Clinical staging is a diagnostic tool used in other medical specialties, which has resulted from the combination of a categorical and dimensional approach. In the last 2 decades, the usefulness of its application in the field of psychiatry has been suggested, mainly as a tool for diagnostic help, and therapeutic and prognostic orientation.
In this paper we review the clinical staging models that have been proposed to date for bipolar disorder, depression and schizophrenia. A literature search was performed in PubMed and Medline databases. A total of 15 studies were selected according to inclusion and exclusion criteria.
Models were grouped according to the type of disorder for which staging was proposed (bipolar disorder: 4, depression: 5, schizophrenia: 6), and their characteristics were described.
As a conclusion, we identify the need to empirically validate these models to demonstrate that staging is a useful tool for clinical practice.
La estadificación clínica es una herramienta diagnóstica utilizada en otras especialidades de la medicina que surge de la combinación de un enfoque categorial y dimensional. En las últimas 2 décadas, se ha planteado su aplicación en el campo de la psiquiatría, fundamentalmente como herramienta de ayuda diagnóstica, de orientación terapéutica y pronóstica. En este trabajo se revisan los modelos de estadificación clínica que han sido propuestos hasta la fecha para el trastorno bipolar, la depresión y la esquizofrenia. Se realizó una búsquedabibliográfica en las bases de datos PubMed y Medline. Se seleccionaron con base en los criterios de inclusión y exclusión un total de 15 estudios. Se describen y comparan las características de cada uno de los modelos agrupados según eltipo de trastorno para el que fueron propuestos (trastorno bipolar: 4; depresión: 5; esquizofrenia: 6).Como conclusión, identificamos la necesidad de validar empíricamente dichos modelos para así demostrar que son una herramienta útil en la práctica clínica habitual.
From the psychiatric and psychological point of view, a categorical focus has dominated in the way to understand and handle mental health problems.1 This perspective assumes that individuals with the same diagnosis are relatively similar and present the same symptoms regardless of the individual's stage of evolution. However, conceptualising mental illness as diverse specific entities is incomplete, given that factors involving great therapeutic and prognostic differences (such as, for example, the number of comorbid diseases, the varying psychopathological profiles or the degree of deterioration in the level of functioning) are not always taken into consideration.2–6 This difficulty can be remedied from a dimensional focus, because it makes it possible to classify subjects throughout a continuum of severity, establishing different levels depending on the signs and symptoms of the disorder, and on the variations produced over time.
Clinical staging models arise from the combination of both approaches. In the first place, the models recognise the attributes that best characterise the subjects, classifying them in terms of all or nothing. In second place, the models quantitatively differentiate such attributes based on different levels of severity. The goal of clinical staging is to divide the course of the illness into recognisable stages that reflect the course of the illness and that are relevant for treatment and prognosis. Using a series of objective, quantifiable markers, the stage of the patient's illness is identified; this in turn makes it possible to: (1) establish the scope of the disorder, (2) emit a prognosis and (3) adopt the most appropriate therapeutic strategy. The final goal is to prevent development to more advanced stages and promote a return to less severe phases or even to complete remission.7 What is more, this tool represents an advancement over conventional diagnostic practice, as it not only defines the extent of the disorder at a specific time, it also reveals its location on the continuum of the course of the illness.7
In short, applying clinical staging might help to achieve precise psychiatry, in which the goals and least harmful and most effective therapeutic actions are adjusted to each person individually.8
Clinical staging in psychiatryThe idea of clinical staging in mental health is not a new concept. Kraepelin, in spite of not using the term itself, was the first to indicate that the course of mental illness seemed to be progressive. Years later, in 1993, Fava and Kellner9 introduced the concept of clinical staging in the psychiatric environment and, since then, a wide range of proposals have appeared (see Tables 1–3).
