To evaluate the influence of the medial–lateral stability of the joint on the short-term clinical outcomes after performing navigation in total knee replacement.
Material and methodsA multicentre prospective study was conducted on 111 consecutive total knee replacements performed with computer assisted surgery. The study included the evaluation of KSS, WOMAC, and SF-12 preoperatively, and at 3 and 12 months of follow-up, and correlation with stability data obtained during surgery, in extension and at 20° and 90° of flexion.
ResultsNo differences were found in WOMAC, KSS and SF-12 relative to coronal stability during surgery.
ConclusionsVariations in coronal stability were shown to have no influence on the short-term clinical results of navigated total knee replacement.
Evaluar la influencia de la estabilidad mediolateral de las artroplastias totales de rodilla implantadas con navegación quirúrgica en sus resultados clínicos a corto plazo.
Material y métodosEstudio prospectivo multicéntrico de 111 pacientes intervenidos con artroplastia total de rodilla mediante cirugía asistida por ordenador. Los resultados clínicos y funcionales se evaluaron a los 3 y seis meses mediante las escalas KSS, WOMAC y SF-12 y se correlacionaron con la información que mostraba el sistema de navegación intraoperatoriamente en cuanto a la estabilidad mediolateral en extensión, a los 20° y a los 90° de flexión.
ResultadosNo se encontró relación entre los resultados clínicos y funcionales y la estabilidad mediolateral medida intraoperatoriamente.
ConclusionesLas variaciones en la estabilidad mediolateral de las artroplastias de rodilla no han mostrado una influencia significativa en los resultados clínicos a corto plazo.
Achieving good clinical and functional long-term results in total knee arthroplasty (TKA) depends on several factors, among which we must mention a correct alignment of the implant1 and adequate balance of soft tissues. In order to obtain a balanced prosthesis it is necessary to achieve optimal varus-valgus alignment and symmetric spaces in flexion and extension.
Computer-assisted surgery (CAS) in TKA has provided a precision instrument enabling more homogenous results for the alignment in the coronal plane than those obtained using conventional instrumentation.2–4 Nevertheless, there is some controversy regarding its ability to provide a better alignment in the sagittal plane.3,4 CAS also enables the use of sequential release techniques to obtain a correct ligament balance and equalize spaces in flexion and extension.5 Although in theory this could result in a longer lifetime of the implant and better clinical outcomes, the relatively short evolution of CAS has not allowed this hypothesis to be confirmed.
The aim of this study was to determine the relationship between medial–lateral stability of TKA, quantified using navigation data, with clinical outcomes.
Materials and methodsWe conducted a prospective multicenter study comprising 111 patients who underwent TKA. Inclusion criteria were patients with knee osteoarthritis candidates for TKA without surgical contraindications. All patients signed an informed consent form. The process which determined the surgery was primary osteoarthritis in 107 cases, secondary posttraumatic arthrosis in 3 cases and rheumatoid arthritis in 1 case. Gender distribution was 34 males (30.63%) and 77 females (69.37%), aged between 44 and 85 years (mean: 69.5 years) and a mean body mass index of 32.15. The operated knee was the left in 45 cases (40.54%) and the right in 66 cases (59.46%), with involvement. According to the Ahlbäck classification,6 46 cases of partial interline impingement, 59 cases of full impingement, 3 cases of sinking of the minor tibial plateau of 5mm, and 3 cases of sinking between 5 and 10mm were found. According to the alignment detected by navigation, 73.9% of the knees presented a varus deformity (angle of 180° between the mechanical axis of the femur and tibia major), 14.4% valgus deformity (angle less than 180°) and 10.6% had a normal axis, considering this as an angle of 180°.
