The Philadelphia Mindfulness Scale (PHLMS) is a brief questionnaire for assessing 2 key components of mindfulness: present moment awareness, and acceptance. This study was aimed at evaluating the psychometric properties of the Spanish version of PHLMS in a sample of participants with and without psychiatric conditions.
Material and methodsThe Spanish version of the PHLMS was administered to a sample of 395 volunteers (256 of them with a psychiatric condition, and 130 from a student sample).
ResultsExploratory factor analysis found a two factor solution, which was also observed in the original version of the scale, with an explained variance of 44.02%. The scale showed good reliability (Cronbach α between 0.81 and 0.86), and an adequate convergent validity with other questionnaires of mindfulness and acceptance. The results also showed a similar discriminant validity to that in the original instrument validation between PHLMS and the clinical symptomatology reported.
ConclusionsThe Spanish version of the PHLMS is a psychometrically sound measure for assessing two core components of mindfulness (i.e. awareness and acceptance) in clinical and research settings.
La Philadelphia Mindfulness Scale (PHLMS) es un cuestionario breve que evalúa 2 componentes clave de la atención plena: la conciencia en el momento presente y la aceptación. El presente estudio evalúa las propiedades psicométricas de la versión española de la PHLMS tanto en una muestra control de estudiantes universitarios como en población con patología psiquiátrica.
Material y métodosSe administró la versión española de la PHLMS a 395 voluntarios (256 con patología psiquiátrica y 139 estudiantes).
ResultadosEl análisis factorial exploratorio de la versión española de la PHLMS apoya la solución bifactorial de la versión original con una varianza explicada del 44,02%. La escala presentó una adecuada fiabilidad (α de Cronbach de 0,81 a 0,86). La PHLMS mostró una adecuada validez convergente con los otros cuestionarios de atención plena y aceptación y una validez divergente de la clínica depresiva y ansiosa comparable a la de la versión original.
ConclusionesLa versión española de la PHLMS presenta adecuadas propiedades psicométricas y puede ser utilizada para medir 2 componentes constituyentes de la atención plena –i.e. conciencia y aceptación– tanto en el ámbito clínico como en investigación.
Normally mindfulness is defined as “intentionally paying attention to the present moment, without judging”.1 Over the last 20 years mindfulness has been introduced and spread very swiftly in modern scientific psychology, to a great extent thanks to the therapeutic interventions based on it or that integrate it as an essential technique within the programme (e.g., cognitive therapy based on mindfulness,2 stress reduction programmes based on mindfulness,3 dialectical behaviour therapy4 and acceptance and commitment therapy,5 among others).
To assess mindfulness and study its relationship with various aspects of health, different scales have been designed. Examples are the Freiburg Mindfulness Inventory (FMI),6Kentucky Inventory of Mindfulness Skills (KIMS),7Cognitive and Affective Mindfulness Scale Revised (CAMS-R),8Toronto Mindfulness Scale (TMS),9Five Facets Mindfulness Questionnaire (FFMQ)10 and the Mindful Attention Awareness Scale (MAAS).11 There are considerable differences among these self-reports, because all of them do not use the same definition of mindfulness, they are not aimed at the same population or they have used different methodologies to build them. For example, the FMI considers that mindfulness abilities can only be achieved by meditation,12 whereas in the MAAS mindfulness is conceptualised as an innate ability, present to a greater or lesser degree in all individuals.11 The second scale mentioned is sustained in a one-way view of mindfulness and assesses only the attention/awareness variable in the present. This 1-dimensional perspective contrasts con that of instruments such as the FFMQ and KIMS, which distinguish up to 5 dimensions, some of which are close to the attention/awareness factor and others, more related with a factor of acceptance.