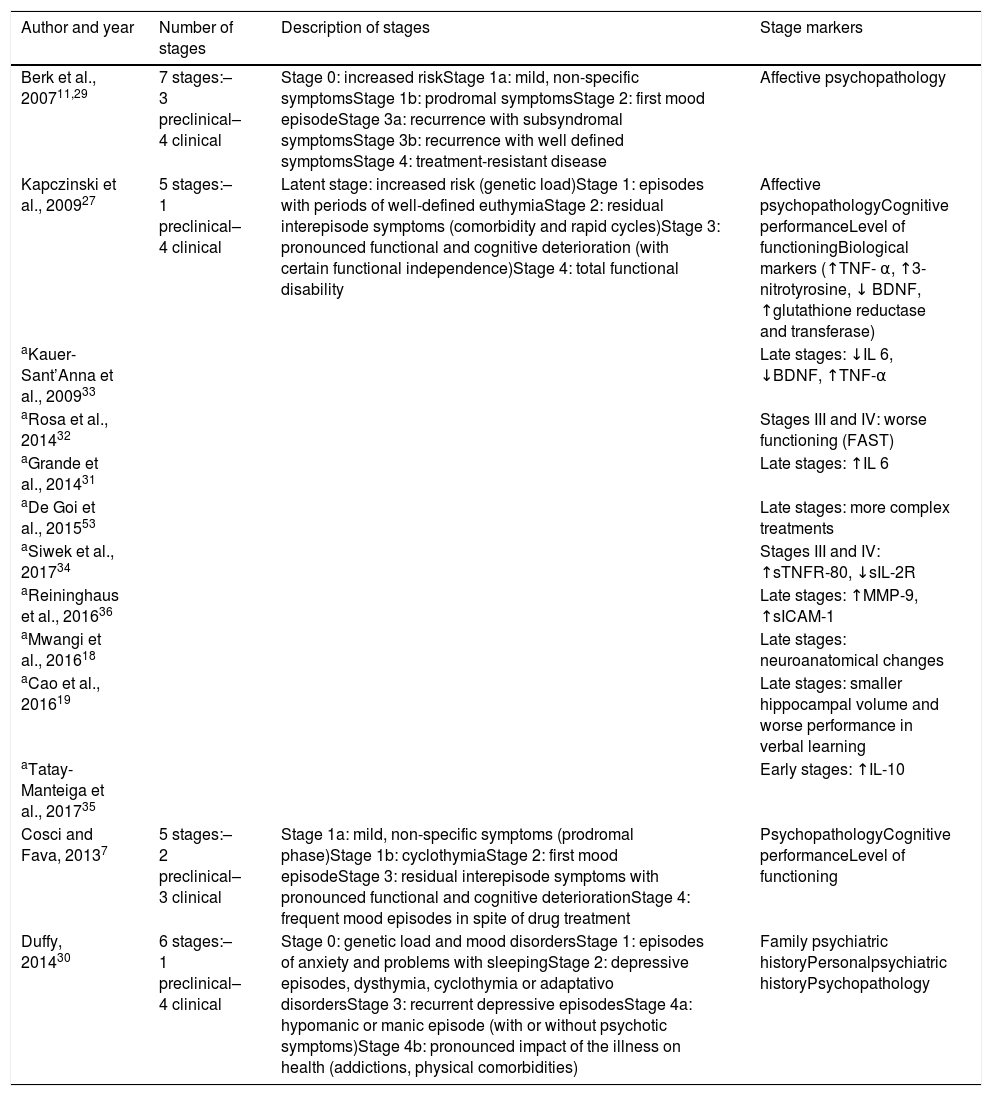
Most significant clinical staging models in bipolar disorder.
| Author and year | Number of stages | Description of stages | Stage markers |
|---|---|---|---|
| Berk et al., 200711,29 | 7 stages:– 3 preclinical– 4 clinical | Stage 0: increased riskStage 1a: mild, non-specific symptomsStage 1b: prodromal symptomsStage 2: first mood episodeStage 3a: recurrence with subsyndromal symptomsStage 3b: recurrence with well defined symptomsStage 4: treatment-resistant disease | Affective psychopathology |
| Kapczinski et al., 200927 | 5 stages:– 1 preclinical– 4 clinical | Latent stage: increased risk (genetic load)Stage 1: episodes with periods of well-defined euthymiaStage 2: residual interepisode symptoms (comorbidity and rapid cycles)Stage 3: pronounced functional and cognitive deterioration (with certain functional independence)Stage 4: total functional disability | Affective psychopathologyCognitive performanceLevel of functioningBiological markers (↑TNF- α, ↑3-nitrotyrosine, ↓ BDNF, ↑glutathione reductase and transferase) |
| aKauer-Sant’Anna et al., 200933 | Late stages: ↓IL 6, ↓BDNF, ↑TNF-α | ||
| aRosa et al., 201432 | Stages III and IV: worse functioning (FAST) | ||
| aGrande et al., 201431 | Late stages: ↑IL 6 | ||
| aDe Goi et al., 201553 | Late stages: more complex treatments | ||
| aSiwek et al., 201734 | Stages III and IV: ↑sTNFR-80, ↓sIL-2R | ||
| aReininghaus et al., 201636 | Late stages: ↑MMP-9, ↑sICAM-1 | ||
| aMwangi et al., 201618 | Late stages: neuroanatomical changes | ||
| aCao et al., 201619 | Late stages: smaller hippocampal volume and worse performance in verbal learning | ||
| aTatay-Manteiga et al., 201735 | Early stages: ↑IL-10 | ||
| Cosci and Fava, 20137 | 5 stages:– 2 preclinical– 3 clinical | Stage 1a: mild, non-specific symptoms (prodromal phase)Stage 1b: cyclothymiaStage 2: first mood episodeStage 3: residual interepisode symptoms with pronounced functional and cognitive deteriorationStage 4: frequent mood episodes in spite of drug treatment | PsychopathologyCognitive performanceLevel of functioning |
| Duffy, 201430 | 6 stages:– 1 preclinical– 4 clinical | Stage 0: genetic load and mood disordersStage 1: episodes of anxiety and problems with sleepingStage 2: depressive episodes, dysthymia, cyclothymia or adaptativo disordersStage 3: recurrent depressive episodesStage 4a: hypomanic or manic episode (with or without psychotic symptoms)Stage 4b: pronounced impact of the illness on health (addictions, physical comorbidities) | Family psychiatric historyPersonalpsychiatric historyPsychopathology |