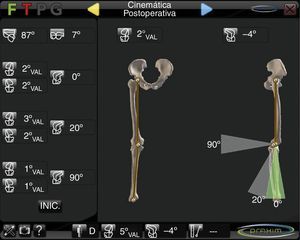
All patients underwent a total knee arthroplasty with Apex® (OMNI Lifescience, East Taunton, Massachusetts, USA), in 30 cases through a standard medial parapatellar approach with patellar eversion and in the rest through a minimally invasive, midvastus approach. In 66 cases (59.5%) we used a femoral implant with preservation of uncemented posterior cruciate ligament (CR) and in 45 (40.5%) we used a cemented posterior stabilized component (PS). In 55 cases we used CR polyethylene inserts, in 45 we used PS polyethylene inserts and in 11 cases the insert used was of the ultracongruent type. Tibial trays were cemented in all patients. The Total Knee Surgetics® system version 7.9 (PRAXIM SA, La Tronche, France) was used to perform all the surgical procedures. This is a closed navigation system, without previous images, which uses a kinematic analysis of the hip, knee and ankle and anatomical mapping of the knee to build a working model. After placing the infrared sensors on the anterior cortex of the femur and tibia and resecting osteophytes, we performed a tibial section at 90° on the mechanical axis of the tibia in the coronal plane, with 5° of posterior slope in the sagittal plane, and applying the technique of dependent cuts by sequential releases with a distractor, the femoral cuts were calculated to obtain symmetric spaces in extension and flexion of 90° with equal soft tissue tension. Once the final components were in place and the joint was closed by suture, we recorded the postoperative kinematics of the limb and quantified the flexion-extension arc and medial–lateral stability by evaluating changes in the femorotibial angle after applying varus-valgus stress maneuvers to induce joint gaping with reduction of the extensor apparatus (Fig. 1). The limit value of stability was established as a variation of 3°, establishing 2 groups for analysis of the results: Group 1, consisting of those knees showing a variation greater than 3°, and Group 2, comprising those knees presenting a variation less than or equal to 3°.
Clinical evaluation was performed in all patients preoperatively and at 3 and 12 months after the intervention. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Knee Society Score (KSS) and Short Form-12 Health Survey (SF-12) were completed in all cases. Moreover, standard simple radiographs in anteroposterior and lateral projections were obtained, as well as telemetry in standing, covering the hip, knee and ankle.
The results were evaluated using the single factor ANOVA test, comparing members of the group with variations of the femorotibial angle less than or equal to 3°, with members of the other group, both in terms of absolute change in each of the described clinical parameters and in the mean values of the assessment scales at different times during follow-up. We considered as statistically significant values of P<.05. Data processing was performed using the software package SPSS (IBM Corp. Release 2012. IBM SPSS Statistics for Windows, Version 21.0 Armonk, NY: IBM Corp., USA).
ResultsNo complications derived from arthroplasty or the navigation technique were observed. None of the patients were lost during follow-up and all patients attended the clinical review on the appointed date.
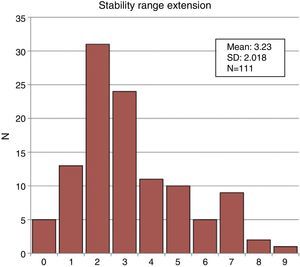
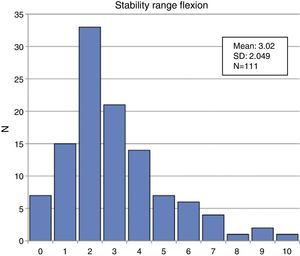
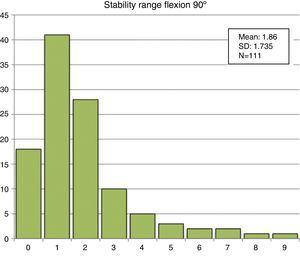
Variations in the femorotibial angle occurred linearly in all cases, that is, those prostheses showing a greater variation in size relative to the others also showed greater variation at 20 and 90° flexion. In extension, the number of knees with variations greater than 3° (group 1) was 34, and those with variations less than or equal to 3° (group 2) were 77. At 20° flexion, 35 knees were included in group 1 and 76 in group 2. At 90° flexion, 14 and 97 knees were included in the respective groups (Figs. 2–4).
Variations in the femorotibial angle measured in extension ranged between 0° and 10°, with a mean value of 3.23° and a standard deviation (SD) of 2.01°. At 20° flexion, these variations were between 0 and 10°, with a mean value of 3.02 and a SD of 2.04°. At 90° flexion, the mean value was 1.86°, with a range between 0 and 9° and a SD of 1.73°.