Aiming to reach a consensus on the elements of mindfulness defined by several theorists and put the concept to use more properly, Bishop et al13 proposed 2 components that seemed to be intrinsic to mindfulness: (a) self-regulation of attention sustained in the present and (b) an attitude of curiosity, openness and acceptance towards the experience. The same definition was also picked up by Cardaciotto et al.14 as a “tendency to be highly aware of internal and external experiences in a context of non-judgemental acceptance”. Although it has been argued that both factors (that of attention/awareness and that of acceptance) could present a certain overlap at the conceptual level,11,15 it also seems reasonable that both aspects are differentiated.13 There are clear examples where high awareness and focus are not accompanied by acceptance, as in the case of anxiety disorders, depression or addictive behaviour.16
The Philadelphia Mindfulness Scale (PHLMS)14 is a short self-report that, up till now, is the scale formulated from a 2-dimensional view of mindfulness developed by Bishop et al.13 The 2 components that it assesses are: (1) awareness in the present moment−defined as “continual monitoring of the internal and external stimuli”−and (2) acceptance−defined as “non-judgemental posture towards one's experience”. The objective of this study was to evaluate the psychometric properties of the Spanish version of the PHLMS in both a control sample of university students and in a population with psychiatric pathology.
MethodParticipantsThe global study sample consisted of 395 participates (289 females and 106 hombres), aged from 18 to 68 years, with a mean age of 31.9 (SD=10.82). There were 2 groups in the sample: a subclinical group (n=256) and another composed of students (n=139). The patients in the psychiatric sample came from the Hospital de la Santa Creu i Sant Pau and from the Fundació Althaia (Xarxa Assistencial Universitària, Manresa) and fulfilled the diagnostic criteria (DSM-IV-TR)17 for one of the following disorders: borderline personality disorder (BPD) (n=69), eating behaviour disorder (n=71), major depressive disorder (n=48) and cocaine dependence disorder (n=68). The non-psychiatric sample was composed of students in the Faculty of Psychology at the University of Valencia and at the Santa Creu i Sant Pau University Nursing School. Table 1 presents the principal sociodemographic characteristics of the 2 study groups. The criteria for exclusion for the entire sample were as follows: presenting any other acute-phase psychiatric illness or psychotic disorder, mental retardation, sensory deficits or language difficulties that made it impossible to fill in the questionnaires.
Sociodemographic characteristics of the student and psychiatric samples.
| Student sample(n=139) | Psychiatric sample(n=256) | P | |
| Sex (% woman) | 75.54 | 71 | n.s. |
| Age | 28.1 (9.14) | 30.75 (10.19) | n.s. |
| Education | <0.001 | ||
| Primary | – | 37.5% | |
| Secondary | – | 41.3% | |
| University | 100% | 20.6% | |
| Marital status | <0.001 | ||
| Single | 63% | 56.1% | |
| Partner relationship/married | 36% | 31.1% | |
| Separated | 1% | 12.8% | |
| Work situation | <0.001 | ||
| Working | 30% | 34.54% | |
| Unemployed/not working | 27.32% | ||
| Work leave | 27.32% | ||
| Only studies | 70% | 10.80% | |
Chi squared test was performed for the categorical variables and Student's t-test for the continuous ones.
The psychiatric sample was recruited using consecutive sampling after checking compliance with the criteria for inclusion and exclusion from the study. The student participants filled in the questionnaires in a classroom at the university. All the participants read and signed the informed consent and participated in the study voluntarily.
To adapt the scale, the normal procedure of translation-back translation was followed.18 A bilingual individual with clinical experience performed the translation of the original scale to Spanish with the collaboration of a clinician with great experience as a mindfulness trainer. An independent native English-speaking translator specialised in translating biomedical texts did the back translation of the Spanish version of the scale to English. This was then sent to the authors of the PHLMS, who, after several corrections to the Spanish version, certified its fit to the original text.
For the test–retest reliability study, a subsample of 53 participants answered the PHLMS once again 2 weeks after the 1st administration. Sensitivity to change was established by analysing the changes in the PHLMS subscales in a subsample of 19 patients diagnosed with BPD, who participated in a 10-week mindfulness intervention in the context of dialectical behaviour therapy (this type of intervention has been shown to be clinically effective in other studies19,20).
InstrumentsThe PHLMS14 is a 20-item questionnaire that assesses 2 mindfulness constructs: awareness and acceptance. It includes questions on how often various aspects related to these constructs have been experienced in the last week; the answers are presented in the form of a 5-point Likert scale, ranging from 1 (never) to 5 (very often).