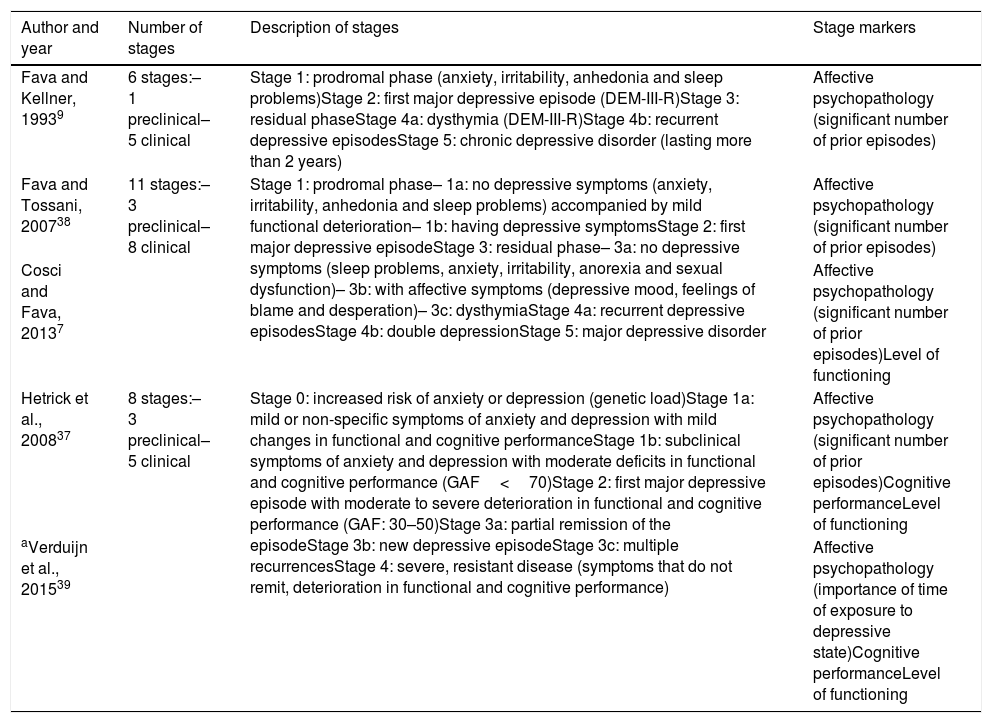
Most significant clinical staging models in unipolar depression.
| Author and year | Number of stages | Description of stages | Stage markers |
|---|---|---|---|
| Fava and Kellner, 19939 | 6 stages:– 1 preclinical– 5 clinical | Stage 1: prodromal phase (anxiety, irritability, anhedonia and sleep problems)Stage 2: first major depressive episode (DEM-III-R)Stage 3: residual phaseStage 4a: dysthymia (DEM-III-R)Stage 4b: recurrent depressive episodesStage 5: chronic depressive disorder (lasting more than 2 years) | Affective psychopathology (significant number of prior episodes) |
| Fava and Tossani, 200738 | 11 stages:– 3 preclinical– 8 clinical | Stage 1: prodromal phase– 1a: no depressive symptoms (anxiety, irritability, anhedonia and sleep problems) accompanied by mild functional deterioration– 1b: having depressive symptomsStage 2: first major depressive episodeStage 3: residual phase– 3a: no depressive symptoms (sleep problems, anxiety, irritability, anorexia and sexual dysfunction)– 3b: with affective symptoms (depressive mood, feelings of blame and desperation)– 3c: dysthymiaStage 4a: recurrent depressive episodesStage 4b: double depressionStage 5: major depressive disorder | Affective psychopathology (significant number of prior episodes) |
| Cosci and Fava, 20137 | Affective psychopathology (significant number of prior episodes)Level of functioning | ||
| Hetrick et al., 200837 | 8 stages:– 3 preclinical– 5 clinical | Stage 0: increased risk of anxiety or depression (genetic load)Stage 1a: mild or non-specific symptoms of anxiety and depression with mild changes in functional and cognitive performanceStage 1b: subclinical symptoms of anxiety and depression with moderate deficits in functional and cognitive performance (GAF<70)Stage 2: first major depressive episode with moderate to severe deterioration in functional and cognitive performance (GAF: 30–50)Stage 3a: partial remission of the episodeStage 3b: new depressive episodeStage 3c: multiple recurrencesStage 4: severe, resistant disease (symptoms that do not remit, deterioration in functional and cognitive performance) | Affective psychopathology (significant number of prior episodes)Cognitive performanceLevel of functioning |
| aVerduijn et al., 201539 | Affective psychopathology (importance of time of exposure to depressive state)Cognitive performanceLevel of functioning |
GAF: Global Assessment of Functioning.
