The study of administrative prevalence from cumulative psychiatric case registers allows the mental health state of the studied region and the functioning of its Health Services to be estimated.
MethodsData were extracted from the Asturias Cumulative Psychiatric Case Register (RACPAS) between January 1st 1998 and December 3rd 2010. Characteristics of the population of the catchment area were studied, and their relationship with the administrative prevalence was analysed.
ResultsThe mean population in the studied period was 1,078,406 inhabitants. The Fritz index and the Youth and replacement indices of the active population decreased throughout the period. There was no significant increase in the prevalence of organic mental disorders, psychosis, mood disorders, and substance use in males, or behavioural disorders associated with somatic factors and physiological dysfunctions in females. There were significant gender differences in the prevalence of all disorders, except for personality disorders and organic mental disorders. Population ageing had a significant influence on the increase in the prevalence of most mental disorders in both males and females.
ConclusionsA slight general increase in the administrative prevalence of mental disorders is observed during the studied period, and it was influenced by population ageing.
El estudio de la prevalencia administrativa a partir de los Registros Acumulativos de Casos Psiquiátricos permite tener una estimación de la salud mental de la población de una zona y del funcionamiento de sus servicios sanitarios.
MétodosAnálisis de los datos del Registro Acumulativo de Casos Psiquiátricos de Asturias (RACPAS) entre el 1-1-1998 y el 3-12-2010. Estudio de las características de la población de referencia y análisis de la asociación de los índices sociodemográficos con la prevalencia de la enfermedad mental.
ResultadosLa población media en los años estudiados fue de 1.078.406 con disminución de los índices de juventud, de Fritz y de reemplazo de la población activa. Se observó un leve incremento de la prevalencia de la mayoría de los trastornos mentales registrados en el RACPAS. No se observó un incremento significativo en la prevalencia de los trastornos mentales orgánicos, psicosis, trastornos del humor, consumo de sustancias no alcohólicas en los hombres ni en los trastornos del comportamiento asociados a disfunciones fisiológicas y a factores somáticos en las mujeres. Hubo diferencias significativas entre los sexos en la prevalencia de todos los trastornos excepto en los trastornos de la personalidad y los trastornos orgánicos cerebrales. El envejecimiento poblacional tuvo una influencia significativa en el incremento de la prevalencia de la mayoría de los trastornos mentales tanto en hombres como en mujeres.
ConclusionesDurante el periodo estudiado se observó un leve incremento general de la prevalencia administrativa influida por el envejecimiento poblacional.
Mental Health in the National Health System is a document in which the Health Ministry of Spain proposes the objectives for mental heath for the 2009–2013 period. Its strategy includes a specific line on Information and Assessment Systems whose general objective is to improve knowledge on the mental health of the population and the attention given by the National Health System.1
Among the epidemiological indexes, prevalence during a period (usually annual prevalence) is the most useful measure for ascertaining the total disease load and its health care impact on services for episodes of such variable length as those of mental health.2,3 The patients that contact the services (administrative morbidity) represent a valid data source for disease evolution.3,4 The more defined and limited the geographical area is, and the more complete and structured the information gathering system is, the more reliable this data is.
Cumulative psychiatric case registers (CPCR) are defined as databases in which the various contacts with a specific set of mental5 health establishments of the individuals comprising the population of a specific geographical area are registered longitudinally.6 These CPCR databases focus on cases (individuals) and store the information about the people in contact with the services and the activities carried out. They are cumulative because they add each individual's information each time there is a contact with the services.7 The geographical base defined makes it possible to obtain rates and develop assessments of an epidemiological nature.
The CPCR possess a series of limitations. They gather information on specialised services, omitting people attended in primary care. They also depend on the nature and structure of the services and on the characteristics of the reference population, so phenomena such as migrations may affect the data to an unknown degree. Another specific limitation of our study is the impossibility of analysing the data by age.
