Despite cautions by professional associations, benzodiazepines (BZD) and Z hypnotics (BZD/Z) are widely prescribed to older adults who are particularly susceptible to insomnia and anxiety, but who are also more sensitive to drugs adverse events. In this study, we assessed the prescription of BZD/Z drugs in a sample of older adults (≥65) who presented for emergency care after a fall.
MethodsWe collected the type, number and dose of BZD/Z drugs prescribed and explored gender differences in the prescription.
ResultsBZD/Z drugs were prescribed to 43.6% of the sample (n=654) and more frequently to women; 78.4% of prescriptions were for BZD/Z drugs with a short half-life. The majority of patients (83.5%) were prescribed only one type of BZD/Z, but 16.5% had been prescribed multiple BZD/Z drugs, with no gender difference. Doses higher than those recommended for older adults were prescribed to 58% of patients, being the doses significantly higher for men compared to women (70.0% vs 53.1%).
ConclusionsOver 40% of older adults presenting for emergency care after a fall had previously been prescribed BZD/Z drugs. Some important gender differences in the prescription of BZD/Z drugs were seen, especially prescription above the recommended dose and of drugs with a long-half life.
A pesar de las advertencias de numerosas asociaciones profesionales, las benzodiacepinas (BZD) y los hipnóticos Z (Z) son ampliamente prescritos a los ancianos ya que son especialmente susceptibles de padecer insomnio y ansiedad, pero a su vez resultan especialmente sensibles a la aparición de efectos secundarios a dichos medicamentos. En este estudio evaluamos la prescripción de BZD/Z en una muestra de ancianos (≥65) que se presentan en el servicio de urgencias de un hospital por haber sufrido una caída.
MétodosRecogimos información del tipo, número y dosis de los fármacos BZD/Z prescritos y exploramos la presencia de diferencias de género en dicha prescripción.
ResultadosLas BZD/Z habían sido prescritas a un 43,6% de la muestra (n=654), más frecuentemente a las mujeres. El 78,4% de las prescripciones fueron de BZD/Z de vida media corta. La mayoría de los pacientes (83,5%) tomaban solamente un fármaco BZD/Z, pero un 16,5% consumían más de una BZD/Z, sin diferencias de género. Un 58% de los pacientes consumían dosis de BZD/Z más elevadas que las recomendadas para ancianos, siendo la proporción significativamente más elevada para los hombres (70% vs. 53,1%).
ConclusionesAlrededor de un 40% de los ancianos que acuden a un servicio de urgencias por haber sufrido una caída se encontraban tomando BZD/Z. Hemos hallado algunas diferencias de género en la prescripción de BZD/Z, especialmente en la prescripción por encima de la dosis recomendada para ancianos y de fármacos de vida media larga.
Despite cautions by many national regulatory agencies and professional associations, a recent publication about benzodiazepine (BZD) use reinforced the efficacy of these drugs in the treatment of anxiety disorders and insomnia, and claimed that their use in older adults is generally accepted by geriatricians when short half-life compounds and low doses are prescribed.1 However, the beneficial effects of BZDs are often disputed and concerns expressed about their adverse events and high rates of prescription in older adults.2,3 Certainly, prescription decisions have to be made on a case-by-case basis and patients should be informed of both the risks and benefits of any prescribed medication.1
These decisions are not easy. Older adults are especially difficult to treat because they often have multiple morbidities that require polypharmacy.4 Also, changes in body composition and organ function during the ageing process can alter drug disposition and make older individuals more vulnerable to medication-associated adverse events.5 In particular, there is an age-related increase in the rate and severity of adverse effects of drugs that act on the central nervous system, which often results from a decrease in the number of neurons and synapses and greater permeability of the blood-brain barrier.6 BZDs are one of the most commonly prescribed drugs in older adults because of their proven efficacy, but care must be taken as their use and abuse may lead to unwanted effects, including cognitive deterioration,7 motor incoordination, ataxia, falls8–10 and respiratory failure.11–13
Clinical guidelines recommend that BZDs and the related group of non-benzodiazepine Z-drugs (zolpidem, zaleplon, zopiclone) should be used at the lowest possible dose, and selecting those with the shortest half-lives.14,15 However, in the real world, there is evidence that various types and doses of these BZD/Z drugs are frequently prescribed in the geriatric population,16 especially in women.3
Falls, especially in older patients, are a serious adverse event of BZD/Z-drugs use, often causing hip fracture and can have a serious impact on mobility, morbidity and mortality.17,18 While the association between BZD/Z drugs and falls in older adults is well established, less is known about the characteristics of patients sustaining injurious falls and the prescription of BZD/Z drugs in such a population
The objectives of this study are to describe the previous prescription of BZD/Z drugs in a sample of older adults attending a general hospital emergency service after sustaining a fall and to explore potential gender differences in the type, number and dose of BZD/Z drugs prescribed.
