Blunt cardiac trauma (BCT) includes a number of diseases ranging from clinically silent arrhythmias to lethal cardiac wall rupture. The most common form is “cardiac contusion”, which is currently under debate. The absence of a clear definition and the lack of diagnostic tests of choice make diagnosing cardiac contusion difficult. We present the case report of a healthy young patient who went to the emergency department with electrocardiogram changes following blunt chest trauma, and review the current literature on the subject.
El traumatismo cardiaco cerrado (TCC) incluye una serie de patologías que van desde arritmias clínicamente silentes hasta la muerte por la rotura de la pared cardiaca. La forma más habitual es la “contusión cardiaca”, lo cual actualmente se encuentra en debate. La ausencia de una definición clara así como las pruebas diagnósticas de elección hacen el diagnóstico de contusión cardiaca difícil. Presentamos el caso clínico de un paciente joven y sano que se presenta al servicio de urgencias con cambios en el electrocardiograma tras un traumatismo torácico cerrado y se revisa la literatura actual sobre el tema.
The incidence of blunt cardiac trauma (BCT) after blunt chest trauma is difficult to determine and ranges from 8% to 76%. Moreover, its clinical presentation varies enormously, and there is no defined pattern for ruling out or documenting cardiac involvement. Recently, it has been demonstrated that an electrocardiogram and troponins may have a 100% negative predictive value in BCT. We present the case of a 56-year-old patient with ECG abnormalities following a fall from a bicycle and impact with the handlebars in the central chest region.
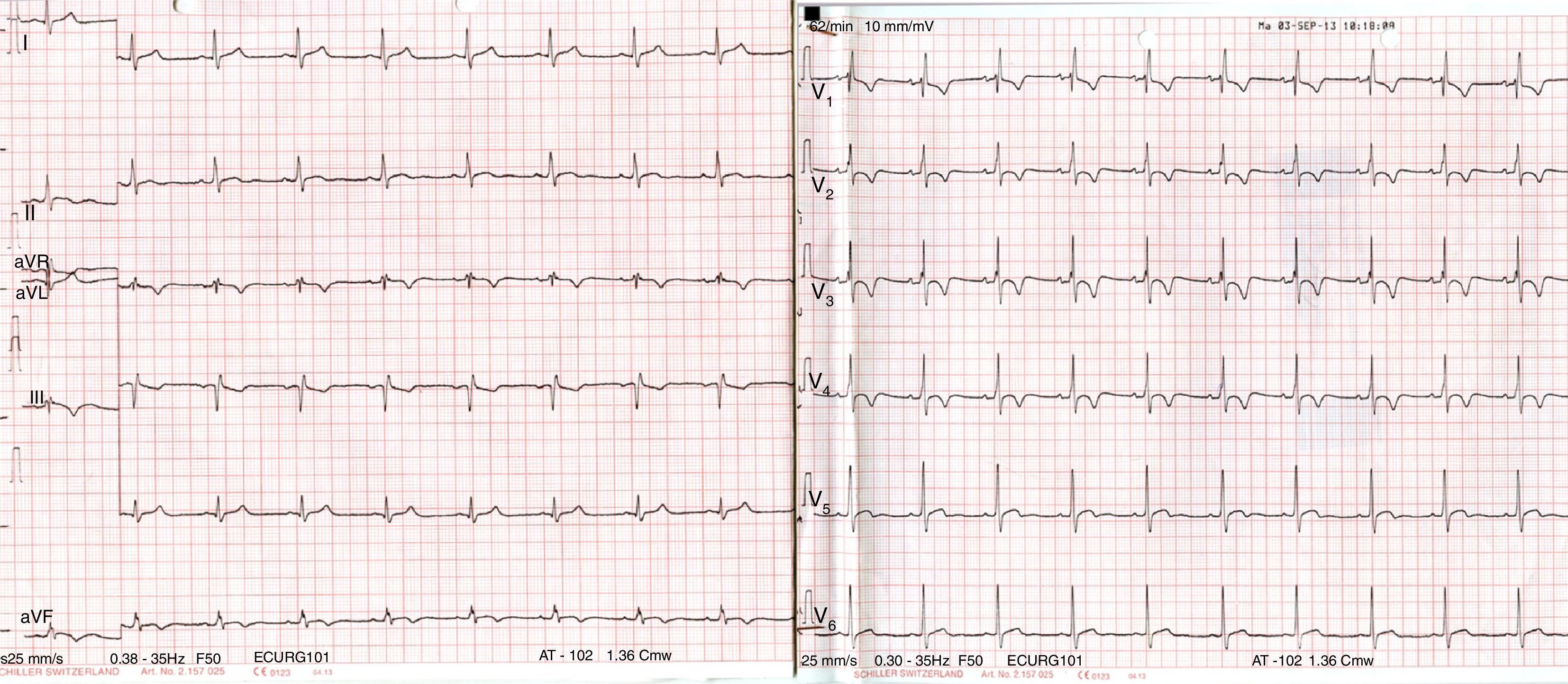
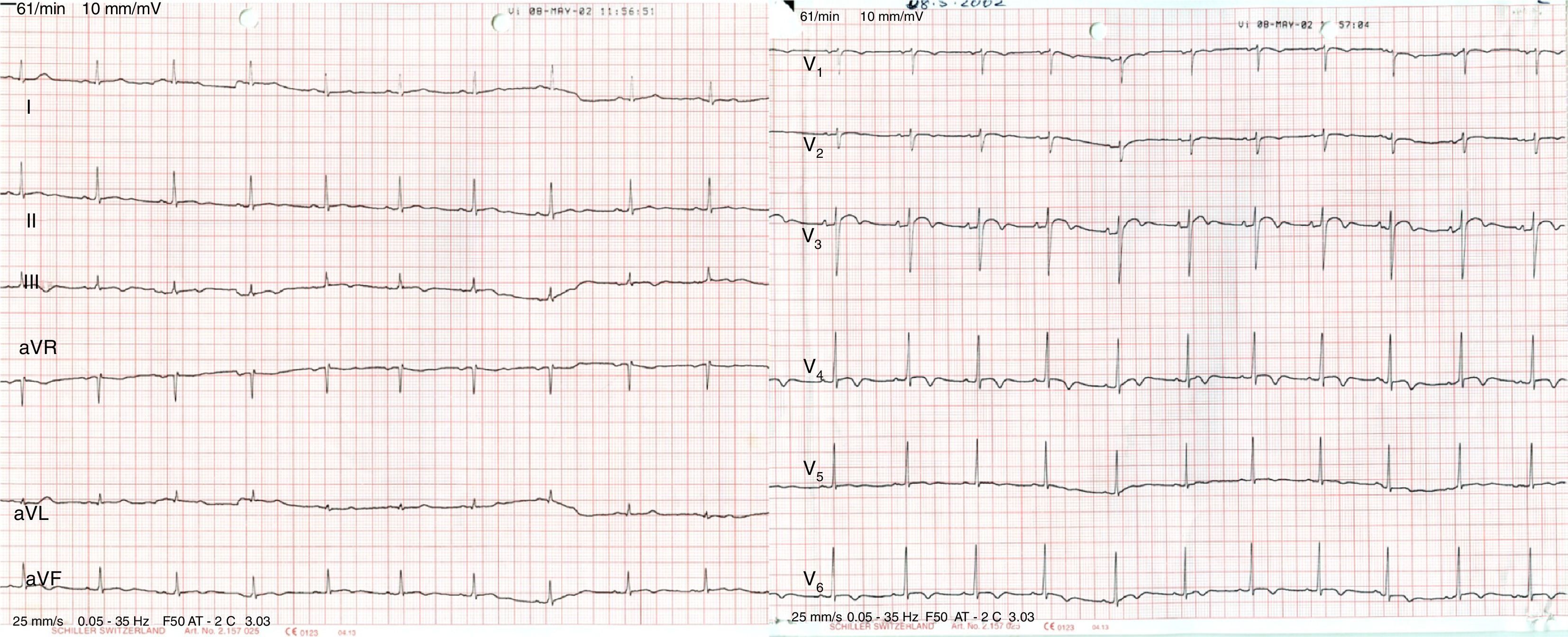
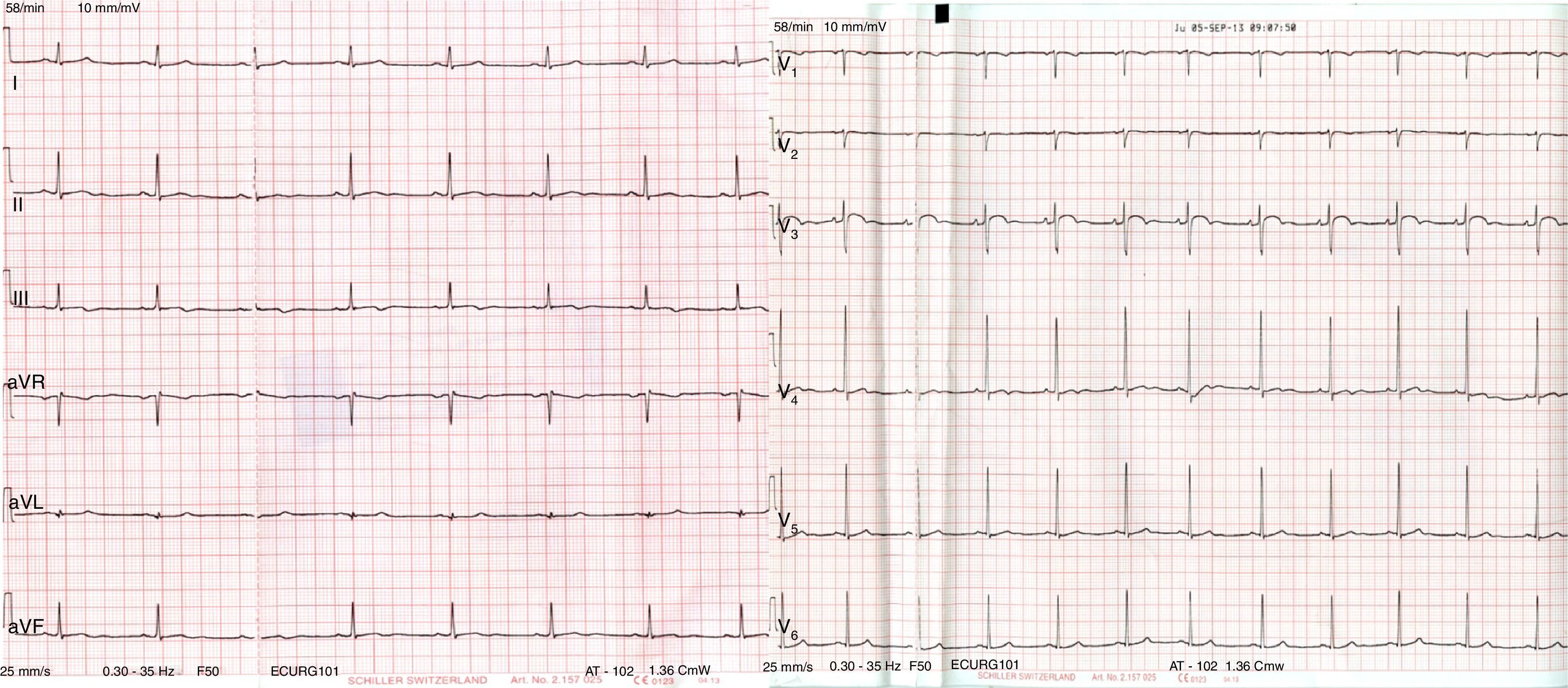
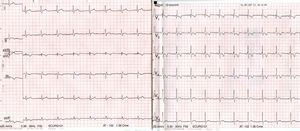
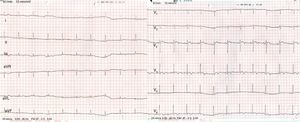
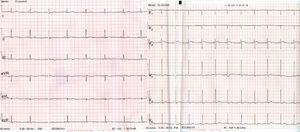
Case reportA 56-year-old patient with no prior history of interest went to the emergency department following a fall from a bicycle and direct impact to the chest at the central sternum with the bicycle handlebars. On admission, the patient was alert and oriented, and his respiration and haemodynamics were stable. He only presented with mild pain on palpation in the lower sternal region, with no other associated signs or symptoms. An ECG on arrival showed a complete right bundle branch block with T wave inversion (V1–V4) (Fig. 1) compared to an asymptomatic prior ECG (Fig. 2); his myocardial enzymes showed no abnormalities (troponin I: 0.10ng/ml). A chest X-ray showed a simple sternal fracture of the distal third of the sternal body. He remained in observation, and after 8h had elapsed since his admission, a minimum of enzymes started (troponin I: 0.42). After 24h, peak enzyme elevation was reached (troponin I: 0.52). An echocardiogram was requested, which showed preserved ventricular function. A chest CT scan confirmed the findings of a fracture of the distal third of the sternum with no associated injuries. He was admitted for observation and follow-up to the intensive care unit for 48h with a diagnosis of myocardial contusion, and subsequently to the cardiology unit. He progressed favourably and a follow-up ECG demonstrated electrocardiographic improvement (Fig. 3). The patient was discharged after 4 days and is currently in follow-up at a cardiology outpatient clinic.