The CPCR for the Principado de Asturias [NT: an autonomous community in northern Spain] (RACPAS in Spanish) began to function on 1 January 1986. It gathers information on all the contacts, both in hospital and at out-patient clinics, with all the public psychiatric service establishments in Asturias, including addiction service.8
The objective of this study was, based on analysing the RACPAS data, to investigate the development of administrative prevalence rates in the mental health services in Asturias between 1998 and 2010.
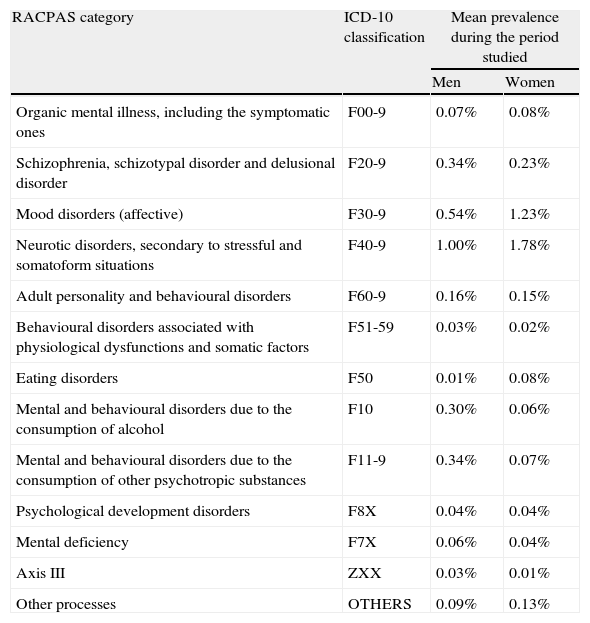
Materials and methodsFor the period from 1 January 1998 to 31 December 2010, the RACPAS data about subjects that established contact with any service establishment of the Mental Health Services in Asturias were analysed. We used the “rate of annual administrative prevalence rate or annual treated prevalence” (subjects that were in contact with the mental health services at the beginning of each year, plus those that established contact for the first time throughout the year) for the temporal analysis of the data. In Table 1, the taxonomy utilised by the RACPAS is presented, as well as its correspondence with the diagnostic categories of the International Classification of Diseases (ICD-10).
Mental disorders studied (according to the taxonomy used in the RACPAS), together with the International Classification of Diseases (ICD-10) code for each type of disorder.
| RACPAS category | ICD-10 classification | Mean prevalence during the period studied | |
| Men | Women | ||
| Organic mental illness, including the symptomatic ones | F00-9 | 0.07% | 0.08% |
| Schizophrenia, schizotypal disorder and delusional disorder | F20-9 | 0.34% | 0.23% |
| Mood disorders (affective) | F30-9 | 0.54% | 1.23% |
| Neurotic disorders, secondary to stressful and somatoform situations | F40-9 | 1.00% | 1.78% |
