Prevent hospitalizations in psychotic disorders is an important aim, so long-acting antipsychotic is a good option that can control better the correct adherence. Moreover, in the current economic context pharmacoeconomic studies are necessary. We estimate the effect in prevention of paliperidone palmitate long-acting injection (PP-LAI) and calculate the economic cost in the 12 months preceding the start of treatment with PP-LAI and 12 months later.
MethodsMirror image study of 71 outpatients diagnosed with psychotic disorders and treated with PP-LAI. In a first analysis, we measured along one year: number of hospitalizations/year, number of hospitalization in days, number of emergency assists/year and if there is antipsychotics associated to long-acting treatment. After this phase, we applied Fees Act of Valencia for economic analysis and estimate of the cost per hospitalization (€ 5640.41) and hospital emergency (€ 187.61).
Summary of resultsAfter one year of treatment with PP-LAI (mean dose=130.65mg/month), we obtained greater numbers in assistance variables: total hospitalizations decrease, 78.8% (p=0.009); shortening in hospitalization days, 89.4% (p=0.009); abridgement of number of emergency assists, 79.1% (p=0.002); decrease of rate of antipsychotics associated to long-acting treatment, 21% (p<0.0001); increase in monotherapy, 53.8% (p<0.0001). Therefore, after 12 months of treatment with PP-LAI we obtained a reduction in inpatient spending (savings of € 175,766.54) and increased spending on antipsychotics 32% (equivalent to € 151,126.92).
ConclusionsPP-LAI can be an effective therapy for the treatment of patients with severe psychotic disorders: improves symptomatic stability and can prevent hospitalizations with cost-effective symptom control.
Prevenir las hospitalizaciones en los trastornos psicóticos es un objetivo importante, por eso los antipsicóticos de larga duración son una buena opción debido a que aseguran un mayor control de la adherencia. Por otra parte, en el actual contexto económico, los estudios farmacoeconómicos son necesarios. Nosotros hemos estimado el efecto del palmitato de paliperidona de larga duración (PP-LAI) en la prevención y hemos calculado el coste económico en los 12 meses que preceden al inicio del tratamiento con PP-LAI y los 12 meses posteriores.
MétodosEstudio de imagen en espejo de 71 pacientes diagnosticados de trastorno psicótico y tratados con PP-LAI. En el primer análisis medimos a lo largo de un año: número de hospitalizaciones/año, número de hospitalizaciones en días, número de atenciones en Urgencias/año y si hay medicación antipsicótica asociada al tratamiento de larga duración. Después de esta fase, aplicamos la Ley de Tasas de la Generalitat Valenciana para el análisis económico y estimamos el gasto por hospitalización (5.640,41 €) y por urgencia hospitalaria (187,61 €).
Resumen de los resultadosDespués de un año de tratamiento con PP-LAI (dosis media=130,65mg/mes) obtuvimos mejores datos de las variables asistenciales: reducción del total de hospitalizaciones, 78,8% (p=0,009); acortamiento en los días de hospitalización, 89,4% (p=0,009); disminución en el número de asistencias en Urgencias, 79,1% (p=0,002); reducción en la proporción de antipsicóticos asociados al tratamiento de larga duración, 21% (p<0,0001); incremento de la monoterapia, 53,8% (p<0,0001). Además, después de 12 meses de tratamiento con PP-LAI obtuvimos una reducción en el gasto de los pacientes hospitalizados (ahorro de 175.766,54 €) y un incremento en el gasto de los antipsicóticos del 32% (equivalente a 151.126,92 €).
ConclusionesPP-LAI puede ser una terapia efectiva para el tratamiento de pacientes con trastornos psicóticos severos: mejora la estabilidad sintomática y puede prevenir las hospitalizaciones con un control sintomático coste-efectivo.
There is evidence that antipsychotic medications can improve and manage symptoms in patients with schizophrenia, but adherence to treatment is poor, with rates of non-adherence ranging from ∼40% to 60%.1 Prevent hospitalizations in psychotic disorders is an important aim, so long-acting antipsychotic is a good option that can control better the correct adherence because can improve adherence, reduce symptoms, and reduce the risks of relapse and rehospitalization, particularly for severely ill patients.2–4 Moreover, in the current economic context pharmacoeconomic studies are necessary, in our environment, to assess the actual cost of different antipsychotic treatments and what the overall cost is for society as a whole.5 The higher costs were driven mostly by increased hospitalizations and length of stay in hospital, which were also accompanied by higher costs for outpatient services and medications.6 Existing studies on the cost-effectiveness of PP-LAI show a reduction in overall costs compared with other treatments.7,8
In this study, we estimate the effect of PP-LAI in clinical indicators (prevention of clinical relapse, number of hospitalization days, number of emergency assists and if there is an antipsychotic associated) and calculate the economic cost of hospital interventions and antipsychotic treatment in the 12 months preceding to start treatment with PP-LAI, 12 months later and evaluation of their difference.
