To study the causes and outcomes of patients with interprosthetic femoral fractures.
Material and methodsA retrospective review conducted on 7 patients treated between 2010 and 2013. The knee arthroplasties had been implanted for at least 5 years, and those of the hip less than a year. They were bipolar cemented in 6 patients and totally non-cemented in one patient, all of them implanted due to a displaced femoral neck fracture. They were treated using osteosynthesis with angular stability plate covering the whole interprosthetic femoral segment. Except for one patient, all have been reviewed at least 12 months.
ResultsThe patients included 6 women and one man, with a mean age of 84.7. The fracture, always by low energy, occurred between 2 and 8 months after that of the hip without the implants being mobilised. Four of them were located at diaphyseal level, and 3 at supracondylar level, and unrelated to the type of knee implant. There was consolidation in all patients at a mean of 4.5 months, without a re-operation in any of them, and with no mortality during the follow-up period. All patients walked independently at the time of the fracture, and all of them have managed to return to walking independently, having lost as average 20° of knee flexion in cases of supracondylar fracture.
ConclusionsThe most important factors in our patients regarding the producing of the fracture have been the changes in the ability to walk after knee replacement and bone fragility. Angular stability plates give good results in the treatment of interprosthetic femoral fractures.
Estudiar las causas de producción y resultados en los pacientes tratados con fractura interprotésica femoral.
Material y métodosRevisión retrospectiva de 7 pacientes tratados entre 2010 y 2013. Las artroplastias de rodilla tenían al menos 5 años desde su implantación y las de cadera menos de un año siendo cementadas bipolares en 6 pacientes y total no cementada en un paciente, implantadas todas por una fractura desplazada del cuello femoral. Han sido tratadas mediante osteosíntesis con placa de estabilidad angular abarcando todo el segmento femoral interprotésico. Excepto un paciente, los demás han sido revisados 12 meses como mínimo.
ResultadosHan sido 6 mujeres y un hombre con edad media de 84,7 años. La fractura, siempre por baja energía, se ha producido entre 2 y 8 meses tras la de cadera sin encontrarse movilizados los implantes, estando localizadas 4 de ellas a nivel diafisario y 3 a nivel supracondíleo, sin relación con el tipo de implante de rodilla. Se ha producido la consolidación en todos los pacientes a los 4,5 meses de media sin reintervención en ninguno de ellos y sin mortalidad en el tiempo que han sido controlados. Todos los pacientes deambulaban en carga en el momento de producirse la fractura y todos ellos han conseguido volver a deambular en carga, habiendo perdido como media 20° de flexión de rodilla en los casos de fractura supracondílea.
ConclusionesLos factores más importantes en nuestros pacientes con respecto a la producción de la fractura han sido la alteración de la capacidad de deambulación tras la artroplastia de cadera y la fragilidad ósea. La placa de estabilidad angular concede buenos resultados en el tratamiento de las fracturas interprotésicas femorales.
Interprosthetic femoral fractures occur in the femoral segment between hip and knee arthroplasties.1 These arthroplasties affect how the fractures occur and how they are treated.1,2 They only constitute 1.26% of femoral fractures3 but the increase in life expectancy and prosthetic surgery procedures result in a larger at-risk population and therefore their greater frequency is to be expected. These are not optimal patients since, as they present limited bone stock,3 it is difficult to stabilise fractures due to prosthetic implants4 and there is occasionally the presence of medullary canal cement which creates problems with biological union.1 In other words, treatment of these fractures poses mechanical and biological challenges. The fractures are always produced by low energy mechanisms, the effect of implants and their features, the effect of the presence and constriction of the knee implant5 and the degree of osteoporosis6 are discussed in clinical and biomechanical studies. Because these fractures are so infrequent, the published series are short with a modest number of patients1–5,7–9 and various materials and osteosynthesis techniques have been used for their treatment, sometimes with a high complication, reoperation and failure rate.10 Lateral angular-stable plates have been recommended for the treatment of these fractures, to cover the entire interprosthetic femoral segment in order to prevent the risk of fracture due to increased stress in the segment of femur without implant,2–5,7,8,11 but there is no definitive algorithm for the treatment of these fractures.7 In this short patient series, our aim is to study the causes of these fractures, the features of the patients in whom they occurred and the outcomes achieved using a single lateral angular-stable plate.