| Adult personality and behavioural disorders | F60-9 | 0.16% | 0.15% |
| Behavioural disorders associated with physiological dysfunctions and somatic factors | F51-59 | 0.03% | 0.02% |
| Eating disorders | F50 | 0.01% | 0.08% |
| Mental and behavioural disorders due to the consumption of alcohol | F10 | 0.30% | 0.06% |
| Mental and behavioural disorders due to the consumption of other psychotropic substances | F11-9 | 0.34% | 0.07% |
| Psychological development disorders | F8X | 0.04% | 0.04% |
| Mental deficiency | F7X | 0.06% | 0.04% |
| Axis III | ZXX | 0.03% | 0.01% |
| Other processes | OTHERS | 0.09% | 0.13% |
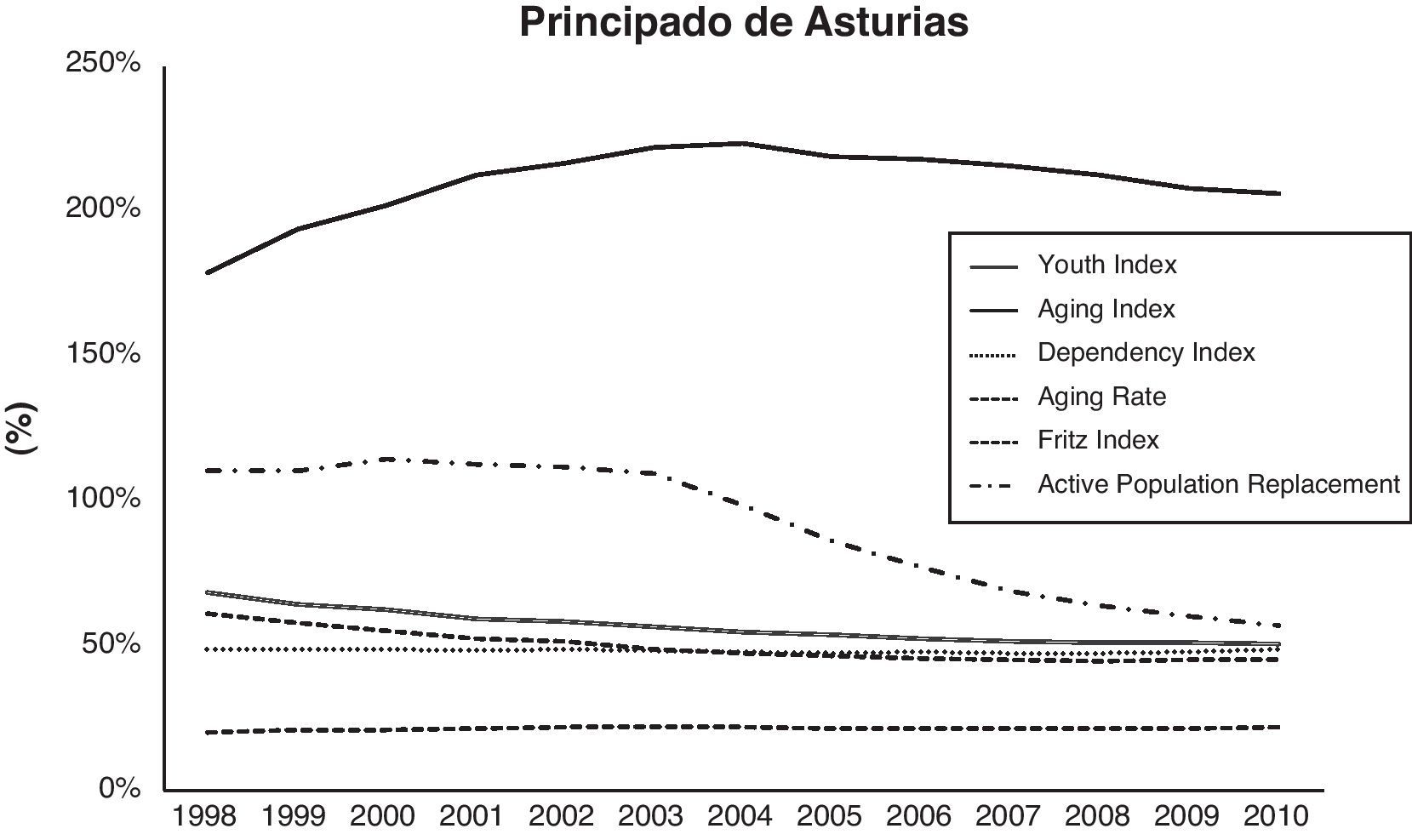
Population data were obtained from the official records of the municipal register of inhabitants for each year included in the interval studied. This information, obtained annually since 1998, was extracted from the National Statistics Institute database. The following population indicators were calculated: (a) Youth Index: the percent of the population younger than 20 in relation to that 60 years or older; (b) Ageing Index: percent of the population older than 64 years against the group of those younger than 16; (c) Dependency Index: the population older than 64 and younger than 16 against the group composed of those between those two ages; (d) Ageing Rate: proportion of the population aged 65 or older against the total population; (e) Fritz Index: percent of population aged less than 20 years, with respect to the group of population aged between 30 and 49 years; and (f) Active Population Replacement Index: ratio of individuals between 15 and 19 years old and the population aged between 60 and 64 years. These indexes show the natural population increase and provide an estimate of the dependent individuals and of the evolution of the active population.