MethodsThis is a record linkage study, of older patients aged at least 65 years who consecutively attended the emergency department of Araba University Hospital in Vitoria (Spain) (between January and December 2010) due to a fall. The study was approved by the hospital's Ethics Committee. We collected data on patient sociodemographic characteristics and information about their previous prescription of BZD/Z drugs (active ingredients and dosage).
To assess whether the study subjects were prescribed short- or long-acting BZD/Z drugs, we classified the prescriptions into two groups: (1) drugs with an ultra-short or short half-life (<20h) (alprazolam, brotizolam, loprazolam, lorazepam, lormetazepam and zolpidem), and (2) drugs with a medium or long half-life (>20h) (bromazepam, clonazepam, clorazepate, diazepam, ketazolam and tetrazepam).
To assess whether the prescribed dose of BZD/Z drug was similar to the recommended dose, we determined the recommended defined daily dose (DDD) in non-geriatric adults (DDDadults) and in older adults(≥65 years old) (DDDolder adults), based on the drug fact sheet produced by the Spanish Agency of Medicines and Medical Devices19 and the recommendations of the World Health Organization.20
Statistical analysisDescriptive statistics were used to describe socio-demographic and “dose of BZD” variables of the study population: numbers and percentages (%) were shown for qualitative variables and means and standard deviations (SDs) for quantitative variables. Comparisons between men and women were made using the chi-square (χ2) test for qualitative variables (dose of BZDs/Z drug prescribed) and the Student's t test for independent samples for qualitative variables (DDDolder adults, DDDadults). The influence of gender on BZD/Z drug prescription or whether the prescribed dose exceeded the DDD was examined using logistic regression models with a dichotomous dependent variable (e.g., BZD/Z drug prescription yes vs no) and a dichotomous independent variable too (gender) adjusting the model by age. Results are reported as odds ratios (OR) and 95% confidence intervals with p values.
ResultsWe examined the records of 654 adults aged at least 65 years (230 men and 424 women), of whom 285 (43.6%) had been prescribed some type of BZD/Z drug up to 2 weeks before they attended the hospital due to a fall (83 men and 202 women). The mean age of all recruited patients was 79.9±8.5 years. Women were significantly older than men (80.7±8.4 years old vs 78.4±8.4 years; t=3302, p=0.001).
Among the 285 people with a BZD/Z drug prescription before their fall, there were 343 prescriptions of BZD/Z drugs, or 1.2 prescriptions per patient. Some patients were prescribed multiple BZD/Z drugs: 238 patients (83.5%) were prescribed one BZD/Z drug,13% (37 patients) two BZD/Z drugs, 3.2% (9 patients) three BZD/Z drugs and 0.4% (1 patient) four BZD/Z drugs. There were no gender differences in the number of BZD/Z drugs prescribed concurrently (X2=0.497, p=0.92).
Women were prescribed BZD/Z drugs significantly more often than men (47.6% prescribed women vs 36.1% prescribed men; X2=8.097, p=0.004). Overall, 243 prescriptions were to women and 100 to men. A logistic regression model assessed whether the older age of women had an influence on their greater prescription of BZD/Z drugs, using BZD/Z drug prescription (yes/no)as the dependent variable and gender as the independent variable, adjusting the model for patient age. We found that gender was still statistically significant, despite adjusting for age in the model (OR=1.53, p=0.013, CI: 1.094–2.137).