Material and methodWe undertook a retrospective review of patients treated between the years 2010 and 2013 with interprosthetic femoral fracture. There were 7 patients in the study, we studied their demographic characteristics, age and gender, causes of fracture, type of fracture according to Platzer's radiological classification,2 degree of osteoporosis using the Singh index12 measured in the contralateral hip, anaesthetic risk (ASA), time since the arthroplasty implant, union time, ambulation, general and local complications, reoperations, relationship of the type of implant with the type of fracture and clinical deterioration of joint function.
All the patients have been treated surgically with spinal anaesthesia with reduction and internal fixation with an angular-stable plate. Scheduled surgery was performed on average 2.5 days from occurrence of the fracture, overlapping the femoral stem of the hip implant between 3 and 10cm, placing 3 percutaneously and 4 by open surgery. The plate was stabilised with screws using accessory wires in the proximal segment depending on the fracture line. None of the hip or knee implants had been revised and no autologous or allografts had been used in any of the cases.
All the patients were kept non-weight bearing on the fractured limb until union of the fracture, physiotherapy was started immediately postoperatively. The fracture was considered to have healed if clinically the patient could walk independently with no pain and two radiological projections showed fracture callus. Delayed fracture union was considered if at 6 months there had been no fracture union but there had been some progress towards it since the last follow-up X-ray, and pseudoarthrosis if no union had taken place at 9 months with no progress towards it within the past 3 months.7 Union with an angle greater than 5° was considered non-union.
All the patients were monitored as outpatients until clinical and radiological union of the fracture, the minimum follow-up period was 12 months, except one patient who was lost to follow-up after 6 months.
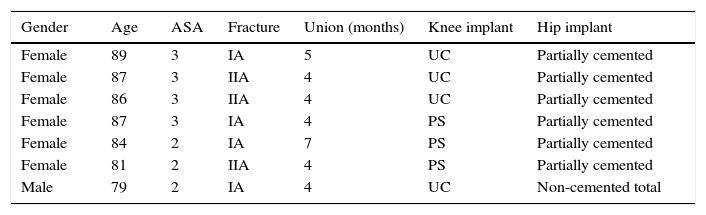
ResultsSix of the 7 patients treated were females and one male, with a mean age of 84.7 years (range 78–87). All the patients had undergone knee arthroplasty due to gonarthrosis at least 5 years prior to incurring the fracture. Ultracongruent polyethylene was used in 4 patients and posterior stabilised polyethylene in 3. Furlong®-type partially cemented bipolar hip arthroplasty was performed on 6 patients (the females) and total non-cemented hip arthroplasty on one (the male) due to displaced, low-energy cervical fracture. All of the hip arthroplasties, except the total arthroplasty, and 4 knee arthroplasties were implanted in our department (Table 1).
Gender, age, ASA, fracture type (Platzer), radiological union, type of knee implant (ultracongruent, posterior stabilised), and type of femoral implant.
| Gender | Age | ASA | Fracture | Union (months) | Knee implant | Hip implant |
|---|---|---|---|---|---|---|
| Female | 89 | 3 | IA | 5 | UC | Partially cemented |
| Female | 87 | 3 | IIA | 4 | UC | Partially cemented |
| Female | 86 | 3 | IIA | 4 | UC | Partially cemented |
| Female | 87 | 3 | IA | 4 | PS | Partially cemented |
| Female | 84 | 2 | IA | 7 | PS | Partially cemented |
| Female | 81 | 2 | IIA | 4 | PS | Partially cemented |
| Male | 79 | 2 | IA | 4 | UC | Non-cemented total |
Interprosthetic femoral fractures. Treatment with an angular-stable plate.