For the analysis of tendencies, the Cox–Stuart test9 was applied in the demographic indexes and in the administrative prevalence rates for the different disorders. The Mann–Whitney test10 was also used to test the existence of statistically significant differences in the median values for the disease prevalence rates. Finally, to study how population ageing related to the passage of time using the administrative prevalence for the diseases, multi-variant models of regression11 were used with the administrative prevalence of each of the disorders as the independent variable. The 2 dependent variables used were the year (passage of time) and ageing rate.
ResultsThe mean population of the study area (Asturias) during the period assessed was 1,078,406 inhabitants (52.03% women). In 1998 the population structure already presented signs of ageing, which increased during the time studied. Fig. 1 shows the evolution of the demographic indicators. Upon applying the Cox-Stuart test, we could see a progressively significant reduction in the youth (P=.0156), Fritz (P=.0156) and active population replacement (P=.0156) indexes.
For men, administrative prevalence increased with statistical significance in the following: neurotic disorders, secondary to somatoform and stressful situations (P=.0156); behavioural disorders associated with physiological dysfunctions and with somatic effects (P=.0156); mental and behavioural disorders due to alcohol consumption (P=.0156); psychological development disorders (P=.0312); mental retardation (P=.0312); and Axis III (P=.0156). For women, the significant increases were found in the following: organic mental disorders, including the symptomatic (P=.0156); schizophrenia, schizotypal disorder and delusional disorder (P=.0156); mood disorders (affective) (P=.0156); neurotic disorders secondary to somatoform and stressful situations (P=.0156); adult personality and behavioural disorders (P=.0156); alcohol-related mental and behavioural disorders (P=.0156); mental and behavioural disorders due to consumption of other psychotropic substances (P=.0312); mental retardation (P=.0156); and Axis III (P=.0156). No tendency to decrease was seen in the administrative prevalence of any disorders.
Comparing the prevalence figures for men and women with the Mann–Whitney test revealed statistically significant differences. Men showed a significantly higher prevalence in schizophrenia, schizotypal disorder and delusional disorder (P=.0001), behavioural disorders associated with physiological dysfunctions and with somatic effects (P=.004), alcohol-related mental and behavioural disorders (P=.0001), mental and behavioural disorders due to consumption of other psychotropic substances (P=.001) and mental retardation (P=.001). Women presented higher prevalence in mood disorders (P=.0001), neurotic disorders secondary to somatoform and stressful situations (P=.0001), eating disorders (P=.00001) and Axis III (P=.02). There were no significant differences in the prevalence for psychological development disorders (P=.019), adult personality and behavioural disorders (P=.096) and organic mental disorders, including the symptomatic (P=.369).
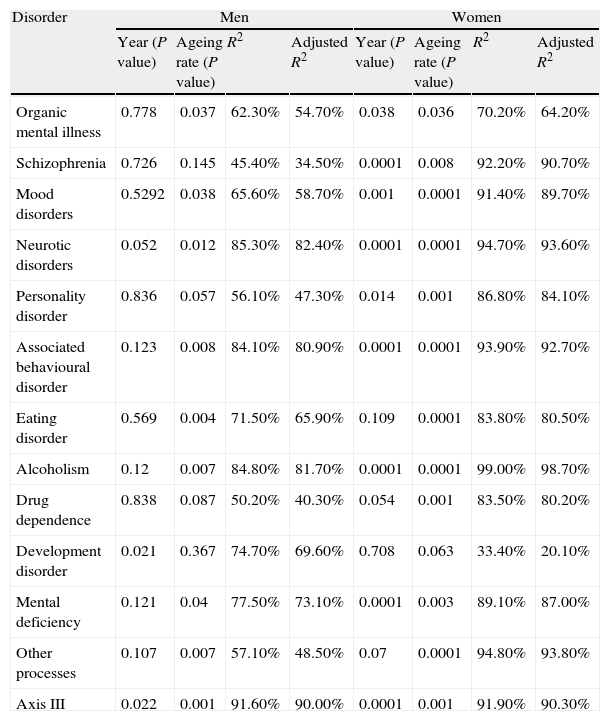
Finally, we wanted to study the simultaneous influence of the population ageing rate and the time variable on the disorder administrative prevalences. We consequently calculated (for each of them and for each gender separately) a set of lineal regression models that linked the independent variable administrative prevalence rate for each of the disorders againt the dependent variables year (passage of time) and ageing rate.