There were no significant differences regarding medial–lateral stability depending on the type of femoral implant or the polyethylene insert employed (Table 1).
Variation of the femorotibial angle according to the type of polyethylene insert.
| Polyethylene | n | Extension | Flexion 20° | Flexion 90° | |||
| Mean | SD | Mean | SD | Mean | SD | ||
| CR | 55 | 3.21 | 2.18 | 2.07 | 1.75 | 2.69 | 2.22 |
| UC | 11 | 3.18 | 2.67 | 1.36 | 0.80 | 3.00 | 1.94 |
| PS | 45 | 3.29 | 1.65 | 1.72 | 1.88 | 3.43 | 1.82 |
| P=.93 | P=.36 | P=.58 | |||||
CR, posterior cruciate; PS, posterior stabilized; SD, standard deviation; UC, ultracongruent.
The postoperative results and the absolute change in score for each of the WOMAC, KSS and SF-12 scales are shown in Table 2. We observed an improvement in all scales in all cases. This improvement was particularly significant when comparing the results at 3 months with those measured preoperatively and increased up to 12 months, although the differences between these last 2 periods were not statistically significant. No relationship was found between these functional and clinical results and the variation in the medial–lateral stability measured in navigation.
Mean values and absolute change obtained in each scale in extension, at 20° and at 90° flexion for each of the follow-up times assessed and in each of the groups established; variation of the femorotibial angle>3° and ≤3°.
| Follow-up | Extension | Flexion 20° | ||||||||||||
| Mean (>3°) | Mean (≤3°) | AC (>3°) | AC (≤3°) | SD (>3°) | SD (≤3°) | P | Mean (>3°) | Mean (≤3°) | AC (>3°) | AC (≤3°) | SD (>3°) | SD (≤3°) | P | |
| Functional KSS | ||||||||||||||
| Preop | 36.03 | 45.87 | 37.65 | 45.07 | ||||||||||
| Three months | 94.08 | 93.43 | 57.50 | 48.20 | 18.92 | 21.99 | 0.05 | 90 | 95.5 | 52.50 | 51.70 | 18.23 | 22.67 | 0.87 |
| One year | 98.33 | 95.42 | 70.83 | 55.00 | 11.65 | 31.12 | 0.11 | 96.88 | 97.11 | 69.29 | 60.29 | 15.92 | 27.06 | 0.42 |
| KSS | ||||||||||||||
| Preop | 26.89 | 23.97 | 22.97 | 26.06 | ||||||||||
| Three months | 77.76 | 77.47 | 51.85 | 52.40 | 13.19 | 12.27 | 0.85 | 75.39 | 78.67 | 52.15 | 52.17 | 14.17 | 11.89 | 0.10 |
| One year | 79.53 | 78.82 | 53.20 | 56.90 | 14.58 | 12.54 | 0.52 | 78.56 | 79.59 | 56.78 | 53.50 | 16.02 | 12.53 | 0.58 |
| SF-12 MCS | ||||||||||||||
| Preop | 36.02 | 37.46 | 37 | 36.9 | ||||||||||
| Three months | 54.36 | 59.59 | 20.23 | 21.09 | 13.70 | 11.61 | 0.77 | 54.67 | 58.77 | 19.33 | 21.37 | 11.44 | 13.00 | 0.50 |
| One year | 56.82 | 59.13 | 19.12 | 19.42 | 15.12 | 12.06 | 0.96 | 60.39 | 56.71 | 20.22 | 18.91 | 15.65 | 13.28 | 0.85 |
| SF-12 PCS | ||||||||||||||
| Preop | 24.17 | 25.32 | 23.29 | 25.65 | ||||||||||
| Three months | 52.4 | 51.4 | 28.22 | 25.38 | 8.45 | 11.50 | 0.23 | 50.16 | 52.69 | 26.77 | 26.54 | 8.03 | 11.31 | 0.93 |
| One year | 53.78 | 53.85 | 30.17 | 28.30 | 7.84 | 9.79 | 0.62 | 54.91 | 53.36 | 32.40 | 28.28 | 4.10 | 9.56 | 0.30 |
| WOMAC pain | ||||||||||||||
| Preop | 16.1 | 14.7 | 15.99 | 14.82 | ||||||||||
| Three months | 1.74 | 1.73 | −14.32 | −12.82 | 3.27 | 3.98 | 0.07 | 2.57 | 1.32 | −13.52 | −13.41 | 3.66 | 3.83 | 0.90 |
| One year | 0.69 | 0.5 | −15.50 | −15.17 | 3.48 | 3.41 | 0.80 | 0.33 | 0.74 | −15.67 | −15.21 | 3.74 | 3.31 | 0.75 |
| WOMAC rigidity | ||||||||||||||
| Preop | 6.54 | 6.01 | 6.66 | 5.97 | ||||||||||
| Three months | 0.6 | 0.69 | −5.91 | −5.25 | 1.44 | 1.97 | 0.09 | 1.13 | 2.42 | −5.57 | −5.52 | 1.79 | 1.81 | 0.90 |