PS: posterior stabilised; UC: ultracongruent.
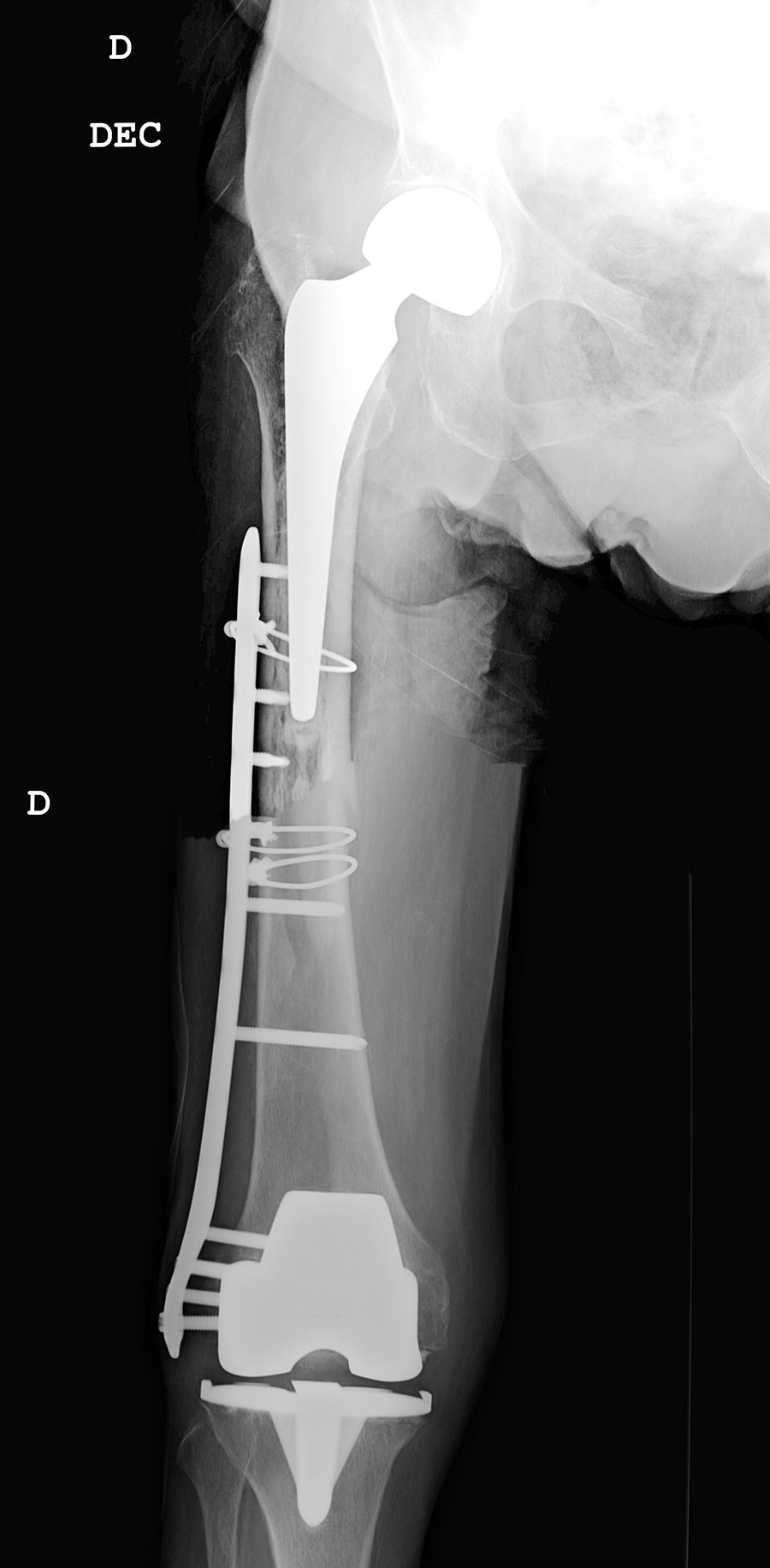
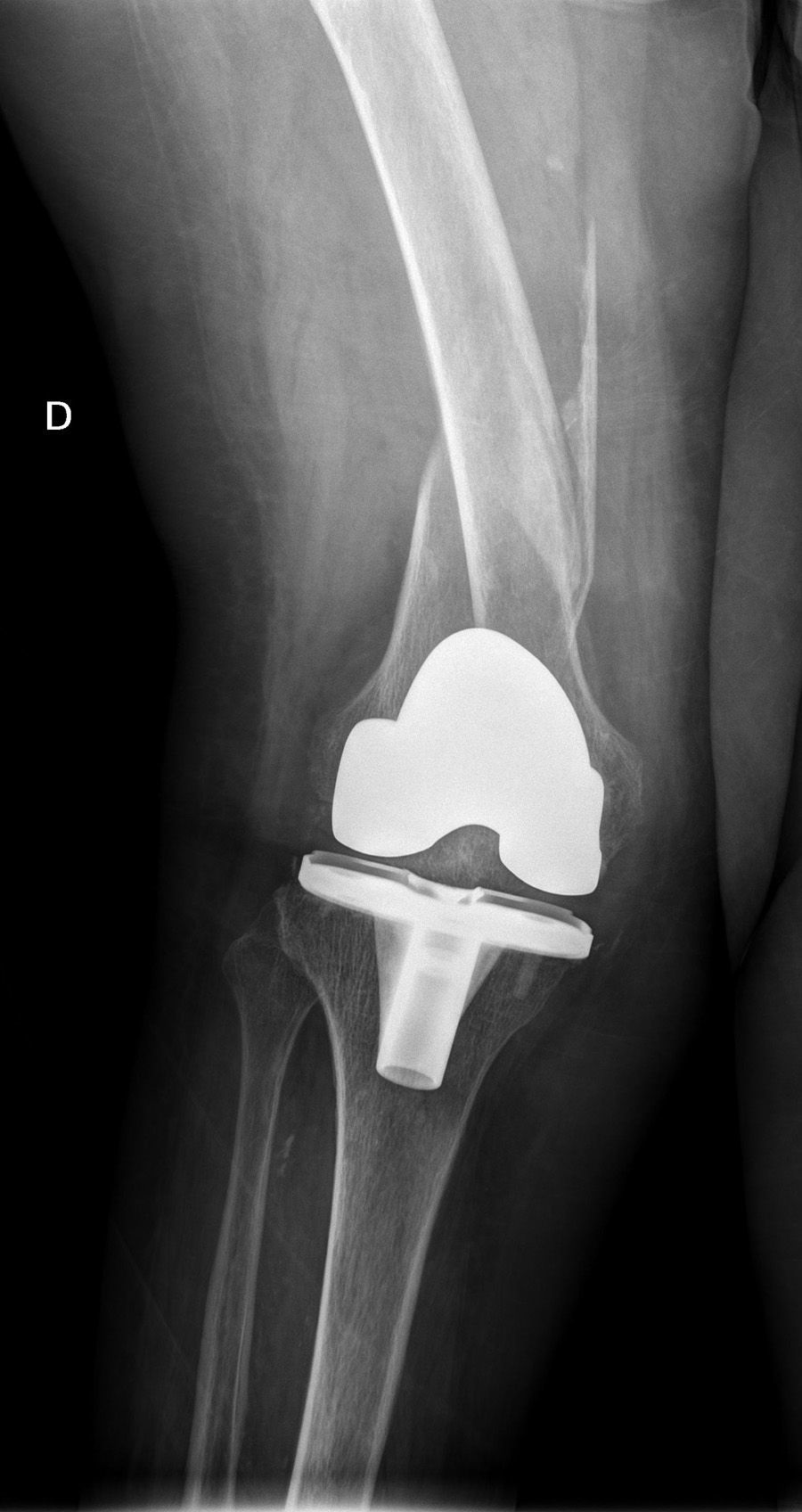
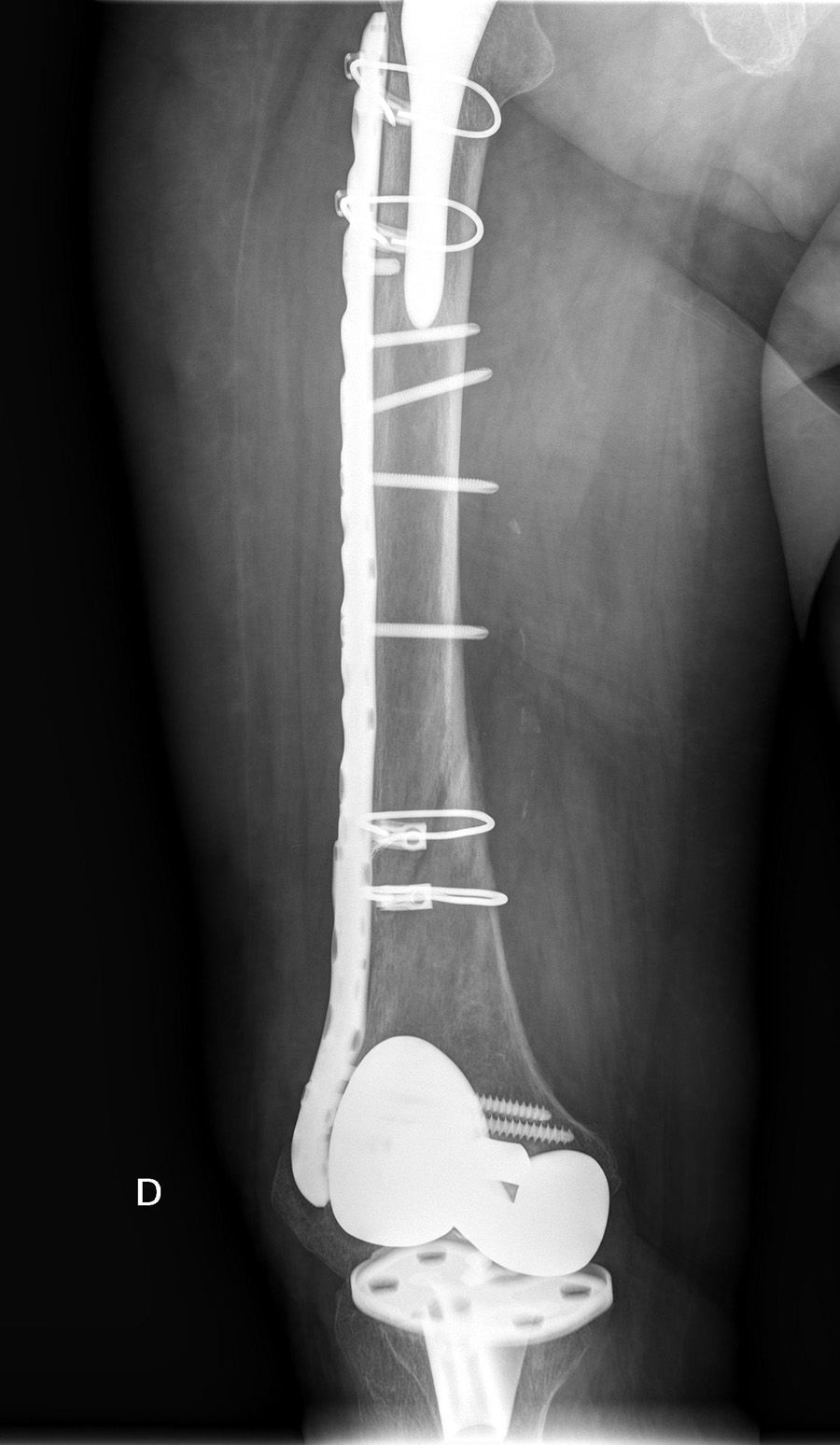
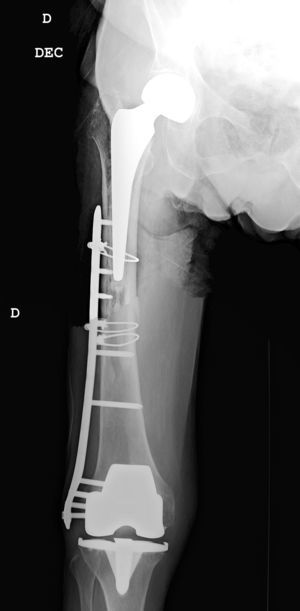
The interprosthetic fractures occurred between 2 and 8 months after the hip surgery, all of them were low-energy produced. In four cases they were located at diaphyseal level and in three at supracondylar level, two with ultracongruent and one with posterior stabilised polyethylene. In all cases both implants were stable and not affected by the fracture line. In two cases the fracture line affected the distal cement plug of the hip arthroplasty (Fig. 1). Following Platzer's classification, the fractures were 4 type IA, and 3 type IIA adjacent to the knee arthroplasties (Figs. 3 and 4). Four patients were assessed with a Singh index of 3 and 3 with an index of 4.
