To evaluate and compare the social cognition in patients with schizophrenia, healthy first-degree relatives and controls, by studying the relationship between social cognition and nonsocial cognition, psychopathology, and other clinical and sociodemographic variables.
MethodThe total sample was comprised of patients diagnosed with paranoid schizophrenia (n=29), healthy first-degree relatives (n=21) and controls (n=28). All groups were assessed with an ad hoc questionnaire and a Social Cognition Scale, which assessed the domains: emotional processing, social perception and attributional style in a Spanish population. The patient group was also assessed with the Scale for the Positive and Negative Syndrome Scale and the Mini-mental state examination. Statistical analyses were performed with SPSS version 15.0.
ResultsPatients scored significantly worse in all domains of social cognition assessed, compared with controls, and mastery attributional style, compared with relatives. The type of psychopathology correlated negatively and statistically significantly with different domains of social cognition: negative symptoms with emotional processing and attributional style, and positive symptoms with social perception. Basic cognition scores correlated positively and statistically significantly with the domains social perception and attributional style.
ConclusionSocial cognition has become an interesting object of study, especially in how it relates to non-social cognition, psychopathology and global functioning of patients, bringing new elements to be considered in the early detection, comprehensive treatment and psychosocial rehabilitation of patients. Its conceptualisation as trait variable, the consideration of the existence of a continuum between patients and relatives are plausible hypotheses that require further research.
Evaluar y comparar la cognición social en pacientes con esquizofrenia, familiares de primer grado y controles sanos. Estudiar la relación que guarda la cognición social con la cognición no social, la psicopatología y otras variables clínicas y sociodemográficas.
MétodoLa muestra total la formaron pacientes diagnosticados de esquizofrenia paranoide (n=29), familiares sanos de primer grado (n=21) y controles (n=28). Todos los grupos fueron evaluados con un cuestionario ad hoc y la Escala de Cognición Social que evalúa los dominios: procesamiento emocional, percepción social y estilo atribucional en la población española. El grupo de pacientes fue evaluado también con la Escala para el Síndrome Positivo y Negativo de la Esquizofrenia y el Mini-Examen Cognoscitivo. Los datos fueron analizados con el paquete estadístico SPSS versión 15.0.
ResultadosLos pacientes puntuaron significativamente peor en todos los dominios de la cognición social evaluados en comparación con los controles y en el dominio estilo atribucional en comparación con los familiares. El tipo de psicopatología correlacionó de forma negativa y estadísticamente significativa con dominios diferentes de la cognición social: la sintomatología negativa con el procesamiento emocional y el estilo atribucional y la sintomatología positiva con la percepción social. Las puntuaciones en la cognición básica correlacionaron de forma positiva y estadísticamente significativa con los dominios percepción social y estilo atribucional.
ConclusiónLa cognición social se ha convertido en un interesante objeto de estudio, especialmente por la relación que guarda con la cognición no social, la psicopatología y el funcionamiento global de los pacientes, aportando nuevos elementos a considerar en la detección precoz, el tratamiento integral y la rehabilitación psicosocial de los pacientes. Su conceptualización como variable de rasgo y la consideración de la existencia de un continuum entre pacientes y familiares son hipótesis plausibles que requieren mayor investigación.