| One year | 0.31 | 0.17 | −6.31 | −6.41 | 1.45 | 2.23 | 0.88 | 0.33 | 0.21 | −6.33 | −6.37 | 1.73 | 1.86 | 0.96 |
| WOMAC functional cap | ||||||||||||||
| Preop | 58.56 | 69.99 | 57.16 | 53.83 | ||||||||||
| Three months | 6.63 | 6.1 | −51.75 | −46.61 | 11.71 | 13.56 | 0.07 | 6.07 | 2.92 | −48.02 | −49.16 | 14.93 | 12.00 | 0.70 |
| One year | 2.75 | 2.91 | −56.18 | −53.67 | 11.95 | 16.38 | 0.64 | 2.11 | 3.16 | −57.53 | −53.94 | 11.78 | 14.81 | 0.53 |
| Follow-up | Flexion 90° | ||||||
| Mean (>3°) | Mean (≤3°) | AC (>3°) | AC (≤3°) | SD (>3°) | SD (≤3°) | P | |
| Functional KSS | |||||||
| Preop | 38.85 | 43.17 | |||||
| Three months | 90.71 | 94.27 | 51.54 | 52.04 | 24.10 | 20.80 | 94 |
| One year | 91.67 | 97.71 | 80.00 | 60.48 | 10.00 | 24.25 | 20 |
| KSS | |||||||
| Preop | 26.54 | 24.8 | |||||
| Three months | 75.92 | 77.86 | 50.67 | 52.43 | 16.26 | 11.95 | 66 |
| One year | 72 | 79.83 | 53.50 | 54.78 | 4.95 | 14.21 | 90 |
| SF-12 MCS | |||||||
| Preop | 31.89 | 37.70 | |||||
| Three months | 52.43 | 58.30 | 20.53 | 20.75 | 8.07 | 13.24 | 96 |
| One year | 42.65 | 59.15 | 21.52 | 19.04 | 20.46 | 14.47 | 81 |
| SF-12 PCS | |||||||
| Preop | 25.73 | 24.79 | |||||
| Three months | 51.16 | 51.96 | 25.43 | 26.85 | 9.51 | 10.53 | 65 |
| One year | 50.97 | 54.06 | 26.08 | 29.67 | 10.63 | 8.61 | 58 |
| WOMAC pain | |||||||
| Preop | 17.29 | 14.91 | |||||
| Three months | 2.71 | 1.55 | −14.37 | −13.29 | 2.91 | 3.88 | 35 |
| One year | 3.67 | 0.24 | −16.00 | −15.28 | 3.61 | 3.43 | 74 |
| WOMAC rigidity | |||||||
| Preop | 6.85 | 6.11 | |||||
| Three months | 0.86 | 0.62 | −5.92 | −5.47 | 1.16 | 1.88 | 40 |
| One year | 1.33 | 0.12 | −6.67 | −6.32 | 1.15 | 1.86 | 76 |
| WOMAC functional cap | |||||||
| Preop | 60.22 | 54.19 | |||||
| Three months | 9.86 | 5.67 | −49.60 | −48.62 | 13.08 | 13.07 | 80 |
| One year | 1.36 | 1.52 | −54.00 | −55.23 | 12.29 | 14.19 | 89 |
AC, absolute change; KSS, Knee Society Score; MCS, mental composite score; PCS, physical composite score; SD, standard deviation; SF-12, Short Form-12 Health Survey; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
CAS applied to TKA has provided more consistency and uniformity of results regarding the coronal alignment of the components and, therefore, the resulting mechanical axis.1–3,7 However, the influence of navigation in the short- and medium-term functional results remains controversial. Seon and Song8 observed better functional outcomes at 1 year when comparing minimally invasive surgery with CAS and conventional surgery. Spencer et al.9 and Kamat et al.10 did not observe better clinical results after 2 and 5 years of follow-up, respectively. In a prospective 5-year comparative study using navigation, Ishida et al.11 observed better alignment, greater range of motion and better specific KSS, albeit with no differences in functional KSS, thus suggesting that navigation would provide no subjective benefits for patients. However, Hoffart et al.12 also used the KSS questionnaire to show better functional results at 5 years in knees treated with CAS compared to conventional arthroplasties. Finally, Hernández-Vaquero et al.13 found no beneficial effect of navigation surgery on the KSS results at 8 years of evolution. Several meta-analyses also concluded that the use of CAS does not improve postoperative function in TKA.14–17
