Subclinical depression is a prevalent condition with important implications for patients’ functioning and well-being. However, there is a lack of studies operationalizing its definition and studying its clinical significance and health impact in depth. This work analyses subclinical depression impact on a health status score derived from eight heath domains, and its prevalence in Spanish population.
MethodsThe sample was selected from World Health Survey database, choosing the answers for Spain of people with a diagnosis of subclinical depression and no depressive disorders.
ResultsControlling the interaction of the different demographic variables, being female was the only significant predictor for the presence of subclinical depression. A worse health status is associated with subclinical depression, being female, a higher age, lower incomes, less years of formal education and being widowed. The decrease is significant in the eight health domains composing the score.
ConclusionsThe necessity of a better conceptualization of the nature of clinical depression is highlighted, going in depth in different proposals defending a definition based on clinical signification rather than in the number of depressive symptoms, with the goal of avoiding the pathologization of human suffering and inherent distress to several vital situations.
La depresión subclínica es una condición prevalente que presenta importantes implicaciones para el funcionamiento y el bienestar de los pacientes. Sin embargo, faltan estudios que operativicen su definición y que profundicen en su significación clínica y su impacto en la salud. El presente trabajo analiza el impacto de la depresión subclínica sobre un indicador de salud compuesto por ocho dominios de funcionamiento, y su prevalencia en la población española.
MétodoLa muestra se ha extraído de la base de datos de la Encuesta Mundial de Salud de la OMS, seleccionando las respuestas para España de personas con depresión subclínica y sin depresión.
ResultadosControlando la interacción de las distintas variables demográficas, ser mujer resulta ser el único predictor significativo para la presencia de depresión subclínica. Un peor estado de salud se asocia significativamente con presentar depresión subclínica, ser mujer, tener una edad elevada, un bajo nivel de ingresos, un menor número de años de educación formal y ser viudo. La disminución resulta significativa en los ocho dominios de funcionamiento que conforman el índice.
ConclusionesSe pone de manifiesto la necesidad de conceptualizar mejor la naturaleza de la depresión subclínica, profundizando en la línea de recientes propuestas que abogan por una definición basada en su significación clínica más que en el número de síntomas depresivos, con el objetivo de no patologizar el sufrimiento humano y el malestar inherente a muchas situaciones vitales.
Subclinical depression is a disorder that is highly prevalent in routine medical practice but scarcely recognized in the current diagnostic manuals, where it is categorized as a “non-specific depressive disorder.” Although there is a wide variety of definitions found in the literature, based on the number of symptoms and their duration and the associated impact, the Judd et al. definition from 19941 is accepted as the standard definition: “two or more simultaneous symptoms of depression, present most of the time for at least two weeks, associated with evidence of social dysfunction, in an individual who does not meet the diagnostic criteria for minor depression, major depression, and/or dysthymia.” The incidence of subclinical depression ranges from 2.3%2 to 12.9%,3 with higher percentages in primary care.4
There is an association between quality of life and the presence of depressive symptoms that do not meet the diagnostic criteria for major depression or depressive episode. Rucci et al.4 found that there was increased disability in activities of daily living in individuals with subclinical depression, which was also associated with significant psychological distress and poor perception of health. In 2007, Da Silva Lima and de Almeida Fleck5 observed that patients with subclinical depression suffered a greater impact on their quality of life than those who had no depressive symptoms and that, of all the groups studied, it was the patients with major depression who experienced the worst impact on their quality of life.
Backenstrass et al.6 found that patients with subclinical depression were significantly impaired in their functioning and in their daily activities in comparison with non-depressed primary care patients. Maier et al.2 proposed that patients with depression that is subclinical and brief have a social disability comparable to patients with major depression. Lastly, looking at how many days in the previous month patients were incapable of working, Goldney et al.3 reported that the mean number of days for patients with subclinical depression was higher than the mean for control group subjects. These authors found a continuum of disability associated with depression where individuals with major depression manifested the greatest disability of all.
In 1997, Judd et al.7 reported significant increases in the use of healthcare services, as well as an increased psychological disability related to subclinical depressive symptoms, this disability increasing in proportion to the severity of the depressive symptoms. Goldney et al.3 came to the conclusion that patients with subclinical depression used healthcare services to a significantly greater extent than non-depressed patients. Ayuso-Mateos et al.8 found that subclinical depressive conditions cause a significant decline in health status and that the differences found are not between the various levels of depression but rather in comparison to non-depressed individuals.
The impact of subclinical depression on the health and well-being of the people of Spain has been analysed using data obtained from the World Health Survey—a World Health Organization (WHO) study reporting data from 68 countries across all regions of the world.