The Spanish-version FFMQ21 is a 39-item scale that measures 5 mindfulness factors: observation, description, acting consciously, not judging, and not reacting to inner experience. The response format consists of a 5-point scale, with answers ranging from 1 (never or very rarely true) to 5 (very often or always true).
The MAAS22 is a 15-item scale that measures the how often the processes of attention to and awareness of the present moment occur in daily life. The response format is a 6-point scale, ranging from 1 (almost always) to 6 (almost never). High scores indicate greater states of mindfulness.
The Acceptance and Action Questionnaire (AAQ)23 is a 9-item questionnaire that assesses experiential avoidance and psychological acceptance. The response format is an 8-point scale, with answers ranging from 1 (never true) to 7 (always true).
The Epidemiological Studies-Depression Scale (CES-D)24 is composed of 20 items. It assesses the presence of depressive symptoms during the last week. The response format is a 4-point scale, with answers ranging from 0 (never or rarely/less than a day) to 3 (very often or always/5–7 days).
The State-Trait Anxiety Inventory-State (STAI-S)25 is a 20-item scale that assesses components of state of anxiety. The response format is a 4-point scale, with a range from 0 (nothing) to 3 (a lot).
Data analysisOur objective was to evaluate the PHLMS construct validity, internal consistency, convergent and divergent validity, temporal reliability and sensitivity to change. To that end, the analyses listed below were carried out.
We performed an exploratory factorial analysis (EFA) using main axis factoring and promax rotation to assess the construct validity of the scale. To study PHLMS internal consistency, Cronbach's alpha reliability coefficient was determined for the total scale and each of the subscales.
To evaluate convergent validity in a subsample of 291 participants (student group, n=83; clinical group, n=208), Pearson correlations were estimated between the PHLMS and the other mindfulness and acceptance scales (FFMQ, MAAS and AAQ). The correlations between the PHLMS and AAQ were obtained only for the patient sample. The divergent validity study was carried out with a subsample of 253 participants (student group, n=123; clinical group, n=130), correlating PHLMS with CES-D and STAI-S scales. The temporal reliability of the scale was studied in a subsample of 32 participants from the student group and 21 patients with BPD using the Pearson correlation coefficient between the PHLMS scores obtained in 2 consecutive administrations separated by 2 weeks. We assessed PHLMS sensitivity to change in a subgroup of patients with BPD (n=19) after a mindfulness intervention that lasted 10 weeks; to do so, the means for the paired-samples t-test were compared for the pre- and post-therapy scores. The t-tests for independent samples (student and clinical groups) were compared to evaluate whether both groups could be differentiated by PHLMS scores. Cohen's d was also calculated to provide information as to the size of the effect of these differences.
Data analysis was carried out using the statistical package SPSS version 18.0 for Windows.
ResultsSociodemographic characteristics of the samplesNo statistically significant differences were observed between groups with respect to age and sex; in contrast, such differences were found in education level, marital status and work situation. Table 1 presents the main sociodemographic characteristics of the sample of individuals with psychiatric pathology and of the student sample.
Construct validityThe EFA was carried out using a sample of 395 participants. After checking that sampling adequacy conditions were fulfilled (KMO=0.85 and significant Bartlett sphericity test of P<.001), the main scale axes were factored using promax rotation. The initial solution indicated that there were 4 factors with eigenvalues greater than 1, which would explain 57.02% of the total variance. However, in agreement with (a) the theoretical framework on which this scale was originally developed,14 (b) the presence of 2 predominant factors observed in the sedimentation graph (Fig. 1), (c) the superior interpretability of the 2-factor solution, (d) the principle of parsimony, and (e) the factorial structure of the original PHLMS version,14 a 2nd EFA was carried out restricting the solution to 2 factors. These 2 factors explained 42.49% of the total variance. Based on the results of this 2nd EFA, the items were then purified in agreement with the following main criterion: eliminating the items that presented low communality, given that the objective of every factorial analysis is to explain the variance using shared factors. Communality expresses the amount of shared variance in each item through the resulting factors; consequently, those with reduced communalities (lower than 0.40) could be eliminated because of their low contribution to the factorial solution.26 Likewise, we used another 3 criteria commonly utilised to select items: the factor load of the item with the factor or factors extracted, Pearson correlation coefficient between the item and the subscale or factor (without the item itself) to which it belongs, and Cronbach's α value that would reach this subscale if the item were eliminated. Specifically, we considered to be eliminable all items with factor loads lower than 0.3227 in all of the extracted factors, with corrected item-total correlation values lower than 0.30,28 or those whose elimination increased subscale reliability by more than 0.02 points.29 Item 15 was the only one that satisfied some of the conditions (in fact, 3 of the 4) recommending its elimination. This item presented communality lower than 0.40 (0.21), a factor load lower than 0.32 (0.31) in the 2 factors or subscales and a corrected item-total correlation lower than 0.40 (0.30) with the subscale to which it would have been assigned based on its greater factor load. The items finally selected (that is, all of them except for Item 15) were subjected to an EFA again. The 2-factor solution without Item 15 explained 44.02% of the total variance. Table 2 shows the items and factor loads for the items from the Spanish version of the scale for the factors labelled awareness and acceptance, before and after Item 15 was eliminated.