Social cognition refers to the social cognitive processes involved in how we develop inferences about the other people's intentions and beliefs, as well as how we weigh social situational factors in making these inferences.1 Considering the different proposals reviewed in literature, we found the following components to form social cognition2: emotional processing, referring to the aspects related to perceiving and using emotions; theory of mind, or the ability to make inferences about the mental states of others, such as intentions, dispositions and beliefs; social perception, such as the ability to evaluate rules, social roles and social context; social knowledge, also known as social framework, which is the ability to identify elements that may characterise a certain social situation; and attributional style, or mode in which explanations and reasons are given for positive or negative outcomes in social situations. After the 1990s, with the publication of “The Cognitive Neuropsychology of Schizophrenia”,3 social cognition was converted into a distinct area of research. Its inclusion among the research domains for the MATRICS4 project (research on measurements and treatments to improve cognition in schizophrenia) and the existence of pioneering studies that presented social cognition as a mediating variable between basic cognition and social functioning5 have led to a considerable increase in research and review articles.6–10 This highlights the search for greater empirical support for the components of social cognition with numerous neuroimaging studies oriented towards finding a neurophysiological correlation11–13 between these components and certain cerebral areas. In addition, social cognition has contributed to clinical practice by emphasising that cerebral neuroplasticity and interpersonal processes are connected and involved in psychopathology, just as they are in psychopharmacological, psychotherapeutic and rehabilitative treatment.14
Despite abundant research in this knowledge area, numerous interesting questions remain unresolved and under study; for example, the relationship social cognition has with non-social cognition and with psychopathology, the difficulty in defining social cognition as a domain that is independent of or dependent on other cognitive parameters and whether to define it as a trait or state variable. In this respect, Cornblatt and Keilp15 proposed a continuum model in the aetiopathogeny of schizophrenia caused by the existence of an attention deficit that would condition information processing from infancy. In the same vein, several studies have found results that show that social cognition domains exhibit stable behaviour, which could be interpreted as representative of a trait variable. Langdon et al.16 found that patients with high schizotypy scores performed more poorly on theory of mind (ToM) tests. Other authors, such as Herold et al.,17 observed that paranoid patients in remission showed worse functioning than controls in tasks with irony as a stable trait. Janssen et al.18 compared ToM task performance in patients with schizophrenia in remission, in first-degree relatives and in controls with no family history of psychosis. They found that the patients presented the worse functioning, and that first-degree relatives obtained intermediate results between the patients and controls. These studies, among others, continue to contribute results that validate the line of research from the preliminary work of Wykes et al.,19 who found a deficit in ToM task performance in unaffected siblings of schizophrenic patients. However, other authors, such as Frith and Corcoran20 and Hardy-Baylé et al.,21 have pointed towards a modular conception of ToM that behaves as a state variable.
With respect to the relationship between social cognition and psychopathology, the model proposed by Frith is of interest. It established a correlation between ToM deficit and psychopathology,22 forming this classification: “desired action” disorders, associated with negative symptoms and disorganisation; disturbances in self-monitoring and individual intentions, associated with the development of external control delusions; and thought-monitoring disorders, associated with paranoid delusions. Regarding negative symptoms, Green and Nuechterlein23 and Nuechterlein and Dawson24 sustained that they correlated strongly with neurocognitive deficit and visual processing. Mazza et al.25 related psychomotor poverty to ToM deficits. With respect to positive symptoms, Walston et al.26 indicated that it is necessary to possess an intact ToM to develop delusions of persecution. Abu-Akel27 proposed a continuity model in ToM deficit that ranged from truly deteriorated ToM to hyper-ToM, which is associated with over-attribution of mental states and was proposed as a causal factor of paranoid states. The latest research has provided different data in this respect. Authors such as Brüne point out that IQ, without completely explaining the deficits, influences ToM functioning in patients in remission.28 Mazza et al.25 found significant variables in relation to working memory, while Greig and Bora et al.29 found a positive correlation between this and ToM. Pickup and Frith30 raised the notion that paranoid patients compensate for their ToM deficiency with their IQ.
Our study was related to several previous works in which social cognition in patients with schizophrenia and their healthy relatives were evaluated. Among these studies, that carried out by Eack et al.,31 which evaluated emotion recognition with results that pointed to its conceptualisation as a trait variable, found that relatives presented errors, over-attributing negative emotions to neutral faces and requiring more time to respond. Another similar study by De Achával et al.32 found that relatives and patients presented problems in comprehending blunders. Furthermore, these groups showed difficulties in comprehending irony.
Due to our interests in research on the relationship between social cognition and psychopathology, non-social cognition and psychosocial functioning of patients with schizophrenia,33–36 this study was carried out with the following objectives: evaluate social cognition in patients with schizophrenia, patients’ relatives and healthy controls to establish possible differences between the groups, as well as study the relationship between social cognition and non-social cognition, psychopathology and other relevant clinical and sociodemographic variables.