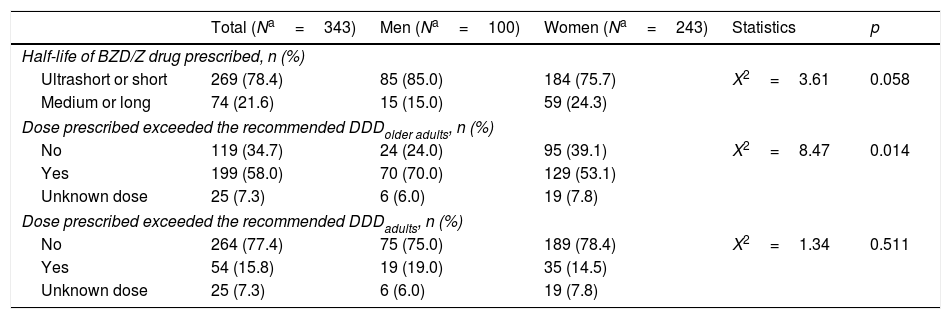
Table 1 shows the half-life category of BZD/Z drug taken (ultra-short/short or medium/long) and whether the dose prescribed exceeded the recommended DDD. As seen in Table 1, 21.6% of prescriptions were for BZD/Z drugs with a medium or long half-life, with a tendency for such drugs to be prescribed more to women than to men (24.3% vs 15%; X2=3.606, p=0.058). Moreover, 58.0% of prescriptions were for a dose above the recommended DDD in older adults (DDDolderadults) in, with a significantly higher percentage in men (70.0%) than women (53.1%) (X2=8.467, p=0.014). We performed logistic regression analysis taking whether the dose was consistent with DDDolder adults as the dependent variable, and patient gender as the independent variable, controlling for age. We found that men had a significantly greater chance of being prescribed BZD/Z drugs in excess of the DDD for older adults (OR=2.30, p=0.008, CI: 1.210–4.251). Furthermore, 54 prescriptions (15.8%) were for a dose that exceeded the DDD in non-geriatric adults (DDDadults), but there was no significant gender difference.
Type and dose of BZDs/Z drugs prescribed.
| Total (Na=343) | Men (Na=100) | Women (Na=243) | Statistics | p | |
|---|---|---|---|---|---|
| Half-life of BZD/Z drug prescribed, n (%) | |||||
| Ultrashort or short | 269 (78.4) | 85 (85.0) | 184 (75.7) | X2=3.61 | 0.058 |
| Medium or long | 74 (21.6) | 15 (15.0) | 59 (24.3) | ||
| Dose prescribed exceeded the recommended DDDolder adults, n (%) | |||||
| No | 119 (34.7) | 24 (24.0) | 95 (39.1) | X2=8.47 | 0.014 |
| Yes | 199 (58.0) | 70 (70.0) | 129 (53.1) | ||
| Unknown dose | 25 (7.3) | 6 (6.0) | 19 (7.8) | ||
| Dose prescribed exceeded the recommended DDDadults, n (%) | |||||
| No | 264 (77.4) | 75 (75.0) | 189 (78.4) | X2=1.34 | 0.511 |
| Yes | 54 (15.8) | 19 (19.0) | 35 (14.5) | ||
| Unknown dose | 25 (7.3) | 6 (6.0) | 19 (7.8) | ||
DDD=defined daily dose.
The BZD/Z drugs most frequently prescribed above DDDolder adults were lormetazepam (91.1% of 112 prescriptions), zolpidem (73.1% of 26 prescriptions) and lorazepam (56.6% of 99 prescriptions), with no significant gender differences.
DiscussionOur results show that almost half of all older adults who presented for emergency care after a fall had been prescribed BZD/Z drugs during the 2 weeks prior to the fall, mostly for short-acting compounds in accordance with current clinical guidelines.14,15 Psychiatry is tending towards precision medicine,21 but until it achieves this, we base it on clinical guidelines prepared by expert consensus. It still often prescribed on a trial and error basis, but medications that are good for some patients do always work for others, and there is no way to predict this before trying it. However, a substantial proportion (21.6%) of prescriptions was for medium or long half-life BZD/Z drugs, particularly among women (24.3% vs 15% in men). In addition, 16.5% of patients were prescribed multiple BZD/Z drugs and over the half of all BZD/D drug prescriptions were for doses higher than those recommended for older adults, with 70% of prescriptions in men being above the DDDolder adults.