Four patients presented an ASA class II due to their background and general condition, and 3 ASA III. None of the patients died during the follow-up period.
All of the patients walked with the aid of orthopaedic devices prior to the fracture, 3 with a walking frame and 4 with crutches. Union took place in all cases with a mean of 4.5 months,4–7 two of them had diaphyseal fractures with delayed union. There were no angles in union greater than 5°, no reoperations or complications or evolutionary complications presented, even in one patient with a short plate which only overlapped 3cm who made satisfactory progress (Fig. 2). All the patients regained their walking ability prior to the fracture except for one female patient who was lost to follow-up at 6 months, the fracture having healed. Clinically, the three patients with a supracondylar fracture lost a mean of 20° knee flexion, previous hip mobility was not altered in any of the patients.
DiscussionInterprosthetic fractures are rare in orthopaedic surgery departments, therefore publications referring to them are also scarce, and there is little information available on how they occur, the features of the patients who suffer them, the most appropriate treatment or the final outcome. The treatment of 141 patients has been published, the majority in the past 4 years1–5,7–9,11 which is an indication both of the rise in their frequency due an increase in life expectancy and arthroplasty surgery, and the growing interest in their resolution due to the therapeutic difficulty they pose.
These are fractures that are typical in the elderly, much more common in women9 and almost always low-energy produced,11 these features were also evident in our study.
The fractures occur in association with hip and knee implants which affect both their occurrence and their location,11 in some series they are more common at supracondylar level close to the knee arthroplasty8 although not in others,7 and not in our study. At this distal location, their occurrence has been associated with constrained knee implants,5 and although this is clinically logical to an extent, it has not been demonstrated in biomechanical studies.13
There are differing options regarding the influence of the stability of the implants in the occurrence of these fractures. According to Hou et al. of the 13 cases they present, 4 presented loosening of one of the prostheses,4 although most published series find no relationship between the fractures and implant loosening because all of them were stable.1,3,8 it is not clear whether the hip prosthesis being cemented or non-cemented affects occurrence of these fractures,1 or whether it is a total hip prosthesis or hemiarthroplasty. The fact that the arthroplasty has been revised or changed1 might have an influence, but this is not the case for knee arthroplasty because almost all cases published were primary arthroplasties.