Materials and methodsThis case and control study was carried out in the Dr Negrín University Hospital of Gran Canaria, and the following 3 groups were assessed: patients, relatives and non-related controls. All participants voluntarily agreed to participate in this research and signed an informed consent form. The case group was formed by patients diagnosed with paranoid schizophrenia, aged 18–65 years, who had been admitted to the Brief Internment Unit of Psychiatry and had overcome the acute phase. Patients in their first psychotic episode were excluded to avoid including people with an undefined psychosis diagnosis. Those diagnosed with mental retardation or dementia were also excluded to control marked cognitive deficit, a possible confounding factor. The relative and control groups complied with the following criteria: no psychiatric history of psychosis, mental retardation or dementia. Relatives were selected by the greater degree of relation (first degree relatives before second degree) and by the variables sex and age so that they would share major characteristics with the patient. Controls were selected according to the criterion of homogeneity of sociodemographic variables such as age, sex and level of education with respect to the cases. By means of an interview and ad hoc questionnaire, the following sociodemographic variables were registered: age, sex, marital status (married or long-term relationship, single, separated, divorced, widowed), living situation (with family members or others, alone, in an institution), education level (illiterate, primary, secondary and higher studies) and work situation (active or on leave, unemployed, unable to work or early retirement due to mental illness). In the patient group, also using clinical history and information from family members and health personnel health, the following clinical variables were also collected: presence of other psychiatric diagnoses (including harmful toxic substance use or dependence) and psychiatric history in the family. Patients were evaluated using the following measures: Positive and Negative Syndrome Scale37,38 (PANSS), validated with patients in a Spanish sample to assess the intensity of positive, negative and general symptomatology presented upon admission and discharge, and the Mini-Cog Test (MEC-30 in Spanish),39 which is the well-known adaptation of the Mini-Mental State Examination (MMSE)40 to a Spanish sample, used to detect possible disturbances in the patient's basic cognition and to evaluate his or her functioning in this area. The Social Cognition Scale (SCS) was administered to the 3 groups (the relatives, unrelated controls and patients upon their discharge). This scale consists of an instrument designed and validated for the Spanish population41 by the same group that validated the Social Perception Scale42 used in national and international studies. The SCS makes it possible to evaluate 3 social cognitive domains: social perception, emotional processing and attributional style. The scale uses photographs of social content that differ in the numbers of elements (cognitive complexity) and in the emotional charge they present. These items reflect the ability to identify different aspects such as the elements present in the image, the image in its totality and facial emotions of the people, as well as whether appropriate inferences are made from the information available.
The following hypotheses were posed: firstly, patients would perform more poorly than the other groups on the social cognition test and their relatives would perform at an intermediate level between the patients and controls. This would bring us closer to considering social cognition as a trait variable and would permit theorising on the existence of prodromal symptoms useful in early diagnosis. Secondly, a relationship would be established between the patients’ social cognition and psychopathology (measured by PANSS) such that a higher grade would be associated with poorer performance in social cognition domains, being able to find differences based on symptomatology type (especially negative symptomatology). Lastly, low functioning in basic cognition (measured by the MEC) would also be associated with poorer performance in social cognition.
