Median prostate volume was 48 (IQR 38–65) cc. Statistically significant differences in PSAD between both groups were found (p=0.03).
Transrectal ultrasound (TRUS) showed hypoechoic nodules in 8 (13.1%) ClTB patients and in 62 (43.1%) COG-TB patients (p=0.0001).
The median number of biopsy cylinders per set of prostate biopsies was 10 (IQR 10–10) in ClTB group and 11 (IQR 9–13) in COG-TB group (p=0.75).
Cancer was diagnosed in 74 (36.1%) patients: of them, 10 (16.4%) were ClTB patients and 64 (44.4%) COG-TB (p=0.0001).
Tumors classification was as follow: ISUP-1: 34 (45.9%), ISUP-2: 21 (28.4%), ISUP-3: 9 (12.2%), ISUP-4: 7 (9.5%) and ISUP-5: 3 (4.1%). No significant statistical differences were found (p=0.89). The median number of biopsy cylinders impaired per set of prostate biopsies was 1 (IQR 1–5) in ClTB group and 2 (IQR 1–4) in COG-TB group (p=0.93).
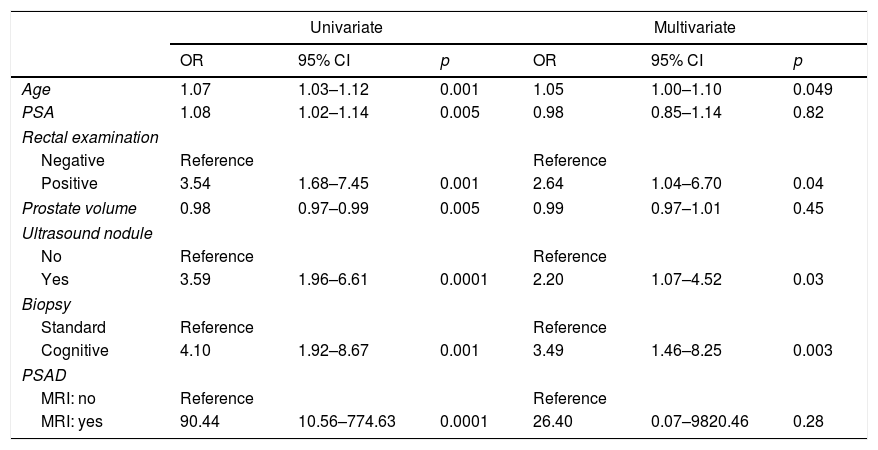
Regarding independent predictive variables for prostate cancer the results were: age (OR=12.05; p=0.049), suspicious DRE (OR=2.64; p=0.04), hypoechoic nodule (OR=2.20; p=0.03) and mpMRI +COG-TB sequence (OR=3.49; p=0.003).
ConclusionsIn patients with at least one negative PB, mpMRI+COG-TB sequence improves 3.5 (OR=3.49) times the diagnosis prostate vs. ClTB.
El objetivo es comparar el rendimiento de la secuencia resonancia magnética (RM) y biopsia transrectal «cognitiva» (BTRCog) frente a la biopsia transrectal clásica (BTRCl) en pacientes con al menos una biopsia de próstata (BP) negativa.
Material y métodoAnálisis retrospectivo de 205 pacientes con al menos una BP negativa. A 144 (70,2%) pacientes se les realizó antes de la biopsia una RM y a 61 (29,8%) no.
Los nódulos se clasificaron según la clasificación PI-RADS v2 agrupando pZa, pZpl y pZpm como zona periférica (ZP), Tza, Tzp y CZ como zona transicional (ZT) y áreas AS como zona anterior (ZA).
A los pacientes con RM se les realizó BTRCog. A los pacientes sin RM se les realizó una BTRCl de la ZP y de la ZT.
Comparación de variables cualitativas con test de la chi2 y de cuantitativas con t de Student. Análisis multivariante (regresión logística) para identificar variables predictoras.
ResultadosLa mediana de edad fue 68 (IQR 62-72%) años, de PSA 8,3 (IQR 6,2-11,7) ng/ml y del número de biopsias previas fue 1 (IQR 1-2). En 169 (82,4%) el tacto rectal (TR) fue normal, mientras que en 36 (17,6%) sospechoso (cT2a-b en 34 y cT2c en 2). La mediana del volumen prostático (VP) fue de 48 (IQR 38-65) cc. Existió diferencia en el PSAD (p=0,03) entre ambos grupos.
En la ETR se identificó nódulo hipoecoico en 8 (13,1%) pacientes con BTRCl y en 62(43,1%) (p=0,0001) con BTRCog.
La mediana de cilindros extraídos en BTRCl fue 10 (IQR 10-10) y en el grupo BTRCog fue 11 (IQR 9-13) (p=0,75).
Se diagnosticó cáncer en 74 (36,1%) pacientes. En BTRCl 10 (16,4%) y en BTRCog 64 (44,4%) (p=0,0001).
Los tumores diagnosticados fueron clasificados: ISUP-1: 34 (45,9%), ISUP-2: 21 (28,4%), ISUP-3: 9 (12,2%), ISUP-4: 7 (9,5%), ISUP-5: 3 (4,1%). No existieron diferencias (p=0,89). La mediana de cilindros afectados en BTRCl fue 1 (IQR 1-5) frente a 2 (IQR 1-4) en el grupo BTRCog (p=0,93).
Variables predictoras independientes de cáncer: edad (OR=12,05, p=0,049). TR sospechoso (OR=2,64, p=0,04), nódulo hipoecoico en ecografía (OR=2,20, p=0,03) y la secuencia RM+BTRCog (OR=3,49, p=0,003).
ConclusionesLa secuencia RMNmp +BTRCog en pacientes con al menos una BP previa negativa multiplica casi por 3,5 (OR=3,49) la probabilidad de diagnosticar un cáncer frente a la BTRCl.