Materials and methodsSampleHaving obtained the results of the WHO World Health Survey from the public database, the responses for Spain were selected. Conducted in 2002 in a total of 68 countries representing all regions of the world, this survey included a total of 252,503 individuals. Its objective was to obtain valid and relevant information on the functioning, contributions, and achievements of healthcare systems and to evaluate whether improvements in these systems in certain countries were having the desired effect. A multi-stage, stratified, probabilistic sampling by conglomerates was conducted, without reposition, on an ideal sample of 5000 individuals per country.
AssessmentsAll participants were interviewed using the WHO World Health Survey, including demographic characteristics, economic status, diagnosis, treatment, and symptoms of depression.
The health domains and questions included on the survey are based on the work done to revise the International Classification of Functioning, Disability, and Health (ICF) and to develop evaluation instruments based on it, such as the Disability Assessment Schedule (WHODAS II). A mental health module (depression and alcohol abuse) based on the WHO Composite International Diagnostic Interview (CIDI) was specifically included in the survey.
The sample for this study was obtained by selecting the responses for Spain from the WHO World Health Survey public database. From these responses, individuals diagnosed with subclinical depression per the ICD-10 Diagnostic Criteria for Research and individuals with no diagnosis of depression were selected.
Subclinical depression: individuals in this group had at least one symptom from Criterion B of the ICD-10-DCR (depressive mood, loss of interest, easily fatigued) but did not meet the criteria for a diagnosis of depressive episode because they did not have the required minimum of four symptoms. They did meet the criteria of having symptoms most of the day and for a minimum of 2 weeks.
Non-depressed: this group included individuals who did not meet the diagnostic criteria for any type of depressive disorder.
Health statusThe health status assessment was based on 16 questions relative to problems with functioning over the previous 30 days. These questions were grouped into the following eight health domains:
- -
Mobility: problems moving about in his/her environment and carrying out activities requiring a certain vigour.
- -
Self-care: problems with self-care and maintenance of physical appearance
- -
Vision: difficulty seeing and recognizing someone across the street (20m), seeing an object at arm's length, or reading.
- -
Pain and discomfort: body pains and general body discomfort.
- -
Interpersonal skills: problems with personal relationships and community involvement and with handling conflicts and tensions.
- -
Sleep and energy: trouble sleeping and problems feeling rested and recovered.
- -
Mood: feelings of sadness, discouragement, worry, and anxiety.
- -
Cognition: trouble concentrating and remembering things and difficulty learning a new task.
The responses to each question were coded on a 5-point scale from “no difficulties or problems” to “extreme difficulty/disability.” The domains included are based on those routinely used on questionnaires like the Short Form-12 (SF-12) and the EuroQol (EQ-5D). Based on item response theory, the responses to the 16 questions were scored using a partial credit model that allowed a composite health status score to be generated. The raw scores were transformed via a Rasch model into a continuous cardinal scale, where 0 indicated the worst health status and the maximum score of 100 indicated the best possible health status.8,11
ResultsSample size and incidenceThe sample analysed was 5542 subjects—5459 with no diagnosis of depression and 83 with a diagnosis of subclinical depression, per the ICD-10 Diagnostic Criteria for Research. The raw incidence of subclinical depression was 1.3%, and the sex- and age-adjusted incidence was 1.4%. These same data reveal an incidence adjusted for major depression of 6.9% in Spain.8
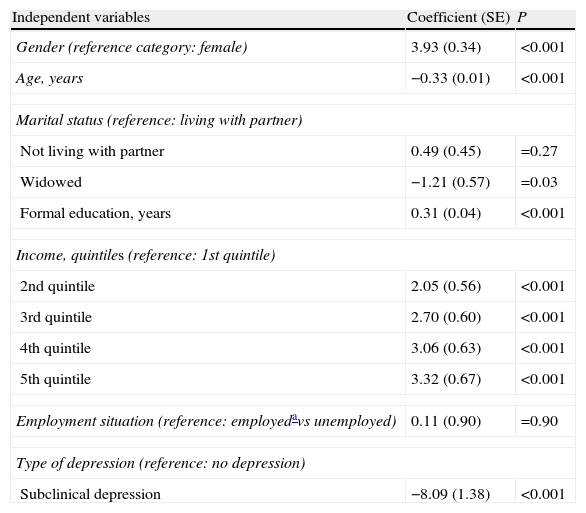
Comparison of predictorsThe correlation between health status, type of depression, and socio-demographic variables was calculated via linear regression, the results of which are shown in Table 1. R2 is 0.309 and the corrected R2 is 0.308, indicating that 30.8% of the dependent variable's variability is explained by the model. The results that were shown to be statistically significant indicate that the women have a poorer health status than the men. Increasing age is associated with reduced health status, as is being in a lower income quintile and having fewer years of formal education. In terms of marital status, not living with a partner correlates to a better health status than being married or living with a partner, although the results obtained are not significant. They are significant, however, for being widowed, which is the worst of the three categories in terms of health status. With regard to employment situation, there was hardly any connection found between this variable and health status; the results were not significant. Lastly, there is subclinical depression, the presence of which is the most weight factor in health status. Subclinical depression correlates to a poorer health status in comparison with patients who are not diagnosed with any type of depression.