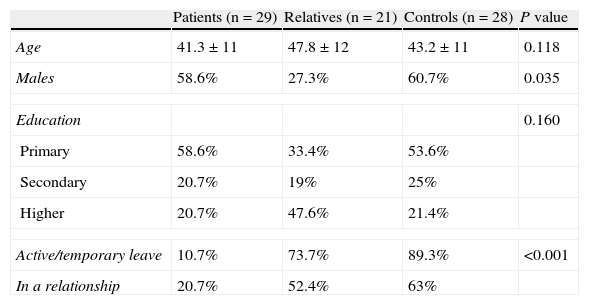
ResultsThe sample consisted of a total of 78 people: 29 patients, 21 relatives and 28 controls. The patients presented an evolution time of 16.3±10.5 years for psychosis, an untreated period of 2.7±7.4 years and a mean of 2.9±2.6 hospital admissions for decompensation. Of this sample, 12% of patients consumed tobacco, 6% alcohol and 6% cannabis. Patients with a family history of psychosis composed 14% of the sample. The relatives were mostly first degree relatives: 43% fathers and mothers, 43% siblings and 10% sons and daughters. We compared the sociodemographic variables of the groups (Table 1) and did not find any statistically significant differences in age or level of education. However, significant differences were found between the sexes, due to a greater female presence in the group of relatives. With respect to work activity, 10.7% of patients performed some activity, which turned out to be statistically and significantly less than in the other groups. In turn, the relatives presented less work activity than the controls. With respect to living as a couple, 20.7% of the patients maintained a stable relationship, a figure statistically and significantly less in comparison to relatives and controls.
Description of the sample.
| Patients (n=29) | Relatives (n=21) | Controls (n=28) | P value | |
| Age | 41.3±11 | 47.8±12 | 43.2±11 | 0.118 |
| Males | 58.6% | 27.3% | 60.7% | 0.035 |
| Education | 0.160 | |||
| Primary | 58.6% | 33.4% | 53.6% | |
| Secondary | 20.7% | 19% | 25% | |
| Higher | 20.7% | 47.6% | 21.4% | |
| Active/temporary leave | 10.7% | 73.7% | 89.3% | <0.001 |
| In a relationship | 20.7% | 52.4% | 63% | |
With respect to the 3 factors that the Social Cognition Scale measured (emotional processing, social perceptions and attributional style), our study did not find any significant correlations between the scores on these factors. This consequently confirmed that the test was capable of measuring them independently in our sample.
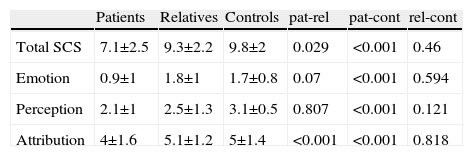
Upon comparing the results from the social cognition test in the groups assessed, we found that patients showed statistically significant worse scores in all social cognition domains evaluated compared to the controls, and worse scores in attributional style compared to the relatives. Upon comparing the 3 groups in total score for social cognition, we found differences that pointed towards a worse score in patients compared to relatives, as well as a worse score in relatives compared to controls. Nevertheless, with our sample, the differences between relatives and controls were not statistically significant (Table 2).
Intergroup differences in social cognition.
| Patients | Relatives | Controls | pat-rel | pat-cont | rel-cont | |
| Total SCS | 7.1±2.5 | 9.3±2.2 | 9.8±2 | 0.029 | <0.001 | 0.46 |
| Emotion | 0.9±1 | 1.8±1 | 1.7±0.8 | 0.07 | <0.001 | 0.594 |
| Perception | 2.1±1 | 2.5±1.3 | 3.1±0.5 | 0.807 | <0.001 | 0.121 |
| Attribution | 4±1.6 | 5.1±1.2 | 5±1.4 | <0.001 | <0.001 | 0.818 |
SCS: Social Cognition Scale.
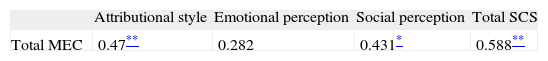
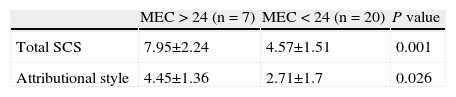
The patients’ scores in basic cognition (measured using the MEC) established positive and statistically significant correlations with the total score in social cognition, and concretely with the domains of social perception and attributional style (Tables 3 and 4). We continued with analysis by dividing patients into 2 groups according to their scores in basic cognition (MEC cut-off point). We found statistically significant differences, such that patients with worse cognitive functioning scored less in total social cognition (Table 4).