Exploratory factorial analysis: variance explained and configuration array.
| Factors | PHLMSItems 1–20 | PHLMSEliminating Item 15 | ||
| Eigenvalue | % Variance | Eigenvalue | % Variance | |
| 1 | 4.90 | 24.49 | 4.76 | 25.08 |
| 2 | 3.60 | 18.00 | 3.60 | 18.94 |
| Configuration array | ||||
| Items | Factor 1Acceptance | Factor 2Awareness | Factor 1Acceptance | Factor 2Awareness |
| 1. I am aware of what thoughts are passing through my mind | −0.026 | 0.572 | −0.032 | 0.574 |
| 2. I try to distract myself when I feel unpleasant emotions | 0.434 | 0.218 | 0.446 | 0.228 |
| 3. When talking with other people, I am aware of their facial and body expressions | −0.105 | 0.555 | −0.110 | 0.556 |
| 4. There are aspects about myself that I don’t want to think about | 0.608 | −0.274 | 0.596 | −0.273 |
| 5. When I shower, I am aware of how the water is running over my body | 0.160 | 0.451 | 0.150 | 0.450 |
| 6. I try to stay busy to avoid thoughts and feelings from coming to mind | 0.721 | −0.028 | 0.726 | −0.021 |
| 7. When I am startled, I notice what is happening inside my body | 0.069 | 0.518 | 0.054 | 0.515 |
| 8. I wish I could control my emotions more easily | 0.528 | −0.117 | 0.517 | −0.117 |
| 9. When I walk outside, I am aware of smells or how the air feels against my face | 0.093 | 0.495 | 0.089 | 0.498 |
| 10. I tell myself that I shouldn’t have certain thoughts | 0.709 | −0.090 | 0.703 | −0.086 |
| 11. When someone asks me how I am feeling, I can identify my emotions easily | −0.195 | 0.604 | −0.196 | 0.607 |
| 12. There are things that I try not to think about | 0.798 | −0.161 | 0.799 | −0.155 |
| 13. I am aware of the thoughts I’m having when my mood changes | 0.124 | 0.625 | 0.110 | 0.623 |
| 14. I tell myself that I shouldn’t feel sad | 0.564 | 0.055 | 0.561 | 0.059 |
| 15. I notice changes inside my body, like my heart beating more quickly or my muscles getting tense | 0.314 | 0.132 | – | – |
| 16. If there is something I don’t want to think about, I’ll try many things to get it out of my mind | 0.638 | 0.223 | 0.639 | 0.230 |
| 17. When my emotions change, I am aware of them immediately | −0.053 | 0.648 | −0.066 | 0.645 |
| 18. I try to put my problems out of my mind | 0.487 | 0.140 | 0.493 | 0.147 |
| 19. When talking with people, I am aware of the emotions I am feeling | 0.064 | 0.626 | 0.053 | 0.625 |
| 20. When a bad memory comes to mind, I try to distract myself to make it go away | 0.630 | 0.159 | 0.638 | 0.168 |
The factors of awareness and acceptance showed no significant correlation between them in the student group (r=−0.050, P>.05), but there was in the clinical group (r=−0.218, P=.001).