The results presented in Table 2 show that the ageing rate was a statistically significant variable for a level α of 5% in almost all the models mentioned. The only exceptions were men in the administrative prevalence of “schizophrenia, schizotypal disorder and delusional disorders”, “adult personality and behavioural disorders”, “mental and behavioural disorders due to consumption of other psychotropic substances” and “psychological development disorders”. In the case of the women, there was a significant influence for all the diseases except for “developmental disorders”. The passage of time was significant in only the men for the developmental and Axis III disorders. However, in women, it was significant for all the disorders with the exception of eating disorders, mental and behavioural disorders due to consumption of other psychotropic substances, and other processes.
Result of the lineal regression models with the administrative prevalence of each of the disorders as the independent variable and the time (year variable) and rate of population ageing as the dependent variables.
| Disorder | Men | Women | ||||||
| Year (P value) | Ageing rate (P value) | R2 | Adjusted R2 | Year (P value) | Ageing rate (P value) | R2 | Adjusted R2 | |
| Organic mental illness | 0.778 | 0.037 | 62.30% | 54.70% | 0.038 | 0.036 | 70.20% | 64.20% |
| Schizophrenia | 0.726 | 0.145 | 45.40% | 34.50% | 0.0001 | 0.008 | 92.20% | 90.70% |
| Mood disorders | 0.5292 | 0.038 | 65.60% | 58.70% | 0.001 | 0.0001 | 91.40% | 89.70% |
| Neurotic disorders | 0.052 | 0.012 | 85.30% | 82.40% | 0.0001 | 0.0001 | 94.70% | 93.60% |
| Personality disorder | 0.836 | 0.057 | 56.10% | 47.30% | 0.014 | 0.001 | 86.80% | 84.10% |
| Associated behavioural disorder | 0.123 | 0.008 | 84.10% | 80.90% | 0.0001 | 0.0001 | 93.90% | 92.70% |
| Eating disorder | 0.569 | 0.004 | 71.50% | 65.90% | 0.109 | 0.0001 | 83.80% | 80.50% |
| Alcoholism | 0.12 | 0.007 | 84.80% | 81.70% | 0.0001 | 0.0001 | 99.00% | 98.70% |
| Drug dependence | 0.838 | 0.087 | 50.20% | 40.30% | 0.054 | 0.001 | 83.50% | 80.20% |
| Development disorder | 0.021 | 0.367 | 74.70% | 69.60% | 0.708 | 0.063 | 33.40% | 20.10% |
| Mental deficiency | 0.121 | 0.04 | 77.50% | 73.10% | 0.0001 | 0.003 | 89.10% | 87.00% |
| Other processes | 0.107 | 0.007 | 57.10% | 48.50% | 0.07 | 0.0001 | 94.80% | 93.80% |
| Axis III | 0.022 | 0.001 | 91.60% | 90.00% | 0.0001 | 0.001 | 91.90% | 90.30% |
Synthetically, the socio-demographical situation of the population at the beginning of the study and the progressive decrease in the Fritz and youth indexes12 define an aged territory, with difficulties for replacing the active population and with an “a priori” increase in the number of dependent individuals.