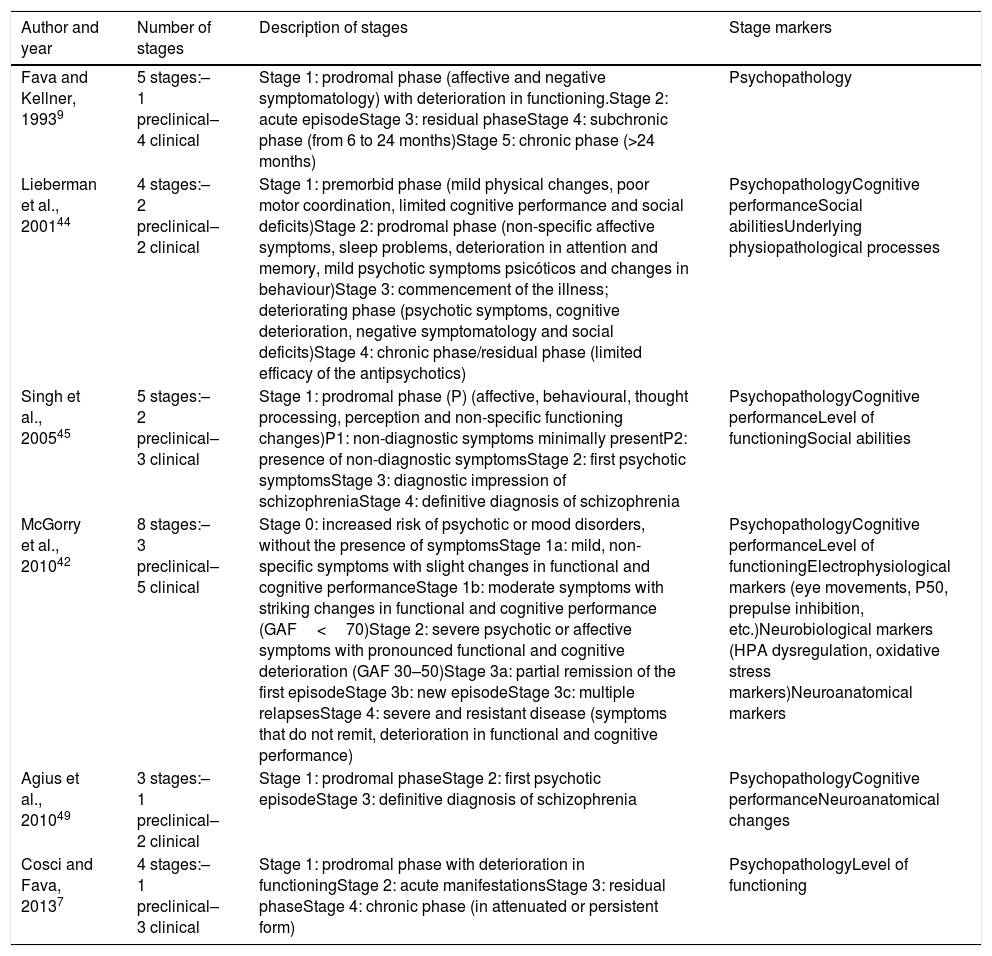
Most significant clinical staging models in schizophrenia.