Final equation for linear regression analysis: impact of subclinical depression on health status, controlling demographic variables.
| Independent variables | Coefficient (SE) | P |
| Gender (reference category: female) | 3.93 (0.34) | <0.001 |
| Age, years | −0.33 (0.01) | <0.001 |
| Marital status (reference: living with partner) | ||
| Not living with partner | 0.49 (0.45) | =0.27 |
| Widowed | −1.21 (0.57) | =0.03 |
| Formal education, years | 0.31 (0.04) | <0.001 |
| Income, quintiles (reference: 1st quintile) | ||
| 2nd quintile | 2.05 (0.56) | <0.001 |
| 3rd quintile | 2.70 (0.60) | <0.001 |
| 4th quintile | 3.06 (0.63) | <0.001 |
| 5th quintile | 3.32 (0.67) | <0.001 |
| Employment situation (reference: employedavs unemployed) | 0.11 (0.90) | =0.90 |
| Type of depression (reference: no depression) | ||
| Subclinical depression | −8.09 (1.38) | <0.001 |
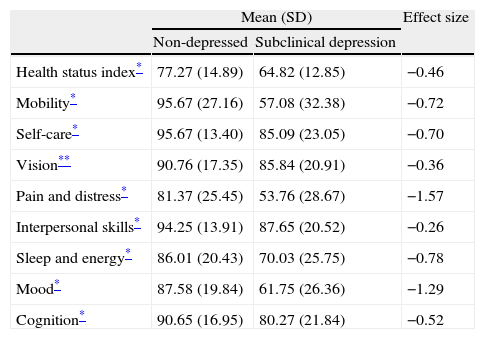
The mean score on the health status index and in the eight domains it encompasses is lower in all cases for the group with subclinical depression than for the individuals not diagnosed with any type of depression (Table 2). The differences are statistically significant for all of them, with a P<0.001 significance level, except for vision, where the significance level is 0.01. Based on effect size, the greatest differences are found in pain and discomfort, followed by sleep and energy, and then mobility.
Mean score on health domains in subclinical depression vs non-depressed.
| Mean (SD) | Effect size | ||
| Non-depressed | Subclinical depression | ||
| Health status index* | 77.27 (14.89) | 64.82 (12.85) | −0.46 |
| Mobility* | 95.67 (27.16) | 57.08 (32.38) | −0.72 |
| Self-care* | 95.67 (13.40) | 85.09 (23.05) | −0.70 |
| Vision** | 90.76 (17.35) | 85.84 (20.91) | −0.36 |
| Pain and distress* | 81.37 (25.45) | 53.76 (28.67) | −1.57 |
| Interpersonal skills* | 94.25 (13.91) | 87.65 (20.52) | −0.26 |
| Sleep and energy* | 86.01 (20.43) | 70.03 (25.75) | −0.78 |
| Mood* | 87.58 (19.84) | 61.75 (26.36) | −1.29 |
| Cognition* | 90.65 (16.95) | 80.27 (21.84) | −0.52 |
A series of logistic regression analyses were run, taking each of the eight health status domains as the dependent variables and, as independent variables, the presence of subclinical depression and the patient's age. The objective was to confirm that the reduced mean for the health domains was due to the presence of subclinical depression, primarily, and not to the effect of age, which is higher in this group. In all cases, the subclinical depression variable was of greater weight than the age variable.