All the results that are indicated hereafter refer to the Spanish version of the PHLMS that does not include Item 15 from the original version.
Internal consistencyThe Spanish version of the PHLMS presented a total Cronbach's α of 0.82. As for its subscales, α=0.86 was observed for the acceptance subscale and α=0.81 for the awareness subscale.
Temporal stabilityWe studied PHLMS test–retest reliability in a subsample of 32 participants from the student group and 21 patients with BPD. To this end, we compared the scores obtained in 2 administrations separated by 2 weeks, using a paired-samples t-test that did not give a significant result; we also carried out Pearson correlations for the score on the awareness (r=0.81; P<.001) and acceptance (r=0.80; P<.001) subscales.
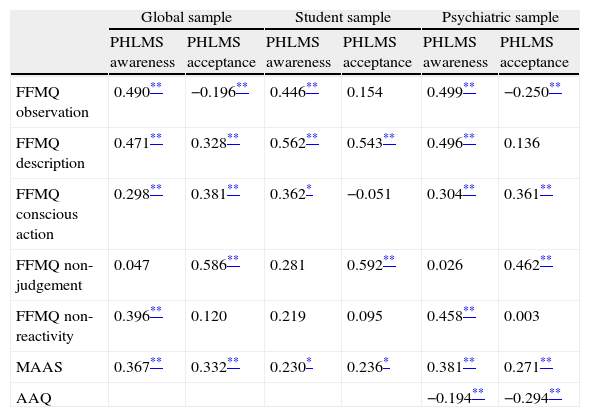
Convergent and divergent validityTo study convergent validity, the correlations between the PHLMS subscales and those of the FFMQ, MAAS and AAQ were evaluated, with significant correlations being observed among almost all the subscales (from r=−0.20 to r=0.59; with P<.05 and P<.01, respectively). Table 3 details, for each group, the correlations between the scores of the PHLMS subscales and the 5 subscales of the FFMQ (observation, description, acting consciously, non-judgement and non-reactivity to inner experience), MAAS and AAQ. The divergent validity of the PHLMS was established using the correlation of the scores of the awareness and acceptance subscales with the scales for depressive symptoms and anxiety (CES-D and STAI-S, respectively); significant correlations were seen from r=−0.39 to r=−0.15 (con P<.05 and P<.0, respectively). Table 4 presents the correlations obtained for the student and patient subsamples specified by group.
Convergent validity of the PHLMS with measurements of mindfulness and experimental avoidance for the control and psychiatric samples.
| Global sample | Student sample | Psychiatric sample | ||||
| PHLMS awareness | PHLMS acceptance | PHLMS awareness | PHLMS acceptance | PHLMS awareness | PHLMS acceptance | |
| FFMQ observation | 0.490** | −0.196** | 0.446** | 0.154 | 0.499** | −0.250** |
| FFMQ description | 0.471** | 0.328** | 0.562** | 0.543** | 0.496** | 0.136 |
| FFMQ conscious action | 0.298** | 0.381** | 0.362* | −0.051 | 0.304** | 0.361** |
| FFMQ non-judgement | 0.047 | 0.586** | 0.281 | 0.592** | 0.026 | 0.462** |
| FFMQ non-reactivity | 0.396** | 0.120 | 0.219 | 0.095 | 0.458** | 0.003 |
| MAAS | 0.367** | 0.332** | 0.230* | 0.236* | 0.381** | 0.271** |
| AAQ | −0.194** | −0.294** | ||||
AAQ: Acceptance and Action Questionnaire; FFMQ: Five Facet Mindfulness Questionnaire; MAAS: Mindful Attention Awareness Scale; PHLMS: Philadelphia Mindfulness Scale.
Correlations of the PHLMS subscales with the CESD-D and STAI-S in the control and psychiatric samples.
| Global sample | Student sample | Psychiatric sample | ||||
| PHLMS awareness | PHLMS acceptance | PHLMS awareness | PHLMS acceptance | PHLMS awareness | PHLMS acceptance | |
| CES-D | −0.155* | −0.390* | −0.114 | −0.334** | −0.187* | −0.257** |
| STAI-S | −0.227* | −0.255* | −0.201 | −0.291* | −0.249** | −0.060 |
CES-D: Center for Epidemiological Studies-Depression; PHLMS: Philadelphia Mindfulness Scale; STAI-S: State-Trait Anxiety Inventory-State.