| Author and year | Number of stages | Description of stages | Stage markers |
|---|---|---|---|
| Fava and Kellner, 19939 | 5 stages:– 1 preclinical– 4 clinical | Stage 1: prodromal phase (affective and negative symptomatology) with deterioration in functioning.Stage 2: acute episodeStage 3: residual phaseStage 4: subchronic phase (from 6 to 24 months)Stage 5: chronic phase (>24 months) | Psychopathology |
| Lieberman et al., 200144 | 4 stages:– 2 preclinical– 2 clinical | Stage 1: premorbid phase (mild physical changes, poor motor coordination, limited cognitive performance and social deficits)Stage 2: prodromal phase (non-specific affective symptoms, sleep problems, deterioration in attention and memory, mild psychotic symptoms psicóticos and changes in behaviour)Stage 3: commencement of the illness; deteriorating phase (psychotic symptoms, cognitive deterioration, negative symptomatology and social deficits)Stage 4: chronic phase/residual phase (limited efficacy of the antipsychotics) | PsychopathologyCognitive performanceSocial abilitiesUnderlying physiopathological processes |
| Singh et al., 200545 | 5 stages:– 2 preclinical– 3 clinical | Stage 1: prodromal phase (P) (affective, behavioural, thought processing, perception and non-specific functioning changes)P1: non-diagnostic symptoms minimally presentP2: presence of non-diagnostic symptomsStage 2: first psychotic symptomsStage 3: diagnostic impression of schizophreniaStage 4: definitive diagnosis of schizophrenia | PsychopathologyCognitive performanceLevel of functioningSocial abilities |
| McGorry et al., 201042 | 8 stages:– 3 preclinical– 5 clinical | Stage 0: increased risk of psychotic or mood disorders, without the presence of symptomsStage 1a: mild, non-specific symptoms with slight changes in functional and cognitive performanceStage 1b: moderate symptoms with striking changes in functional and cognitive performance (GAF<70)Stage 2: severe psychotic or affective symptoms with pronounced functional and cognitive deterioration (GAF 30–50)Stage 3a: partial remission of the first episodeStage 3b: new episodeStage 3c: multiple relapsesStage 4: severe and resistant disease (symptoms that do not remit, deterioration in functional and cognitive performance) | PsychopathologyCognitive performanceLevel of functioningElectrophysiological markers (eye movements, P50, prepulse inhibition, etc.)Neurobiological markers (HPA dysregulation, oxidative stress markers)Neuroanatomical markers |
| Agius et al., 201049 | 3 stages:– 1 preclinical– 2 clinical | Stage 1: prodromal phaseStage 2: first psychotic episodeStage 3: definitive diagnosis of schizophrenia | PsychopathologyCognitive performanceNeuroanatomical changes |
| Cosci and Fava, 20137 | 4 stages:– 1 preclinical– 3 clinical | Stage 1: prodromal phase with deterioration in functioningStage 2: acute manifestationsStage 3: residual phaseStage 4: chronic phase (in attenuated or persistent form) | PsychopathologyLevel of functioning |
GAF: Global Assessment of Functioning; HPA: hypothalamus-pituitary-adrenal axis.
One of the features that a disorder has to have to benefit from a clinical model of stage involves possessing a predictable clinical course over time.10 The initial stages are more benign and tend to respond to simpler therapies. In contrast, the more advanced stages require therapeutic tools of greater risk; that is, with a greater capacity to produce long-term adverse effects or physical alterations, as well as needing palliative strategies focused on the consequences and disabilities produced by the illness.11 Various authors1,12,13 have supported the hypothesis that the natural course of severe mental illness develops from an asymptomatic state (at risk) towards non-specific symptom manifestations, such as mild anxiety and subthreshold and somatic symptoms, which can finally lead to a specific mental disorder mental. Likewise, numerous studies have shown that the patterns of response to treatment vary depending on the developmental stage in which the therapy is carried out.4,5,12,14
The models formulated up to now are interesting. However, they are exclusively theoretical proposals. From now on, efforts should be aimed at their empirical validation. In addition, these models approach the reality of mental illness only partially, given that they do not contemplate all the variables that can be relevant over the course of the illness; examples are the patient's physical health,15,16 health-related quality of life17 or neuroanatomical markers.18,19
MethodWe present a selective review of clinical staging in severe mental illness, specifically in bipolar disorder (BD), depression and schizophrenia. A general search of the PubMed databases was performed with the following search strategy: ((staging[Other Term]) AND (schizophrenia[Mesh Terms] OR bipolar disorder[Mesh Terms] OR depression[Mesh Terms])). In order to find other relevant references, the bibliography of the articles selected was performed. Next, we screened the results to select studies based on the following inclusion criteria: (1) studies whose study objective was the proposal of a clinical staging model for BD, depression or schizophrenia, (2) ones that clearly described the different stages proposed, and (3) those written in English or Spanish.
ResultsFrom the electronic search, a total of 35 articles were obtained and from the manual search, a total of 20. Applying the inclusion criteria, only 15 articles precisely described a staging model for each of the disorders studied; the others either did not described a model or referred to previous models.