Comparing our data with the annual prevalence data collected in the general European population (ESEMED study), the Mental Health Services in Asturias are estimated to take care of approximately 1/4th of the mental disease existing in the community: 24.7% of mood disorders, 28% of anxiety disorders and 22% of the alcohol-related problems.13 The Asturias data coincide, fairly precisely, with this study cited with respect to morbidity treated. This is true overall (25% of the people in the general population that had a mental disorder in the last 12 months consulted a mental health service), as well as broken down by diagnostic groups. The ESEMED data show that 36% of the mood disorder cases (30% of cases with severe mental disorder) and 26% of the anxiety disorders are treated in mental health services,14–16 with the proportion of those that come to these services varying based on the pathology present and the socio-demographic patient characteristics (age, gender and marital status).17 In our environment, consequently, considerable mental health needs would go without coverage, specifically in that less than 1/3 of the individuals that suffer a mental disorder in the course of a year receive some type of specialised treatment.18 The exception is in the psychotic disorders, in which the prevalence treated is closed to the true prevalence in the general population, estimated to be 3 per 1000 inhabitants in men and 2.86 per 1000 in women.19
In the general Spanish population, the most prevalent mental disorder was major depressive disorder, with an annual prevalence of 3.9%. Other highly prevalent disorders were specific phobia, alcohol abuse disorder and dysthymia.15 In our study, the anxiety disorders presented a greater prevalence treated than did the affective disorders; this may be due to the limitations of the register. The RACPAS does not specifically include adaptation disorders (whose prevalence can reach 2.9%) among its diagnostic categories. These disorders, located between absence of mental disorder and affective disorders, can be responsible for the variations between our data and those of mental disorder prevalence studies in the general population, which normally use instruments to detect cases that make it possible to obtain a more detailed diagnostic categorisation.20
As for the differences by sex, predictable results were obtained. There were higher administrative prevalence rates for women in mood, anxiety and somatisation disorders, while the higher rates were in disorders from substance abuse in the men.21
The general tendency towards prevalence increase in most diagnostic groups during the period was not, however, homogeneous. There were differences in man and female tendencies and among diagnostic groups. In the case of the “factors influencing health status and health services contact” (Axis III), prevalence increased notably during the first years of the period analysed and then remained stable. A modification in the diagnostic habits of the mental health professionals or in the referral habits of the Primary Health Care physicians might be one explanation. The same phenomenon (sharp increase in the first years, with tendency to stabilise after 2004) can be seen clearly in the most prevalent disorders (anxiety and mood disorders) and, in a less pronounced way, in the less prevalent ones. The RACPAS began functioning in 1986 and, at the beginning of the period studied, the psychiatric healthcare network in Asturias was already significantly developed. Bearing these facts in mind, the hypothesis seems implausible that the early increase could reflect the time taken for initial registration and accumulation of new chronic and recurrent processes.3
The proportional decrease in the rise in mood disorders in the final years of the period has been found in other studies. They showed rapid increases in affective disorder treatment in the decade from 1987 and 1997; these increases coincided with the development of new antidepressants and better depression diagnosis techniques in primary care, as well as with more modest increases in the previous decade, linked to a change towards biological understanding of depression and a consequent decrease in psychotherapeutic treatments.22–24 These are arguments that could also be used for anxiety disorders.
The RACPAS classification system involves problems derived from excessively general diagnostic categories. Studying the mood disorder tendencies over wide periods (15 years), non-associated prevalence increases have been found: increases not associated with the rise in major depression prevalence (not modified during the period); with the proportion of individuals indicating that their lives were extremely stressful (which decreased); with changes in the proportion of individuals that reported poor mental health. That is to say, although there were no changes in the measurements based on symptom assessment and the perception of extreme stress even decreased, diagnoses and treatments rose. These data lend no support to the hypothesis that the increase in administrative prevalence was due to real changes in the mental health of the population, and make it necessary to think that this increase might arise from other factors such as hypothetical variations in professionals’ diagnosis habits, mental health knowledge or in patient capability of or interest in reporting mental health problems.25 Likewise, other authors3 have indicated that this increase has to be viewed with caution, given that the overall category of “affective disorders” includes relatively few serious disorders, being limited to a greater number of “mild and non-specific” ones that presumably make the prevalence rise.