The pre- and post-treatment assessments were compared, with significant variation between the pre-treatment mean of the acceptance subscale and the post-treatment score being seen: 24.10 (SD=8.46) vs 27.53 (SD=8.41); t=−2.493; gl=18; P=.02; d=0.29). No significant changes were observed between the pre- and post-treatment means for the awareness subscale: 30.89 (SD=7.85) vs 31.47 (SD=6.94); t=−0.589; gl=18; P=.5; d=0.08.
Differences in the Philadelphia Mindfulness Scale by groupThe student and el clinical groups significantly differed in the mean scores on the acceptance subscale: 31.83 (SD=7.52) vs 25.89 (SD=6.75), respectively (t=7.893; gl=380; P<.001; d=−0.83). No significant differences were seen between the student and clinical groups with respect to the awareness subscale: 32.87 (SD=4.97) vs 31.90 (SD=6.46), respectively (t=1.628; gl=384; P=.10; d=−0.17).
DiscussionThe Spanish version of the PHLMS presents a 2-factor structure and some psychometric properties similar to those of the original scale.14 The 2 scale factors (acceptance and awareness) were observed in the factorial analysis and explained a variance that, after the elimination of Item 15, was 44.02%, above that obtained in the original PHLMS study. It is relevant to note that the psychometric functioning of Item 15 was already irregular in the original validation of the instrument, where it presented a considerable factor load in both factors.14 Although the 2-factor structure from the original article on the scale was replicated in the global sample, these factors were found to be inter-related in the sample of patients with psychiatric pathology.
The acceptance and awareness subscales showed appropriate internal consistence. As for the convergent validity with other scales of mindfulness and acceptance, the subscales of the Spanish version of the PHLMS correlated at global level with the corresponding means of the other scales. In both samples, the awareness and acceptance subscales correlated positively and significantly with the MAAS, and a positive relationship was seen between the awareness subscale and 4 of the FFMQ facets, as well as between the acceptance subscale and the facet of not judging. The acceptance subscale correlated negatively and significantly with the AAQ and positively with the FFMQ subscale of not-judging, which are conceptually closer to this construct. Similar results were obtained in the original PHLMS article,14 in which correlations were also observed between the PHLMS with the AAQ and with the KIMS subscale of not judging (scale forerunner to the FFMQ) were also. The acceptance subscale also correlated positively with the MAAS.
However, there were differences between groups with respect to the correlations between the acceptance subscale and various facets of the FFMQ, as well as between the awareness subscale and the non-reactivity subscale. For only the clinical sample, a negative correlation was seen between acceptance and the observation facet of the FFMQ, a positive relation between acceptance and conscious action, and the awareness subscale correlated positively with FFMQ non-reactivity. In the student group, there was a correlation between acceptance and the FFMQ facet of description, which was for found in the patient group. For further details, see Table 3.
In general terms, the behaviour of the correlations between the PHLMS subscale of awareness and the other scales of mindfulness responded to what was expected. However, it is surprising that, in the patient group, the FFMQ facet of non-reactivity correlated only with the PHLMS awareness factor and not with that of acceptance, given that non-reactivity along with not judging would be the theoretical equivalent of the component of acceptance measured in the FFMQ.30 Turning to the matter of the acceptance subscale, it behaved very differently depending on the group studied. In fact, at least in the clinical group, the hypothesis proposed by Bishop et al13 and defended by Cardaciotto et al14–that awareness and acceptance would behave independently–seemed not to receive any support: in addition to the negative correlation found between the acceptance and awareness subscales in this group, crossed relations were also observed between these subscales and their theoretical counterparts on the FFMQ. This fact would back the theory proposed by Brown and Ryan,11,15 in which acceptance and awareness are considered as 2 highly inter-related concepts.