Clinical staging in bipolar disorderOver the last two decades, experts have considered that the etiopathogenesis of BD involves the presence of an active neurodevelopmental process that, at least partially, is mediated by inflammatory processes, oxidative stress, apoptosis and alterations in neurogenesis.20–22 These features make it an ideal disorder to benefit from a clinical staging model.20
Likewise, clinical evidence supports its development from prodromal (preclinical) stages towards more severe, treatment-resistant stages.23 An example of this would be the decrease in euthymia time, the increase in frequency and severity of episodes, the greater risk of recurrence and the increase in sensitivity to stress factors over time.24 Patients who have experienced 10 or more episodes more frequently present inability to work, worse level of functioning and poor quality of life, in addition to more severe, more persistent symptoms. The concept of allostatic load, which refers to the physiological mechanisms of adaptation to stress, would make it possible to integrate these findings.25–27 In addition, studies examining response to treatment reveal that both the psychological treatments and the pharmacological treatments are more effective if they are implemented in the initial stages.14,28
In the last few years, different theoretical clinical staging models for BD have been proposed (see Table 1). The first one, developed by Berk et al.,29 consists of 7 stages centred around variables of psychopathology in affective disorders. It begins with an asymptomatic period, in which factors of risk are mainly identified (Stage 0, of increased risk), after which the patient can either advance towards Stage 1a (presence of mild, non-specific symptoms) or directly towards Stage 1b (manifestation of prodromal symptoms). After that, the first affective episode may present (Stage 2, the first episode of mood disorder). Stage 3 (recurrence) is classified based on the number and type of episodes: Stage 3a (recurrence with symptoms of sub-syndromal mood disorders); Stage 3b (recurrence with well defined symptoms) and Stage 3c (multiple recurrences). Finally, in Stage 4 (treatment-resistant disease), the authors describe a patients whose clinical development is characterised by symptoms that are persistent and resistant to treatment. Years later, these authors proposed the most appropriate therapeutic strategies for each of the different stages.11
In 2009, Kapczinski et al.,27 posed a second, 5-stage, model that incorporated cognitive, functional and biological marker variables besides including affective psychopathology. It established a different prognosis and treatment for each stage. The model has 4 stages: a preclinical one (Stage 0, latent) and 3 clinical ones. Stage 1 is characterised by the presence of mood episodes separated by clear periods of euthymia. Next, in Stage 2, these euthymic periods become contaminated by residual symptoms. In Stage 3, there is a pronounced cognitive and functional deterioration, whose worsening leads to Stage 4; that is, to the presence of complete functional incapacity. Years later, in 2013, Cosci and Fava7 developed a 4-stage model similar to that of their predecessors, but eliminating the preclinical stage because they considered that the prodromal manifestations were highly non-specific and did not make it possible to discriminate among the different types of disorders. In contrast, Duffy et al.,30 keeping in mind BD's elevated heritability, again included a preclinical stage defined solely by the presence of confirmed family BD history; they considered the descendents of these patients to be a high-risk group. Their model, in addition to incorporating this preclinical stage, distinguished between 2 subgroups of patients: those that progressed to a classic BD and the ones that developed a bipolar spectrum disorder (patients with mixed or psychotic symptoms). Their model is made up of 6 stages and establishes different clinical markers depending on the subgroup to which the patient belongs.30
Without arriving at the proposal of a specific model, several authors have identified potentially useful variables to classify patients with BD according to severity, such as level of functioning31,32 and biological markers.31,33–36 Specifically, alterations have been observed in several inflammatory parameters in the late stages (III–IV) of BD: interleukins 1 (sIL-2R),34 6 (IL-6)31,33 and 10 (IL-10)35; soluble tumour necrosis factor receptor 80 (sTNFR-80)34; brain-derived neurotrophic factor (BDNF)33; matrix metalloproteinase MMP-936 and soluble intercellular adhesion molecule 1 (sICAM-1)36 (see Table 1 for further information).
Likewise, Mwngi et al.,18 found neuroanatomical differences between patients in early, intermediate and late stages. Patients in more advanced stages presented greater brain structure alterations, which gives support to the hypothesis of neurodevelopment in BD and the usefulness of staging models. In a neuroimaging study, Cao et al.,19 found that late-stage patients had a smaller hippocampal volume and greater difficulties in verbal learning than control subjects. These studies indicate that neuroanatomical alterations seem to be potential markers for clinical staging of BD.
Clinical staging in depressionClinical staging models have been developed for major depression with 2 different aims: classify the progression of the illness and resistance to treatment. In this review, we will focus on the first (see Table 2), given that the second are limited to resistant depressions.