In women, there was an increase in all the diagnostic groups, except for “behavioural disorders associated with physiological dysfunctions and somatic factors”, including “eating disorders”. That the prevalence values stabilised could be due to the combined effect of the epidemiological variations of the disorder shown in some studies: maintenance of the incidence of anorexia nervosa2 and possible decrease in the incidence of bulimia nervosa26; the stabilisation might also be due to the implementation of specific programmes that (through greater information, sensitisation and ease of access) have made it possible to carry out earlier, more effective interventions in decreasing case chronification.
It is interesting to note that, despite the changes in population structure, the cases of organic mental illness (OMI) remained stable. This could be due to various factors: in Asturias, the neurology services are generally the ones that give the diagnosis of dementia; other OMI cases, such as strokes, are associated with affective disorders in over 50% of the cases27 and, when they consult mental health services, they do so mainly for mood disorders, which is the diagnosis that ends up in the records.
As far as psychotropic substances, assessment of patients that appear in emergency services or primary care show (as in our study) increased attention in the last 15 years for problems related with alcohol, while healthcare for other drugs remain stable.28 In Spain, between 2001 and 2007, there was a slight decrease in the prevalence of male and female consumption of psychotropic substances, except for cocaine use in women.1
The fact that psychosis prevalence remained stable is relevant, because these are chronic processes in which it is unreasonable to think that there could be a decrease in the incidence during the period. In addition, in the last decade, infrastructures (Comprehensive Treatment Centres) and programmes (assertive community treatment, administration of psychopharmaceuticals) have increased in Asturias, which would have produced greater recruitment and maintenance of patients in public healthcare services. Despite everything, the data coincide with those provided by other case records that have established minor tendency to change in the prevalence of treated schizophrenia.3 The data also coincide with previous RACPAS data showing (in the decade from 1987 to 1997) that the incidence figures of this disorder tended to drop, a tendency that was then considered to stem from demographic changes or administrative factors such as modifications in the diagnostic habits of the professionals.29 In the case of the psychoses, the prevalence treated from the beginning of the period studied is probably closer to the real prevalence than is the case in other disorders, which lowers the possibility of increase.
In the analysis of trends in the prevalence of treated disorders, the proportion of patients that lost contact with the services (death, treatment abandonment, releases) should be noted. Figures of up to 31% in a year have been given for abandonment of follow-up in mental health services.30 In a study performed in a community service, 17% of inappropriate follow-up loss was found; this occurred more frequently in younger, single patients that suffered from anxiety and somatoform disorders, and less often in patients with severe mental disorder (schizophrenia diagnoses turned out to be a solid predictor of maintained contact with the services).31 In Spain, a rate of around 20% was found for inappropriate treatment abandonment in a year, in patients with anxiety or depression.32 Follow-up losses could also occur in patients with acute psychotic episodes (especially secondary to toxic substances, which the RACPAS groups together with chronic psychotic disorders) and in addictions and eating behaviour disorders, given that this type of disorders occur in patients with characteristics associated with inappropriate follow-up losses (young, lacking family ties and having a low level of satisfaction with the services).
The significant increase in prevalence for most disorders during the period studied suggests that there is a “general” factor rather than factors related to groups of specific disorders. These increases in prevalence, which imply more individuals in contact with the services, may be due to: (a) changes in population structure (considering that the total population remained stable during the period, the increased contacts would have to be linked to age distribution modifications, which are reflected in the linear regression results); (b) changes in population attitudes, with a growing tendency to seek or accept formal mental healthcare more quickly and easily; (c) increases in stress in the population in the last decade related to deterioration of social conditions; (d) changes in the structure of the Mental Health Services (expansion and diversification of the healthcare system during the period); and (e) changes in the habits of the professionals (changes in diagnostic routines or greater duration of healthcare in the services).
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appears in this article.
Right to privacy and informed consentThe authors declare that no patient data appears in this article.
Conflict of interestThe authors have no conflict of interest to declare
Margarita Eguiagaray, Julio César Fernández and all the professionals who have made the correct functioning of the Asturias Cumulative Psychiatric Case Register possible.
Please cite this article as: Bobes J, et al. Evolución de la prevalencia administrativa de los trastornos mentales durante 13 años en Asturias. Rev Psiquiatr Salud Ment (Barc.). 2013;6:60-6.