The reasons why almost one-quarter of BZD prescriptions in women were for long-acting drugs are unknown. The symptoms of anxiety and insomnia are sometimes difficult to control in older people.22 It has been reported that BZDs with ultra-short half-lives may cause rebound anxiety,23 especially in the geriatric population. Hence, BZDs with a long half-life may be used for short periods to provide better symptom control after other non-pharmacological methods have failed. However, prolonged use of long-acting BZDs should be avoided due to the risk of accumulation and associated adverse effects.24 Also, even when used for a short time, BZDs with long half-lives are more likely to have residual effects the next day, including sedation, which would increase the risk of sustaining a fall. It is important to carefully follow-up older patients who have been prescribed long half-life BZDs, especially older women, who are more prone to falls than older men.25 There are many risk factors for falls in older people, including decreased muscle mass/strength and balance.26 BZD/Z drugs have also been reported to decrease balance27 and physical strength,28 thereby further increasing the fall risk in older patients. There is evidence that the use of BZD/Z drugs with long half-lives and the prolonged use of any BZD/Z drug is associated with a significant decrease in physical performance of older women29 and worse functional status.30 Thus, more care should be taken about the type, dose and duration of BZD/Z drugs prescribed to older women as they can impact on the risk of falls.
Early studies of BZD use in older patients showed that many (48%)were prescribed long-actingcompounds.31 Ourfinding that 21.6% of prescriptions for BZD/Z drugs were for compounds with a medium/long half-life are consistent with a recent American study, which reported that 25% of adults receiving BZDs were using long half-life BZDs.32 In accordance with a French study of psychoactive drug prescription,33 we found that the prescription of BZD/Z drugs was higher in women than in men, independent of age. This finding may be attributable to the fact that anxiety and insomnia are more common in women than men.34
Although the majority of patients were prescribed only one type of BZD/Z drug, almost two out of every ten patients received inappropriate prescribing of multiple BZD/Z drugs, despite evidence that such combinations have no benefits over monotherapy,35 and that this practice is contraindicated in older adults.23 This polypharmacy may reflect the difficulties in controlling insomnia and anxiety in older patients, and suggests there may be underutilization of non-pharmacologicalinterventions,36 such as counselling about sleep hygiene37 and the use of cognitive behavioural therapy38 or mindfulness-based meditation,39 that have been shown to be effective in treating insomnia and anxiety, including in older people.
Our results show that BZD/Z drugs were often prescribed at significantly higher doses than the recommended DDDolderadults, especially in men (70%), but also in women (58%). In some cases, the dose even exceeded the DDD in non-geriatric adults. This is in accordance with a previous observational study of older patients (mean age of 75 years) hospitalized in an intensive care unit, which found that men received higher doses of BZD (lorazepam) than women, after adjusting for variables such as age and severity of disease.40 Further, a population-based study in Taiwan found that being male and elderly were significantly associated with higher rates of continuation of BZDs once started.41 The reasons why BZD/Z drugs are frequently used at higher than recommended doses, especially in older men, are unclear. They could be attributed to the perception that, in case of agitation, men's behaviour could be aggressive, or due to men's higher body mass or metabolic differences between men and women.
The frequent use of BZDs above the recommended dose underlines the importance of implementing additional interventions to decrease insomnia and anxiety in older people. In Spain, an estimated 11.4% of the general population use benzodiazepines, with a higher likelihood of use in women, older patients and people suffering from a mental disorder.42 According to the PROTECT-EU project, developed in 7 European countries including Spain, BZD/Zs prescription rates (that is, number of prescriptions) varies from 5.7% to 16% and those rates were 1.5–2 times higher for women than men, especially in older patients.43
A small, open-label, randomized study has shown that a combination of BZD (lormetazepam 0.5mg/day) with sleep hygiene therapy is more effective at improving sleep architecture in older adults with insomnia than sleep hygiene therapy alone.44 Aslormetazepam 1mg can cause postural instability lasting up to 8h in older people,45 which is likely related to an increased risk of falls, it is good practice to use lower doses in older patients, if possible, to balance the benefits and risks of BZD treatment.