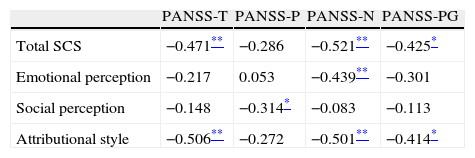
With respect to the relationship between the patients’ symptomatology (measured by PANSS) and social cognition (measured by the SCS), we found negative correlations. The following relationships were statistically significant: patients’ negative symptomatology with emotional processing and attributional style, positive symptomatology with social perception, and general psychopathology with attributional style. This is to say, the negative symptoms that patients presented were specifically related to the difficulty shown in perceiving and expressing emotions, as well as in giving significance and making causal attributions to social life events. Positive symptoms presented were related to the difficulties found in assessing rules, roles and social context.
The correlation between the items on the PANSS and SCS scales were studied, resulting in a mean of −0.26. The highest correlations occurred in the items from the negative subscale (PANSS-N) and in those from the general psychopathology subscale (PANSS-GP), such as attention deficit and volition disorders, which are related to negative symptomatology. Correlation of the specific item “conceptual disorganisation” from the PANSS was studied (due to the value given to disorganisation in the references), as well as the SCS scale. This correlation was among the highest between the positive subscale and social cognition. However, correlations with the items from the negative scale were higher (Table 5).
Psychopathology and social cognition.
| PANSS-T | PANSS-P | PANSS-N | PANSS-PG | |
| Total SCS | −0.471** | −0.286 | −0.521** | −0.425* |
| Emotional perception | −0.217 | 0.053 | −0.439** | −0.301 |
| Social perception | −0.148 | −0.314* | −0.083 | −0.113 |
| Attributional style | −0.506** | −0.272 | −0.501** | −0.414* |
PANSS: Positive and Negative Symptom Scale; SCS: Social Cognition Scale.
In order to ascertain the relationship maintained between sociodemographic variables and social cognition, we performed Pearson correlations and t-tests for equality of means. We found that age was not of statistical significance for any of the groups evaluated; neither was marital status or substance consumption. The gender variable showed significance in the group of relatives.
Level of education established significant differences between patients and controls in attributional style: the group of patients with secondary or higher studies (vs elementary studies) presented higher scores than the controls with this level of education. Likewise, the patients’ scores were lower if they had a lower level of education. Work situation turned out to be significant in the relatives and the controls, even though it did so in different ways for each group. In the group of relatives, those who worked showed better emotional processing, while controls who did not work showed better emotional processing. For the patient group, social cognition scores showed no significant correlations with period of evolution for psychosis or with psychosis period without treatment.
DiscussionFew studies are available that assess different components of social cognition in patients with subacute psychopathology, first degree relatives and controls. This makes it difficult to establish comparisons between the results of our study and previous research. It is also an opportunity in that this work was a novel study that assessed and compared social cognition in patients with schizophrenia after overcoming a phase of psychotic decompensation. Our results remain in line with other works such as those of Bediou et al.43 and Cavieres and Valdebenito,44 who found that social cognition domains were affected in patients with schizophrenia compared to controls. At the present moment, we cannot confirm the finding of an intergroup continuum for social cognition that would be explained by a greater deficit in patients and a moderate deficit in relatives, compared to controls. Nevertheless, some data lead us to think that, with a larger sample, we could find more significant results in this vein.32,45,46 With respect to the possible relationship between sociodemographic variables and social cognition, our study, like Bediou et al.,43 pointed towards the independence of age in the adult population, which contrasted with De Achával et al.32 In our study, education level among patients and controls was related to performance in attributional style, which is not the case in Bediou et al.43 In our study, the gender variable was significant in the group of relatives, while in the Cavieres and Valdebenito44 study, this variable was significant in the control group for emotional processing. Work situation was a significant variable for relatives and controls, but no previous results for this were found in the references reviewed.