In an experimental study with cadaver femurs, Lehmann et al. found that the greatest risk of fracture was if the patient had a hip arthroplasty and a retrograde intramedullary nail and the risk of fracture did not increase if the patient had a knee arthroplasty, even if the knee arthroplasty was constrained.13 These outcomes might change the concept of interprosthetic fracture, fractures occurring in patients bearing two femoral prostheses, whether or not they are arthroplasties, should be considered, since distal femoral implants such as a retrograde nail or a short plate, affect the occurrence of fractures more than the presence of a knee arthroplasty.13 If we take this concept into account, the number of fractures produced in femurs with two implants would increase considerably. This study clearly applies in terms of the treatment to be given, so that when a distal femoral fracture occurs in a bearer of a hip arthroplasty, a retrograde implant should not be used in their treatment, but preferably an extramedullary implant.13 The femoral area between two intramedullary femoral implants, is an area that logically should be at high risk of fracture due to an accumulation of stress, as has been documented in a few cases,5 and the size of this area between implants would seem likely to affect the occurrence of a fracture, so that the smaller the gap the greater the risk, because there is a greater concentration of force in this area. Segal et al. in an experimental study using artificial bones into which they implanted a cemented hip arthroplasty and a revision knee arthroplasty, found that if the gap was kept between 5 and 20cm it did not affect fracture occurrence.14
In our series, the arthroplasties, both hip and knee, were primary, cemented except for one case and stable, 4 cases were located in the diaphyseal segment without involvement of the implants and 3 cases were adjacent to the knee arthroplasty, ultracongruent polyethylene was used in two of them: in other words, implant loosening, prosthetic revision surgery, or constrained knee implant had no effect. All our patients were bearers of hip arthroplasties implanted due to a fracture; a fact that might have more influence than the type of implant, their advanced age and the indication for a cemented implant, in most cases, patients with poorer bone stock who have already suffered at least one osteoporotic fracture. All our patients had bone fragility with low Singh indices. The fact that the fracture occurred a few months after the hip fracture would indicate the functional limitations generated after the fracture which led to a fall and the consequent fracture, which does not occur after implantation of a knee or hip arthroplasty due to degenerative disease. The influence of femoral hip prosthetic implants in our series was much more fundamental than knee arthroplasty; all of them implanted several years before the fracture occurred. The influence of the degree of osteoporosis has already been noted by Lesaca et al. who, in an experimental study, found the cortical thickness in the interprosthetic femoral segment to be the most important and decisive factor in the occurrence of interprosthetic fractures.
Variants of the Vancouver and de Lewis and Rorabeck classifications have been applied in order to adapt them to interprosthetic fractures.1,4,5,7 Platzer et al. specifically classified these fractures as type I when the fracture is remote from both implants, type II adjacent to one implant and type III adjacent to both implants. These are further subdivided into type A, both components stable, type B, one loose component, B1 hip and B2 knee, and type C, both components loose. The frequency of one or other type was 17% type I and III and 66% type II.2 Seventy-five percent had stable components and one or both components were loose in only 25%.2 In our series all of the patients presented stable implants and none of the fractures affected the implants, although the supracondylar fractures were adjacent to the knee arthroplasties, and in two cases were affecting the cement distal to the femoral hip implant, 4 cases were classified as type IA and 3 type IIA.