MethodsWe used a sample of 71 outpatients of Mental Health Center in La Mata (Torrevieja, Alicante). All data were anonymized and held securely in line with the Organic Law on Data Protection. Patients were aged between 19 and 76 years (inclusive) and both gender (32 women and 39 men), with a mean age of 43.5 years (SD 13.8). 15 of them were on couple or married and 56 were single or divorced. Just 11 patients lived alone (60 lived with other people) and 12 were working (59 were unemployed). All patients must be diagnosed with Psychotic Disorders (as per the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition [DSM-IV-TR] criteria): Schizophrenia 68%, Schizoaffective Disorder 13%, Psychosis not specified 11% and Delusional Disorder 8%. All of them must be treated with PP-LAI (≥28 days). In the other hand, exclusion criteria included: psychiatric diagnosis due to medication/substance abuse or a general medical condition; symptoms or signs of abstinent; history of neuroleptic malignant syndrome or tardive dyskinesia; women if is pregnant or not using an acceptable method of contraception unless postmenopausal for >1 year.
The design of the study is a mirror image (i.e., same patients assessing the period before and after receiving a long-term treatment) where sample is followed along one year (2013–2014). Assessments were done at two moments: at baseline, before initiation of PP-LAI (12 month pre-PPLAI); after 12 months of treatment with PP-LAI (12 month post-PPLAI).
The analysis is divided in two different phases. In a first analysis, we measured different clinical indicators: (1) total number of hospitalizations per year, (2) total number of hospitalization in days, (3) total number of emergency assists per year and (4) if there is antipsychotic associated to LAI treatment. After this phase, we applied Fees Act of Valencia9 for economic analysis and estimate (1) the cost per hospitalization (estimated average of € 5640.41 per patient)10 and (2) the cost hospital emergency (estimated average of € 187.61 per patient).10 At last phase, we evaluate the difference of all data between before initiation of PP-LAI and 12 months after, measured as percentage. We have done a descriptive analysis for data, nonparametric Mann–Whitney test for comparison of independent samples and Wilcoxon test for related samples contrast. The level of significance was set to α=0.05.
ResultsData retrieved was from the initial sample selected of 71 patients, with no cases of discontinuation. The mean dose of treatment with PP-LAI along the year was=130.65mg/month.
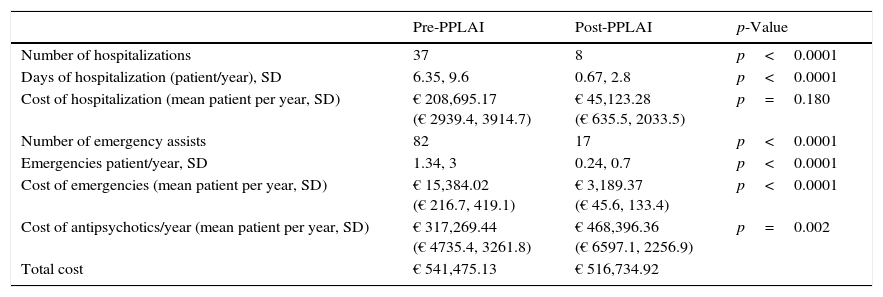
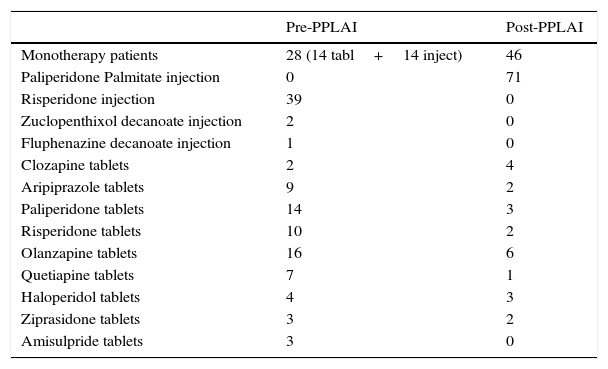
Assistance variables (Table 1) Rate of number of clinical relapses with hospitalization the year before PP-LAI initiation was 0.52 (SD 0.69) (hospitalizations per patient per year) and twelve months after PP-LAI was 0.11 (SD 0.36) (hospitalizations per patient per year), with a total hospitalizations decrease of 78.8% (p=0.009). There was a numerical decrease in the mean number of bed days per patient per year from one year before PP-LAI initiation (6.35, SD 9.6) to one year after PP-LAI initiation (0.67, SD 2.8). The median number of bed days decreased 89.4% (p=0.009). Number of emergency assists was 1.34 (SD 3) per year before PP-LAI and 0.24 (SD 0.7) a year later, with an abridgement of number of emergency assists of 79.1% (p=0.002). Likewise, mean of antipsychotics per patient was 1.9 (SD 0.63) one year before PP-LAI initiation and this mean reduced until 1.5 (SD 0.57) twelve months after PP-LAI, with a total decreased of 21% (p<0.0001) (Table 2). Other important data was the percentage of patients with monotherapy, that started being 39.4% and they ended up being 60.6% after the year, which reflects an increase in monotherapy of 53.8% (p<0.0001).