With respect to the existing debate over conceptualisation of social cognition as a trait or state, the permanence of the deficit in patients after psychopathological improvement found in our study could be interpreted as a trait. However, we should consider, as pointed out by other authors, the possible influence and factor of confusion that presence of negative and residual symptomatology in patients could represent.47 Authors such as Corcoran and Frith,48 who lean towards the conceptualisation of social cognition as a trait, noted the existence of a primary deficit in domains like ToM, considering that patients with negative symptoms did not achieve adequate development of this domain. This position is based on the model developed by Fordor49 and in the existence of spectrum disorders, such as Asperger syndrome or William's syndrome. However, most studies reported that patients with schizophrenia did not present errors in basic tasks, but rather in those with greater complexity, such as second-order ToM tasks.50 This pattern could reflect normal development of social cognition before onset of the disorder. Schenkel et al.51 described a group of patients with poor social functioning during infancy, early onset of symptoms, clinical symptoms of disorganisation and deficit in second-order ToM tasks. Duñó et al.52 sustained the hypothesis formulated by Murray et al.53 and, in turn, by Pickup and Frith,30 defending the existence of a patient subtype with serious anomalies in social cognition in premorbid life stages.
With respect to social cognition and psychopathology, our study highlighted the significant relationship between patients’ negative symptomatology and deficits in different social cognitive domains. These results coincide with previous studies such as those from Frith and Hardy-Baylé et al.21 that predicted patients with prevalence of negative symptoms or disorganisation would have a greater deficit.
In regards to the relationship between social cognition and neurocognition, we found in our study that low scores on the Mini-Cog Test were significantly associated with low total scores on the Social Cognition Scale, and specifically associated with the social perception and attributional style domains. These results follow the line of recent studies that found correlation between basic cognition domains (especially IQ and working memory) and social cognition. Based on those findings, authors such as Brothers54 or Penn defined social cognition as a domain interrelated with non-social cognition, as well as with components that form it. In this sense, Penn referred to basic neurocognition as a necessary but not sufficient condition for adequate social cognition.55
As for the limitations of our study, the small size of our sample should be considered, although many studies with this research objective are being carried out using smaller samples. In our study design, a sole control group was established to pair with the patient group. Therefore, it would be interesting to count on another paired group for the relative sample. We administered only a single screening test and only to patients to measure non-social cognition. No treatment variables, such as antipsychotic drug type or dosage, were collected that would make interesting analyses possible.
In conclusion, social cognition is a broad, complex construct formed by different closely related domains. Its study provides new elements to consider in the comprehension of psychopathology (as well as for other conditions such as personality disorders, eating disorders, bipolar disorder and dementia, among others), the identification of at-risk population for better early detection, comprehensive treatment and psychosocial rehabilitation of patients. In this increasingly popular area of study, it is necessary to continue advancing in research because there are important theoretical and methodological difficulties, such as the scarcity of validated instruments and empirically corroborated theoretical models. Recent studies have focused on cerebral neuroimaging in the search for a specific neural substrate56 that points to new markers where psychopharmacology and psychotherapy can be of influence. Future research could also be aimed at the study of social cognition as a prognostic factor in schizophrenia and at establishing the relationship social cognition maintains with overall functioning of the patient.
Ethical disclosuresHuman and animal protection. The authors declare that the procedures followed conformed to the ethical standards of the committee responsible for human experimentation and were in agreement with the World Medical Association and the Declaration of Helsinki.
Data confidentiality. The authors declare that they followed the protocols of their work centre regarding publication of patient data and that all patients included in the study received sufficient information and gave their informed consent in writing to participate in said study.
Right to privacy and informed consent. The authors obtained informed consent from the patients and/or subjects mentioned in this article. This document is held by the corresponding author.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: Rodríguez Sosa JT, Gil Santiago H, Trujillo Cubas A, Winter Navarro M, León Pérez P, Guerra Cazorla LM, et al. Cognición social en pacientes con esquizofrenia, familiares de primer grado y controles sanos. Comparación entre grupos y análisis de variables clínicas y sociodemográficas relacionadas. Rev Psiquiatr Salud Ment (Barc). 2013;6:160–167.