Treatments carried out a decade ago resulted in a great many failures. Kenny et al. in 1998 published 4 cases stabilised with the techniques available at the time and the treatment failed in all 4 patients, some of them eventually had an amputation above the fracture.10 Different types of treatment have been used, retrograde nails, nail plates, dynamic condylar screws, allografts, cerclage wiring, prosthesis revision surgery,2,4 tumour prostheses,15 etc., but there is no standard treatment since this is determined by the characteristics of the fracture, the presence of implants, the time since they were placed, the occasional presence of cement, bone quality, the patients’ age and features, etc. These factors can affect mechanical stability4 and the biology of fracture union.1 Given these constraints, treatment should be personalised.11
The treatment objectives are to restore femoral length and rotation, ensuring the functionality of the arthroplasty and to achieve sufficient stabilisation to enable early mobilisation, providing the fracture the biomechanical features necessary for its union. Currently the most used material, when the implants are not loose,4,9 are angular-stable plates, which has revolutionised the treatment in increasing stability of fixation, especially in osteoporotic bone, with minimum aggression to soft tissues.1,2,4,5,8 The plate should cover the entire interprosthetic femoral segment5,7,8,11 from distal to proximal3 and the screws should be fixed in at least 8 femoral cortical bones in the proximal segment using a cerclage or wire11 accessory to increase the stability of the screws. Cerclages, as they do not provide rotational stability,1 should not be used for the main or primary fixation of the plate, but rather as a complementary system to screws to provide greater stability and to be placed in the most proximal area of the plate.1 Hou et al. indicate that the plate used should overlap the intramedullary femoral implant by at least two femoral diameters to prevent areas of stress,4 i.e., between 6 and 8cm. In our series the overlap was between 3 and 10cm, no failures occurred as a result of limited overlap in some. Some authors1,3,8 use locked plates with the same concepts, but introduced by minimally invasive or percutaneous surgery, offering the advantages of preserving fracture haematoma and reducing injury to soft tissues to a minimum. Union is achieved using these treatments in between 80 and 100%1,2,7,8 of the cases treated, very much depending on good technical surgery.1
Ochs et al. based on Platzer's classification, created a therapeutic algorithm in which, depending on the type of fracture and the stability of the implants, they indicate treatment with angular-stable plates or prosthesis revision surgery.16 If knee revision implants with intramedullary stem are used, a complementary osteosynthesis plate should be added to prevent areas of stress between the two intramedullary implants.5
We have followed the abovementioned criteria, using a single lateral angular-stable plate in all cases covering the entire interprosthetic femoral segment, achieving union in all cases with no reoperations or failures. The only problem that we found was achieving an adequate overlap of the osteosynthesis plate to the femoral hip implant, since the reduced availability of plate lengths means that occasionally we have to make a rather limited or excessive overlap; a choice has to be made between one or the other.
A wide approach and femoral bone removal are required in order to place a graft, and therefore their use is disputed. Spongy bone allografts have occasionally been used in the fracture site,1 but the use of allografts in palisade,9 seeking to increase fracture stability and long-term increase of bone quality or stock, is exceptional due to the good stability provided by angular-stable plates.
Another point of discussion is mortality. These are serious, high-risk fractures in the elderly patient. To a greater or lesser degree, the majority of published series report mortality,2–5,7 it is difficult to establish rates due to the limited number of patients included in these series, as in ours, with no mortality but with very limited review time, and therefore we have nothing to contribute on this point.
Our study, despite the homogeneity of the treatment, presents limitations due to the limited number of patients and because it is retrospective, but we can conclude that interprosthetic fractures are very rare, although an increase in the short-term is predicted, and has already started. The majority occur in females of advanced age, the presence of implants, the functional deterioration which occasionally presents after their placement for hip fracture and above all bone quality, are determining factors. Treatment should be personalised according to the features of the patient and the fracture but along with prosthetic implant stability, the best mechanical and biological solutions are lateral angular-stable plates that should be placed percutaneously or in a minimally invasive manner without using allografts, covering the entire interprosthetic femoral segment, overlapping the femoral hip implant between 6 and 8cm and using, if necessary, cerclages to enhance the fixation and stability of the implant in its proximal portion. Outcomes using this technique tend to be good with a high rate of union, low risk of fracture callus, and there has been a major decrease in the number of reoperations and failures.
Level of evidence IV.
Ehtical disclosuresProtection of human and animal subjectsThe authors declare that neither human nor animal testing have been carried out under this research.
Confidentiality of dataThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors declare that no patients’ data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Albareda J, Gómez J, Ezquerra L, Blanco N. Fracturas interprotésicas femorales. Tratamiento con placa lateral de estabilidad angular. Rev Esp Cir Ortop Traumatol. 2017;61:1–7.