Blunt cardiac trauma (BCT) encompasses a spectrum of diseases ranging from clinically silent, transitory arrhythmias to fatal myocardial wall rupture. It includes commotio cordis, which refers to sudden cardiac arrest following sternal trauma in the absence of structural heart disease or structural damage to the heart. The most common form is “cardiac contusion”, which remains a subject of considerable debate. The absence of a clear definition and the fact that there is no accepted gold standard in complementary tests make diagnosing cardiac contusion difficult. Important considerations in blunt cardiac trauma include arrhythmias and cardiac motion abnormalities that may be as serious as cardiogenic shock or rupture of a valve, septum, ventricular wall, septal wall or atrial wall.1,2
Regarding its epidemiology, its true incidence is difficult to estimate owing to the great deal of variability in its definition, and ranges from 0% to 76% in patients with blunt cardiac trauma.3 It is associated with up to 20% of road traffic deaths.4
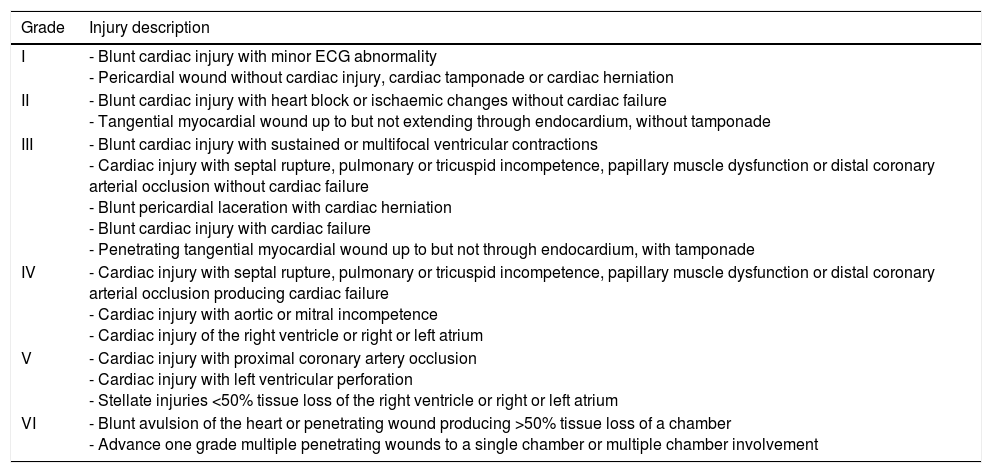
The incidence of BCT is unknown and estimates vary widely. Cases of BCT diagnosed as “myocardial contusions” or “cardiac contusions” are the most common. However, each of these terms has been used to refer to a wide range of heart injuries. The absence of clear diagnostic criteria and the lack of reliable diagnostic tests make presenting reports difficult. Symptoms suggestive of BCT may actually be unrelated to BCT, while some injuries may be clinically asymptomatic. In addition, some of the criteria used to define significant BCT, such as arrhythmias, may be due to the effects of polytrauma in a susceptible patient (for example, a patient with pre-existing heart disease). Other diagnostic criteria such as troponin elevation may occur in polytrauma not involving the chest.5 Given the ambiguity shrouding the terms “myocardial contusion” and “cardiac contusion”, it is preferable to describe BCT in terms of specific injuries (for example, septal rupture or myocardial infarction) or cardiac dysfunction (for example, decreased contractility in the absence of arrhythmia or haemorrhage). Cardiac rupture is the most devastating type of BCT because the majority of patients who experience heart chamber rupture do not make it to the emergency department. Although it is not widely used in emergency medicine, the heart injury scale developed by the American Association for the Surgery of Trauma is easy to use, applies to both blunt trauma and penetrating injuries, and provides a standard framework for research and documentation (Table 1).5 According to this scale, the final diagnosis would be type II blunt cardiac injury with heart block or ischaemic changes without cardiac failure.