DiscussionControlling the effect of the various demographic variables on predicting the presence of subclinical depression, the results of the binary logistic regression analysis for subclinical depression vs no depression showed that gender was the only significant predictor: with the remaining demographic variables controlled, being female is a significant predictor of subclinical depression. Comparing the non-depressed group with the subclinical depression group, in terms of demographic characteristics, revealed statistically significant differences for almost all variables analysed (employment situation and living with a partner being the exceptions); in that case, however, the differences were analysed separately for each variable without taking into account how they all interacted, as occurs in a binary logistic regression analysis. There are recent findings in the literature that all the demographic variables considered were significant as predictors of subclinical depression, but the sample size was much larger than that available in this case.8
Results of the linear regression analysis using health status index, demographic variables, and subclinical depression show that there is a significant association between poorer health status and subclinical depression, being female, being older, having a lower income level, having fewer years of formal education, and being widowed. These results have been found previously for the worldwide population.8 Not living with a partner is associated with better health status than living with a partner; however, as in the case of employment situation, the weight of this variable in the equation is not statistically significant. The reason for this lack of significance could be that only those individuals of working age who are actively seeking employment are included in the “unemployed” category, while the rest—individuals who are actively working, retired, laid off—are grouped in the “employed” category. As expected, the presence of subclinical depression is the variable most strongly associated with a poorer general health index.
Lastly, comparing the two groups in terms of mean health status index and the mean for the eight domains it encompasses, the differences are significant for all domains—even the vision domain which, on the face of it, would appear to have a less obvious association with subclinical depression. Although age is an important mediating factor—the subclinical depression group's mean age is higher, which could correlate to a lower score on the various domains of the health status index—when the effect of age is controlled through linear regression analysis, subclinical depression is found to result in decreases across all domains, even assuming age to be uniform. This indicates that subclinical depression has a clear impact on health, including key areas of the individual's functioning, and gives evidence of the connection between the presence of depressive symptoms and a decline in the quality of life. This is in keeping with recent studies reporting increased disability in activities of daily living in individuals with subclinical depression, associated with marked psychological distress and impaired functioning in these patients compared to individuals who do not have any type of depression.3,4,6,7
The impact of subclinical depression on the individual's functioning and health means it could be considered for inclusion in future classification systems for mental disorders. However, this would mean running the risk of pathologizing human behaviour and using medical treatment for the suffering and distress that are part of everyday, adverse circumstances that most individuals experience at some time in their life. To avoid this, recent studies have proposed that subclinical depression be conceptualized on the basis of a clinical significance criterion—how it impacts functioning and activities of daily living—instead of being limited to the symptom count alone.9,10 The clinical significance criterion is considered unnecessary in major depression because the symptoms required for the diagnosis, in and of themselves, mean that the individual's functional capacity is reduced. This is not a feature inherent to subclinical depression, however. For this reason, to meet the criterion of 1–3 depressive symptoms present, at least 1 of these should be a key symptom of the disorder—depressed mood, anhedonia, or easily fatigued. In any event, it would take further studies to define the boundaries of the depressive spectrum vs ordinary sufferings vs normality more precisely.
LimitationsFirst, the small sample size of individuals with subclinical depression (No.=83) affects the statistical significance of the analysis, as well as the binary logistic or linear regression, and gives rise to distributions that are hardly representative of the data for any of the demographic variables analysed.
Second, because this is a transversal study, it cannot be known whether the subclinical depression appears alone and independently, as an episode with its own beginning and end, or whether the depressive symptoms are part of the prodromal or residual phase of a major depressive disorder. For the same reason—this being a transversal study—it is not possible to determine the causal direction of the relationship between subclinical depression and health status. Longitudinal studies on this would have to be conducted so that the evolution of subclinical depression symptoms could be evaluated over time.
ConclusionsSubclinical depression is a prevalent condition that appears to be associated with a significant decline in health status.
This decline in health status affects all its components—those most commonly related to depressive symptoms, such as mood and sleep/energy, as well as others where the connection appears to be less direct, as in the case of vision.
A number of socio-demographic variables are more strongly associated with the presence of subclinical depression: being female, being older, having a lower level of income and formal education, and being widowed.
The impact of subclinical depression on health status is important enough to propose that its symptoms, course, and implications for daily living need to be better defined and that its inclusion in future diagnostic systems be evaluated.
The recognition of subclinical forms of depression should not lead to pathologizing either human behaviour or the distress inherent to adverse experiences of everyday life—hence, the interesting proposal that a clinical significance criterion be considered rather than basing it solely on the depressive symptom count.
Conflicts of interestMar Rivas is supported by the Programa propio para la formación del profesorado universitario, FPU-UAM [teaching fellowship at UAM], Universidad Autónoma de Madrid, Spain. The rest of the authors have no conflicts of interest to declare.
Pleace cite this article as: Rivas M, et al. Depresión subclínica en España: prevalencia e impacto sobre la salud. Rev Psiquiatr Salud Ment (Barc.). 2011;4:144–9.