The negative correlation seen between the acceptance subscale and the observation subscale on the FFMQ in the group of psychiatric patients was not reported in the validation of the original instrument carried out with 78 university students in psychotherapeutic support and with the KIMS (the instrument from which the FFMQ derives). This result might be explained by the varying, and even occasionally antagonistic, behaviour of the FFMQ observation subscale with other indexes and aspects of mindfulness depending on the population studied,21,31 which would be suggested by the fact that this association was observed only in the psychiatric sample. In this regard, in a study where the behaviour of the FFMQ in patients with eating disorders was analysed, the observation factor correlated significantly and positively with the dietary clinical symptoms.32 The capability of self-observation seemed to play an adaptive role in some cases and a maladaptive one in others.33 The negative correlations seen between the PHLMS subscales could also be due to the theoretical overlap between the component of awareness and the facet of observation.
The correlations observed between the PHLMS and anxious and depressive symptoms indicated, at the global level, an inverse relationship between the 2 subscales and clinical anxious and depressive symptoms. This result agrees with many previous studies where the scores obtained on mindfulness questionnaires had a negative relationship with affective and anxious symptoms (for a review34). It should be pointed out that, as in the original study on non-clinical samples, the acceptance subscale would be more sensitive to anxious and depressive symptoms than the awareness scale, which does not correlate with either of the 2 in control student samples.14 In parallel, significantly lower scores were seen in the acceptance subscale in the clinical group than in the non-clinical sample, while this was not true in the awareness subscale. This backs the usefulness of separately measuring both components of mindfulness and the central role–already suggested in the original validation of the scale14–that the construct of acceptance would seem have in mental disorders.
The test-retest reliability analysis shows that the PHLMS presents appropriate temporal stability. As for the sensitivity to change, only the subscale of acceptance seemed to be sensitive to a 10-week mindfulness intervention. This could indicate that the component of attitude (acceptance) has greater sensitivity to change than that of attention (awareness) in short mindfulness interventions in BPD.19,20 Another matter is that, although the awareness factor significantly predicted psychiatric seriousness in the Cardaciotto et al14 study, the coefficient β was 10 times less than that provided by the factor of acceptance; it could therefore be speculated that although the short mindfulness intervention was capable of inducing changes in psychiatric symptoms, these improvement would be especially reflected in the factor of acceptance and not in that of awareness.
Our study has some limitations, among which we could highlight the absence of psychiatric evaluation in the student group, which makes it impossible to rule out the presence of psychopathology in that sample. Another point is that, as the sample involved was entirely university students, it is impossible to extrapolate the results for this group as standard data. The differences between groups related to years of education, marital status and work situation could also constitute a study limitation. Likewise, the psychiatric sample was composed of patients with various diagnoses; this fact would on the one hand increase sample representativeness, but it would also reduce the possibility of finding differences with respect to the control group due to high heterogeneity. It should also be pointed out that, to provide greater detail about the behaviour of the scale, we considered correlations with significance levels of P<.05 in the analysis of convergent and divergent validity; these are levels higher than those normally advisable in the case of estimating multiple correlations. This fact could have increased the probability of making type i errors. Finally, the study of sensitivity to change was performed on only a group of patients with borderline personality disorder, so the results might not be applicable to other psychiatric populations.
In conclusion, the Spanish version of the PHLMS has been shown to be a psychometric instrument comparable to the original to measure the constructs of awareness and acceptance in the Spanish-speaking population with or without psychiatric pathology. However, the relationship between awareness and acceptance would seem to differ based on the presence or absence of psychopathology. The fact of differentiating mindfulness into its 2 essential components can make it possible to study more specifically the effects of mindfulness interventions and the mediating effect of each factor in these results.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that procedures conformed to the ethical standards of the responsible committee on human experimentation and in accordance with the World Medical Association and the Helsinki Declaration.
Confidentiality of dataThe authors declare that they have followed the protocols of the workplace on the publication of data from patients.
Right to privacy and informed consentThe authors have obtained the informed consent of patients and/or subjects referred to in article consent. This document is in the possession of the corresponding author.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Tejedor R, Feliu-Soler A, Pascual JC, Cebolla A, Portella MJ, Trujols J, et al. Propiedades psicométricas de la versión española de la Philadelphia Mindfulness Scale. Rev Psiquiatr Salud Ment (Barc). 2014;7:157–165.