Heart injury scale developed in 1994 by the American Association for the Surgery of Trauma (AAST) and its Organ Injury Scaling (OIS) Committee with six levels to objectify the severity of cardiac trauma.
| Grade | Injury description |
|---|---|
| I | - Blunt cardiac injury with minor ECG abnormality - Pericardial wound without cardiac injury, cardiac tamponade or cardiac herniation |
| II | - Blunt cardiac injury with heart block or ischaemic changes without cardiac failure - Tangential myocardial wound up to but not extending through endocardium, without tamponade |
| III | - Blunt cardiac injury with sustained or multifocal ventricular contractions - Cardiac injury with septal rupture, pulmonary or tricuspid incompetence, papillary muscle dysfunction or distal coronary arterial occlusion without cardiac failure - Blunt pericardial laceration with cardiac herniation - Blunt cardiac injury with cardiac failure - Penetrating tangential myocardial wound up to but not through endocardium, with tamponade |
| IV | - Cardiac injury with septal rupture, pulmonary or tricuspid incompetence, papillary muscle dysfunction or distal coronary arterial occlusion producing cardiac failure - Cardiac injury with aortic or mitral incompetence - Cardiac injury of the right ventricle or right or left atrium |
| V | - Cardiac injury with proximal coronary artery occlusion - Cardiac injury with left ventricular perforation - Stellate injuries <50% tissue loss of the right ventricle or right or left atrium |
| VI | - Blunt avulsion of the heart or penetrating wound producing >50% tissue loss of a chamber - Advance one grade multiple penetrating wounds to a single chamber or multiple chamber involvement |
The electrocardiogram (ECG) is a test of choice that is more relevant for haemodynamically stable patients with BCT. An ECG consistent with BCT may reveal persistent sinus tachycardia, a new bundle branch block or ST depressions or elevations.6,7 It may be difficult to determine whether the abnormality is a primary event (for example, an acute coronary syndrome that preceded trauma), a direct result of a cardiac injury or a problem caused by the physiological stress of severe trauma. A major retrospective study found that patients with a diagnosis of BCT have two to four times the initial risk of arrhythmias, depending on patient age, compared to paired controls who experienced polytrauma without any cardiac trauma.8
In summary, the following must be looked for on the ECG9:
- -
New arrhythmias including ventricular fibrillation, ventricular tachycardia, ST segment changes and new bundle branch blocks.
- -
It is not so sensitive for right ventricle damage although it has been demonstrated that right ventricle leads are not useful (1).
- -
Left ventricular contusions may have ST segment abnormalities.
- -
The majority of ECG disorders in BCT are non-specific.
- -
In a geriatric patient, pre-existing heart disease must always be considered, and therefore a baseline ECG must be obtained for comparison.
A simple chest X-ray study does not provide any information on cardiac involvement, although it is required to rule out associated chest diseases such as pulmonary contusion or multiple fractures of the ribs or sternum which could serve as an alert to the possibility of a cardiac injury. Echocardiography may provide important information for patients who show signs consistent with significant BCT, but contributes little to the management of haemodynamically stable patients with no arrhythmia. An echocardiogram is requested in all patients with unexplained blunt chest trauma and persistent shock out of proportion with apparent injuries despite aggressive resuscitation, and in any patient with signs consistent with significant BCT. The echocardiogram reveals localised haematomas, aneurysms, fistulas, pericardial effusion, short circuits, regurgitating lesions and cardiac ruptures, and analyses the myocardium's overall and segmental contractility, since contractility abnormalities are relatively common in cardiac contusion. Given that many patients with chest trauma have a poor transthoracic window, transoesophageal echocardiography is essential in the diagnostic process and, unlike other imaging techniques, may be done at the patient's bedside.