Several authors have studied the stability of TKA performed through standard techniques and their influence on postoperative clinical outcomes.18–20 The first work which attempted to correlate stability, clinical results and navigation was that by Song et al.21 in 2007. In a prospective study of 92 TKAs with a minimum follow-up of 1 year, these authors used radiographs under stress to compare the anteroposterior and medial–lateral stability of the resulting joint, with and without the use of navigation techniques, and concluded that there were no significant differences between both groups. The mean value of varus-valgus laxity recorded in the navigation group was 7.9° (3.5° medial+4.4° lateral), even greater than those obtained in our series, with no short-term clinical differences being observed in regard to the use of CAS. In our work, we decided to establish a limit value for medial–lateral stability of 3° to restrictively differentiate the more stable prostheses from those which were not. This was the mean value of the total laxity obtained, both in flexion and extension.
In 2009, Lüring et al.22 conducted a retrospective study with a follow-up period of 2 years in order to analyze whether navigation improved the results of the WOMAC, KSS, range of motion and alignment. By plain radiography under stress they concluded that medial–lateral stability obtained in extension and flexion of 90° was the same in both the CAS and manual groups and that there were no clinical differences between the two. The range of medial–lateral opening obtained was between 2.5 and 3.5° in extension. These values were similar to those observed in our group of patients, with a mean value of 3.23°.
The results obtained in our series, both in extension and in 20 and 90° flexion, did not present a significant influence on stability measured intraoperatively in the short-term clinical results. Despite this, and although navigation has not currently been proven to represent an effective tool to obtain better joint stability, we recommend the use of this technique in TKA as a tool enabling an objective quantification of the spaces and alignment of the limb.
Our study has some limitations. The medial–lateral force used to assess stability was applied by surgeons in a subjective and non-instrumented manner, so there could be some bias regarding this factor. Moreover, measurements were performed intraoperatively and not during clinical follow-up, so there could be some differences caused by soft tissue scarring which could have modified the range of medial–lateral stability. The evolution time was short, so a long-term evaluation of the results of this series will be required in order to assess whether there is an influence of medial–lateral stability on prosthesis survival and on clinical changes reported by patients.
Level of evidenceLevel of evidence iv.
Ethical responsibilitiesProtection of people and animalsThe authors declare that this investigation adhered to the ethical guidelines of the Committee on Responsible Human Experimentation, as well as the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that this work does not reflect any patient data.
Right to privacy and informed consentThe authors declare that this work does not reflect any patient data.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Martín-Hernández C, Revenga-Giertych C, Hernández-Vaquero D, Albareda-Albareda J, Queiruga-Dios J, García-Aguilera D, et al. ¿Influye la estabilidad mediolateral de las artroplastias totales de rodilla en la evolución clínica a corto plazo? Estudio multicéntrico a un año con cirugía asistida por ordenador. Rev Esp Cir Ortop Traumatol. 2014;58:101–107.