With these models, it is understood that applying a staging model in depression could make it possible to delay or prevent disease onset, as well as increase the number of individuals treated appropriately, reduce the severity of the disorder or prevent its development.6,37
Fava and Kellner9 developed the first clinical staging model for unipolar depression, which was later updated in 2007.38 This model has 6 stages and is based on affective symptomatology and the number of episodes. According to these authors, depression begins with a prodromal phase characterised by the presence of risk factors without depressive symptoms (Stage 1a) or by subdepressive symptoms that do not reach the severity of an episode (Stage 1b). From that point on, individuals can present the first depressive episode (Stage 2). Next comes the residual phase (Stage 3), which may consist of an asymptomatic period (Stage 3a) or of a stage in which the diagnostic criteria for dysthymic disorder are fulfilled (Stage 3b). Stage 4 is characterised by the presence of multiple recurrences (Stage 4a) and, if dysthymia has been present, the diagnosis of double depression is proposed (Stage 4b). Lastly, Stage 5 is reached when there are no remission periods and the depressive episode lasts more than 2 years. In 2013, a new version7 was put forward, in which the level of functioning was added as a variable that determined the step between stages. The residual phase was also divided into 3 stages: (1) non-affective symptoms such as sleep problems, anxiety or sexual dysfunction, (2) dysthymia and (3) depressive symptoms.
In 2008, Hetrick et al.,37 proposed an adaptation of the McGorry12 model for psychotic and mood disorders. This model consists of 8 stages and takes into consideration changes in the patient's cognitive performance and level of functioning. The first 3 are preclinical stages, while the characteristic symptoms of a major depressive disorder develop over the next 5 (Stage 2: first depressive episode; Stage 3a: partial remission of the first depressive episode; Stage 3b: recurrence; Stage 3c: multiple recurrences and Stage 4: severe and persistent major depressive disorder determined by the severity of the psychopathology and its strong repercussion on cognition and functioning). Verduijn et al.,39 examined the predictive validity of the staging model proposed by Hetrick.37 Their investigation showed that using a staging model based on purely clinical stages is reasonable for major depressive disorder. However, and in contrast to what was thought, the time of exposure to the depressive state seemed to characterise the clinical stages better than the number of previous depressive episodes.
As for physiological parameters, no investigations identifying biomarkers capable of distinguishing between disease progression stages were found.40 For that matter, the physiopathological mechanisms involved in the aetiology of depression have not been found to be linked to its clinical progression.41
Clinical staging in schizophreniaSchizophrenia is a complex mental disorder mental with long evolution, whose symptoms generally emerge during adolescence and early adulthood. Our current classification systems lack diagnostic validity, especially in the first phases, when symptoms are still appearing and have not become sufficiently developed to fit the existing syndromic criteria. This is mainly due to the difficulty in distinguishing between the transitory or normative changes stemming from neurodevelopment, and changes that precede the development of a mental disorder.42 Creating staging models that allow the incorporation of prodromal stages together with therapeutic strategies adapted would make it possible to reduce the degree of deterioration associated with the disorder. Such models would also prevent progression to more advanced stages.
The bases for applying clinical staging models in schizophrenia started from the agreement between the neuroanatomical brain studies (grey matter changes) described by Pantelis et al.,43 and the clinical-based studies by McGorry et al.12 The first theoretical staging model for schizophrenia was proposed by Fava and Kellner9 (see Table 3). This model has 5 stages based solely on psychopathology. The stages are as follows: Stage 1, prodromal symptoms (mainly affective and negative) with limitations of functioning; Stage 2, acute episode; Stage 3, residual symptoms; Stage 4, subchronic symptoms (lasting from 6 to 24 months); and Stage 5, chronic symptoms (lasting longer than years). In 2001, Lieberman et al.44 proposed a new 4-stage model that included biological markers and indications of cognitive and social functioning, in addition to psychopathological variables. In 2005, Singh et al.45 proposed 5 stages in the development of schizophrenia: prodromal phases (P1: non-diagnostic symptoms minimally present; P2: presence of diagnostic symptoms), first psychotic symptoms, diagnostic impression of schizophrenia and chronic stage (definitive diagnosis). Earlier, Cannon et al.46 had described a premorbid stage, occurring before the prodromal phases, in which signs of neurodevelopmental delay could be seen, seeming to indicate an increase in the risk of developing schizophrenia in the future. Years later, McGorry et al.4 developed an 8-stage model whose main innovation was including electrophysiological, neurobiological and neuroimaging markers. After many modifications,47,48 the final model consisted of the following stages: Stage 0, increased risk of psychotic disorder without the presence of symptoms; Stage 1a, presence of non-specific or mild symptoms; Stage 1b, moderate subsyndromal symptoms; Stage 2, onset of the first psychotic episode; Stage 3a, partial remission of the first episode; Stage 3b, recurrence or relapse of the psychotic disorder; Stage 3c, multiple recurrences of greater clinical severity and impact of the disease; and Stage 4, severe and persistent disease. In 2010, Agius et al.49 proposed a 3-stage model based on the cognitive, neuroanatomical and clinical impact of the disease. Finally, Cosci and Fava7 posited a model that integrated the previous proposals, consisting of 4 stages: (1) prodromal symptoms with deterioration of functioning; (2) acute manifestations; (3) residual phase; and (4) chronic phase (either attenuated or persistent).