Assistance and economic data.
| Pre-PPLAI | Post-PPLAI | p-Value | |
|---|---|---|---|
| Number of hospitalizations | 37 | 8 | p<0.0001 |
| Days of hospitalization (patient/year), SD | 6.35, 9.6 | 0.67, 2.8 | p<0.0001 |
| Cost of hospitalization (mean patient per year, SD) | € 208,695.17 (€ 2939.4, 3914.7) | € 45,123.28 (€ 635.5, 2033.5) | p=0.180 |
| Number of emergency assists | 82 | 17 | p<0.0001 |
| Emergencies patient/year, SD | 1.34, 3 | 0.24, 0.7 | p<0.0001 |
| Cost of emergencies (mean patient per year, SD) | € 15,384.02 (€ 216.7, 419.1) | € 3,189.37 (€ 45.6, 133.4) | p<0.0001 |
| Cost of antipsychotics/year (mean patient per year, SD) | € 317,269.44 (€ 4735.4, 3261.8) | € 468,396.36 (€ 6597.1, 2256.9) | p=0.002 |
| Total cost | € 541,475.13 | € 516,734.92 |
Type of antipsychotics.
| Pre-PPLAI | Post-PPLAI | |
|---|---|---|
| Monotherapy patients | 28 (14 tabl+14 inject) | 46 |
| Paliperidone Palmitate injection | 0 | 71 |
| Risperidone injection | 39 | 0 |
| Zuclopenthixol decanoate injection | 2 | 0 |
| Fluphenazine decanoate injection | 1 | 0 |
| Clozapine tablets | 2 | 4 |
| Aripiprazole tablets | 9 | 2 |
| Paliperidone tablets | 14 | 3 |
| Risperidone tablets | 10 | 2 |
| Olanzapine tablets | 16 | 6 |
| Quetiapine tablets | 7 | 1 |
| Haloperidol tablets | 4 | 3 |
| Ziprasidone tablets | 3 | 2 |
| Amisulpride tablets | 3 | 0 |
Economic analysis (Table 1) Year before PP-LAI, we have got a spending mean in hospitalization per year and patient of € 2939.4 (SD 3914.7) (total of € 208,695.17) and € 216.7 (SD 419.1) (total of € 15,384.02) in emergency assistance. After one year with PP-LAI, we obtained a spending mean in hospitalization per year and patient of € 635.5 (SD 2033.5) (total of € 45,123.28) and in emergency assistance, € 45.6 (SD 133.4) (total of € 3189.37). These assume a reduction in inpatient spending of 78.4% and 79.3%, respectively (savings of € 175,766.54). Other side, increased spending on antipsychotics 32% (prePP-LAI, mean per patient and year € 4735.4 [SD 3261.8], with total cost of € 317,268; one year postPP-LAI, mean per patient and year € 6597.1 [SD 2256.9], with total cost of € 468,396), which is an increased investment equivalent to € 151,126.92. So that, in evaluating the overall cost savings occurs € 24,740.21 (4.57%).
DiscussionIn psychotic patients, poor adherence is associated with relapse, hospitalization and longer inpatient stays.10 Moreover, some studies show that PP-LAI significantly delayed psychotic relapses during more one year of follow up.11,12 Bressington et al.13 in a similar study as us, with a cohort of 66 patients with a diagnosis of schizophrenia, obtained better results in clinical variables after 12 months of treatment with PP-LAI.
In this study, we have also obtained favorable results to this treatment, but they must be considered carefully. Some limitations that we detected must be considered: little number of the sample, more time of follow up than 12 months or clinical assessments of all patients with standarized scales.
ConclusionsWe suggest that PP-LAI can be an effective therapy for the treatment of patients with psychotic disorders, due to improve symptomatic stability and can prevent hospitalizations with cost-effective symptom control and prevention of relapse in the long term with the consequent economic benefit.
Ethical responsibilitiesProtection of people and animalsThe authors state that for this investigation no human or animal experiments have been performed.
Confidentiality of dataThe authors state that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the correspondence author.
Conflict of interestDr Mesones, Dr Gurillo, Dra Sánchez, Dr Miller and MHS Griñant report no financial relationships with commercial interests.
Please cite this article as: Mesones-Peral JE, Gurillo-Muñoz P, Sánchez-Sicilia MP, Miller A, Griñant-Fernández A. Hospitalizaciones y análisis económico en pacientes psicóticos con palmitato de paliperidona de larga duración. Rev Psiquiatr Salud Ment (Barc). 2017;10:33–37.