Chronic insomnia and anxiety are difficult to treat, especially in older adults. A recent study confirms that psychotropic medication, especially BZD, is an independent risk factor for falls,46 and that this risk is generally associated with a cumulative effect of BZD doses used in the weeks prior to the fall.47 Nevertheless, using the lowest effective doses of BZD/Z drugs and avoiding polypharmacy are targets that can be reached and could be an easy and effective way to decrease the fall risk in older adults. Our findings suggest that special care must be taken when prescribing BZD/Z drugs to women.
Given the high use of BZD/Z drugs in older people, various interventions have been examined for reducing such use. In some patients, it is possible to progressively and slowly taper the dose of BZD/Z drug. One report suggests that it may take more than one year to completely stop the treatment without incurring symptoms.48 A recent meta-analysis of randomized controlled trials concluded that BZD withdrawal tends to be more effective if combined with psychological therapy,49 especially cognitive behavioural therapy when cognition is not severely impaired. Clinical guidelines should consider that there will always be a residual group of patients in whom it will not be possible to decrease the BZD doses, and these individuals will require special supervision.50 This may include the use of fall prevention strategies and mobility aids. Special care should be taken in patients with concurrent mental disorders who require careful evaluation and optimal psychopharmacology.
Our study has several limitations that must be taken into consideration. First, the cross-sectional design means we are unable to draw any conclusions about causal relationships in the reported findings. Second, the patients were included in the study on arrival at the emergency department and the reason for diagnosis underlying the prescription of BZD/Z drugs was not always clear. Third, we could not confirm ingestion of these drugs (despite their prescription) within the 2 weeks before the fall. Fourth, there is no control group in this study. Finally, the study was conducted in one Spanish hospital and may not reflect practice elsewhere. Fourth, this is a single centre study so external validity should be jeopardize, but the Emergency Department of the University Hospital of Alava covers the entire population of the province (around 320000 people).
To conclude, we found that BZD/Z drugs were prescribed to over 40% of older adults who sought emergency care in a Spanish general hospital after a fall. We found certain gender differences in the prescribing of BZD/Z drugs to older adults, specifically higher rates of prescription of BZD/Z drugs and of long half-life benzodiazepines to women. Also, doses higher than recommended were prescribed to many patients, especially in men. These inadequate practices may be reduced by avoiding high doses and prolonged use of benzodiazepines with long half-lives, especially considering the special characteristics of ageing and the high morbidity associated with falls. It is important however, to bear in mind, that it is best to entirely avoid, if possible, prescribing BZD/Z drugs to the elderly.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestNone.
This work was supported by health research funds from the Spanish Government, cofinancing FEDER (PS09/02002, EC10-333, PI10/01430, PI10/01746, PI11/01977, PI11/02708, 2011/1064, 1677-DJ-030, EC10-220, PI12/02077, PI13/02252, PI13/00451 and PI14/01900); European Regional Development Funds (Mastermind is partially funded under the ICT Policy Support Programme (ICT PSP) as part of the Competitiveness and Innovation Framework Programme by the European Community) (FI-STAR project has received funding from the European Union's Seventh Programme for research, technological development and demonstration under grant agreement No. 604691); local grants from the Department of Education, Linguistic Policy and Culture of the Basque Country Government (2008111010, 2009111047, 2010111170, 2010112009, 2011111110, 2011111113, 2013111162, and KRONIK 11/010); the Basque Foundation for Health Innovation and Research (BIOEF); Networking Center for Biomedical Research in Mental Health (CIBERSAM); the Spanish Clinical Research Network (CAIBER; 1392-D-079) and the University of the Basque Country (GIC10/80, GIC12/84). The psychiatric research department in University Hospital Araba is supported by the Stanley Research Foundation (03-RC-003).The founding sources had no role in the study design, collection and interpretation of data, writing the manuscript or in the decision to submit the article for publication.
Please cite this article as: Martinez-Cengotitabengoa M, Diaz-Gutierrez MJ, Besga A, Bermúdez-Ampudia C, López P, Rondon MB, et al. Prescripción de benzodiacepinas y caídas en mujeres y hombres ancianos. Rev Psiquiatr Salud Ment (Barc). 2018;11:12–18.