Over the last few years, there have been several studies demonstrating the usefulness of a focus based on clinical staging for schizophrenia. To begin with, in 2016 a study showed that the variations in cell adherence (particularly the sICAM-1 molecule) reflected a biochemical staging model in schizophrenia.50 In addition, Dragioti et al.51 examined the differences in 3 groups of patients with a diagnosis of schizophrenia (classified according to age) on the Positive and Negative Syndrome Scale for schizophrenia. The study results indicated that the course of schizophrenia seemed to reflect a process ranging from coherent mental functioning with consciousness of disease, through disorganisation to, finally, neurocognitive deterioration. Another recent study52 has shown that individuals with a single episode of schizophrenia present less severe scores on the positive, disorganised and hostility factor dimensions than those who have undergone more than one episode. These findings provide empiric support (partial validations) to the idea of staging in schizophrenia. However, further studies that determine specific clinical and biological markers for each stage are needed, as well as others that take the multidimensional nature of the disorder into consideration.
DiscussionOver the last 2 decades, the staging models in severe mental illness (specifically, in BD, depression and schizophrenia) have been evolving and progressing due to the clinical need to stage the patients in order to bring us closer to precision medicine.
This article presents the results of a selective review of the staging models for severe mental illness proposed up until now. It is necessary to point out that, in spite of the models available, none of them have had their validity shown empirically.
In relation to BD, there were 4 models developed towards the end of the first decade in the 21st century: the model proposed by Kapczinski et al.27 is the one that has evolved and progressed the most. For example, Rosa et al.32 classified 54 patients according to Kapczinski's model. They used a semi-structured interview and chose as the bases the course of the illness, the presence of comorbid illnesses and the level of functioning (work, social relationships and self-care). Study results showed evidence in favour of clinical staging in BD, given that the patients in initial stages demonstrated better functioning than those in later stages. Following the same methodology, De Goi et al.53 showed that patients in early stages required simpler pharmacological strategies than those classified in more advanced stages. Lastly, there is another study in which low levels of sIL-2R and high levels of sTNFR-80 in serum are characteristic of late stages.34 In spite of the fact that it might seem that these studies validate the model proposed by Kapczinski, they only do so partially: some are based on functioning, others on treatment and yet others on some specific biomarkers. The rest of the studies found were limited to identifying variables that discriminated between early and late stages, without even proposing any specific staging model.18,19,31,33,36
With respect to unipolar depression, 3 staging models have been proposed. All of them clearly define a prodromal phase, but there are differences as to the number of preclinical stages that make it up. The only model validated empirically is that developed by Hetrick et al.37 Their research demonstrated the predictive validity of clinical staging models for depression. In addition, these authors found that how long the episodes lasted had greater predictive power than the number of previous episodes.
As for clinical staging models for schizophrenia, we have found 6 theoretical proposals. The last one, from Cosci and Fava,7 integrated all the previous proposals and set out 4 stages: prodromal, acute manifestations, residual and chronic phase. The rest of the studies on patients with this diagnosis are based on dividing the sample according to years of evolution and finding markers that distinguish between early and late stages; however, they do not validate the staging models proposed to date.
Future studies must carry out longitudinal research and establish the predictive value of the clinical staging models for the different disorders mentioned. The goals should include improving diagnostic capability and making it more precise: from the initial stages of the illness, with the need for early detection, to the more advanced stages, with the need to identify resulting complications and deficits (psychiatric and somatic comorbidities, and losses in the level of functioning and in quality of life). An additional objective should be to encourage the application of interventions adapted to patient needs according to the stage in which the individuals are found.
ConclusionsFrom what has been indicated, we can conclude that the clinical staging models traditionally used by other medical specialities might also be applicable to mental and behavioural illnesses. Specifically, various theoretical staging models have been established for BD, depression and schizophrenia in the last decade. However, empirical validity has been shown for only one of those developed for depression. For these reasons, and in spite of all the effort carried out to date, it remains essential to validate the models developed up until now or to create new empirical staging models whose validity has been demonstrated for routine clinical practice.
FundingLorena de la Fuente-Tomás has a contract under the Severo Ochoa Predoctoral Aid Programme for research and teaching in the Principado de Asturias.
This study was funded by the Ministry of Economy and Competitiveness, the Carlos III Healthcare Institute (PI14/02037 and PI16/01761) and the European Regional Development Fund (ERDF).
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: de la Fuente-Tomas L, Sánchez-Autet M, García-Álvarez L, González-Blanco L, Velasco Á, Sáiz Martínez PA, et al. Estadificación clínica en los trastornos mentales graves: trastorno bipolar, depresión y esquizofrenia. Rev Psiquiatr Salud Ment (Barc.). 2019;12:106–115.