The usefulness of cardiac biomarkers in BCT is unclear.10,11 In the absence of haemodynamic instability, signs of serious injuries or an abnormal ECG, several observational studies have suggested that high CK-MB or cardiac troponin levels is non-specific for detecting the presence of a clinically significant BCT and has little prognostic value. Moreover, high troponin levels are more common in patients with significant chest trauma. The latter finding may be due to stress induced by catecholamines, hypovolaemic shock with reperfusion injury, oxidative damage, bacterial or viral toxins, or microcirculatory dysfunction. For these reasons, cardiac biomarkers are not routinely obtained in patients without haemodynamic instability, signs of serious lesions or an ECG with significant abnormalities. While some studies have suggested that biomarkers are sensitive indicators of BCT, whether or not such damage is significant in patients with no clinical signs or symptoms remains unclear.4 The most recent studies have shown that the ECG alone is insufficient to rule out myocardial damage; this is based on data from prospective studies12–14 of 500 patients. The majority of these studies have shown that adding troponin increases the negative predictive value to 100%. In summary, we believe that troponins must be obtained on arrival at hospital,10,15,16 that they have a positive predictive value (21–48%) and a negative predictive value (93–94%), and that when they are combined with a normal ECG their negative predictive value increases to 100%. A more recent study17 in 993 patients with BCT demonstrated that patients with positive troponin, although it represents a challenge in patients with polytrauma, tend to have a worse prognosis even in the absence of clinical evidence of acute cardiac damage, and therefore reflects the severity of both cardiac and extrathoracic damage.
Diagnostic and therapeutic approach to BCT in the emergency departmentPre-hospital management depends on the symptoms and severity of a patient's disease. Pre-hospital care must treat patients with potential serious cardiac injury in accordance with advanced trauma life support principles, and special attention must be paid to the patient's airway, respiration and circulation. Rapid transport to the nearest trauma centre is crucial; interventions that cause unnecessary delays must be avoided. The role of the emergency physician is to identify and implement the protocol for polytrauma, to identify patients with potential BCT and to start suitable consultations and tests swiftly. The physician must perform an emergency ultrasound in accordance with the FAST or E-FAST protocol with a cardiac study. The FAST protocol with a cardiac component has been demonstrated to be cost-effective for patients with BCT and hypotension but not for normotensive patients.18
If there is persistent shock with no apparent lesions despite aggressive resuscitation, an echocardiogram will be better to identify wall movement abnormalities and valve disorders. The fact that haemorrhage remains the main cause of traumatic shock must be borne in mind, and other common non-cardiac causes of shock must be considered (for example, tension pneumothorax). While controversy on the role of biomarkers continues, a troponin test is not routinely conducted in a stable patient with blunt chest trauma in the absence of significant ECG abnormalities, symptoms suggestive of ischaemia or age <60 years. If such criteria are met then it is reasonable to conduct a troponin test on arrival and four to six hours later.
The therapeutic approach to be taken with this type of patient will depend on the patient's haemodynamic compromise. In cardiac contusion with no haemodynamic repercussions, an approach that includes complete rest, electrocardiographic monitoring and symptomatic treatment must be taken. The patient's haemodynamic conditions may require the administration of inotropics and even the insertion of an intra-aortic counterpulsation balloon. Antiarrhythmic drugs must be administered in the presence of arrhythmias secondary to cardiac involvement, and anticoagulation must be started in the presence of an intraventricular thrombus. Surgery must be contemplated when there is tamponade due to pericardial or haemopericardial effusion resulting from a cardiac or coronary-artery rupture, a need to close a fistula or a serious valve lesion with haemodynamic instability.
Regarding predictors of mortality, a recent 8-year retrospective study of 117 patients demonstrated greater mortality in patients with high troponin levels, increased lactate levels and hypotension. It is therefore important to correct hypotension and lactate levels.19 A multi-centre retrospective study using data from 47,580 patients in trauma registries in Germany and several European hospitals identified sternal fractures as an important predictor of BCT, as in the reported case.20
ConclusionsThe diagnosis of BCT remains a challenge but must be considered in patients with a significant traumatic mechanism. Currently there is no single test to diagnose or rule out BCT. What is important is to identify patients with significant BCT and limit costly and unnecessary tests. The number of tests required for hospital discharge has not been defined in the literature. The ECG remains the initial option. The role of troponin is less clear; however, when added to a normal ECG, it provides a NPV of 100%, which would avoid unnecessary costs and stays on intensive care units. In the future, CT scan use may change the way we distinguish between traumatic or ischaemic lesion, given the importance of distinguishing between a traumatic lesion superimposed on a pre-existing morbidity, as in this case the treatment for an acute coronary syndrome and the treatment for cardiac trauma are completely different.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNone.
Conflict of interestThe authors declare that they have no conflicts of interest.