To evaluate the clinical and radiological results of a tantalum acetabular monoblock with a mean follow-up of 12 years.
Material methodA prospective follow-up was performed on 23 hip replacements in 23 patients. The most frequent diagnosis was primary coxarthrosis (9 cases) and avascular necrosis (7 cases). The clinical results were assessed using the Merle D’Aubigne-Postel scale. The orientation of the components, the integration of the acetabula, and the presence of post-operative hiatus, or the appearance of radiolucent lines were evaluated. The polyethylene wear was measured using the Kim method.
ResultsThe mean follow-up of the series was 12 years. All the implants were osseointegrated at the end of follow-up. The mean values of, pain, ability in walking, and mobility on the Merle D’Aubigne-Postel scale were 5.4, 5.2 and 4.4, respectively, at the end of follow-up. A post-operative hiatus had not been filled in one acetabulum, and 4 implants had non-progressive radiolucent lines in the area of the DeLee zone 1.
ConclusionsTantalum acetabular monoblocks have an excellent survival with follow-ups longer than ten years in primary hip surgery.
Valorar los resultados clínicos y radiológicos de un cotilo monobloque de tantalio con un seguimiento medio de 12 años.
Material y métodoSe siguieron prospectivamente 23 prótesis de cadera en 23 pacientes. Los diagnósticos más frecuentes fueron coxartrosis primaria (9 casos) y necrosis avascular (7 casos). Los resultados clínicos fueron valorados con la escala de Merle D’Aubigne-Postel. Se midieron la orientación de los componentes, la integración de los cotilos y la presencia de hiatos postoperatorios o aparición de líneas radiolúcidas. El desgaste del polietileno fue medido con el método de Kim.
ResultadosEl seguimiento medio de la serie fue de 12 años. Todos los implantes se encontraban osteointegrados al final del seguimiento. Los valores medios de dolor, capacidad de deambulación y movilidad en la escala de Merle D’Aubigne-Postel fueron 5,4, 5,2 y 4,4 respectivamente al final del seguimiento. En un cotilo un hiato postoperatorio no se había rellenado y 4 implantes tenían líneas radiolúcidas no progresivas en la parte de la zona 1 de DeLee.
ConclusionesLos cotilos monobloque de tantalio presentan una excelente supervivencia con seguimientos superiores a diez años en cirugía primaria de cadera.
At present, cementless fixation of the acetabular component is the most widespread in primary arthroplasty of the hip. The survival of these implants depends on a series of factors, including the material, design, manufacturing process and method of sterilization, the osteoinductive and osteoconductive properties of the implant, and on the stability of the initial fixation of the acetabular cup.1–4 Good primary stability will foster osseointegration of the acetabular cup.5
New materials and designs have been developed in an attempt to improve implant survival. In 1997, tantalum began to be used in primary hip surgery. This material has certain characteristics that make it very attractive for the development of implants for orthopaedic surgery. It has a high friction coefficient with bone, which offers an outstanding primary fixation. Second, it is a material with close to 80% porosity and a pore size of 550μm, which favours osseointegration.6–9 Third, its 3GPa modulus of elasticity is similar to that of subchondral bone (2GPa), which, in addition to facilitating the growth of bone on the implant, also makes the distribution of loads more physiological, thereby decreasing bone resorption.8–10
Monoblock components are associated with a lower rate of wear between the polyethylene and the implant. The wear particles do not have access to the fundus of the implant since there are no holes for the insertion of screws. Because it does not require a system of fixation for the insert, the acetabular component can be thinner, making it possible to implant thicker polyethylenes.10–12 The hypothesis of this paper is to determine whether the greater integration capacity of tantalum would improve the survival rate of these uncemented acetabular cups.
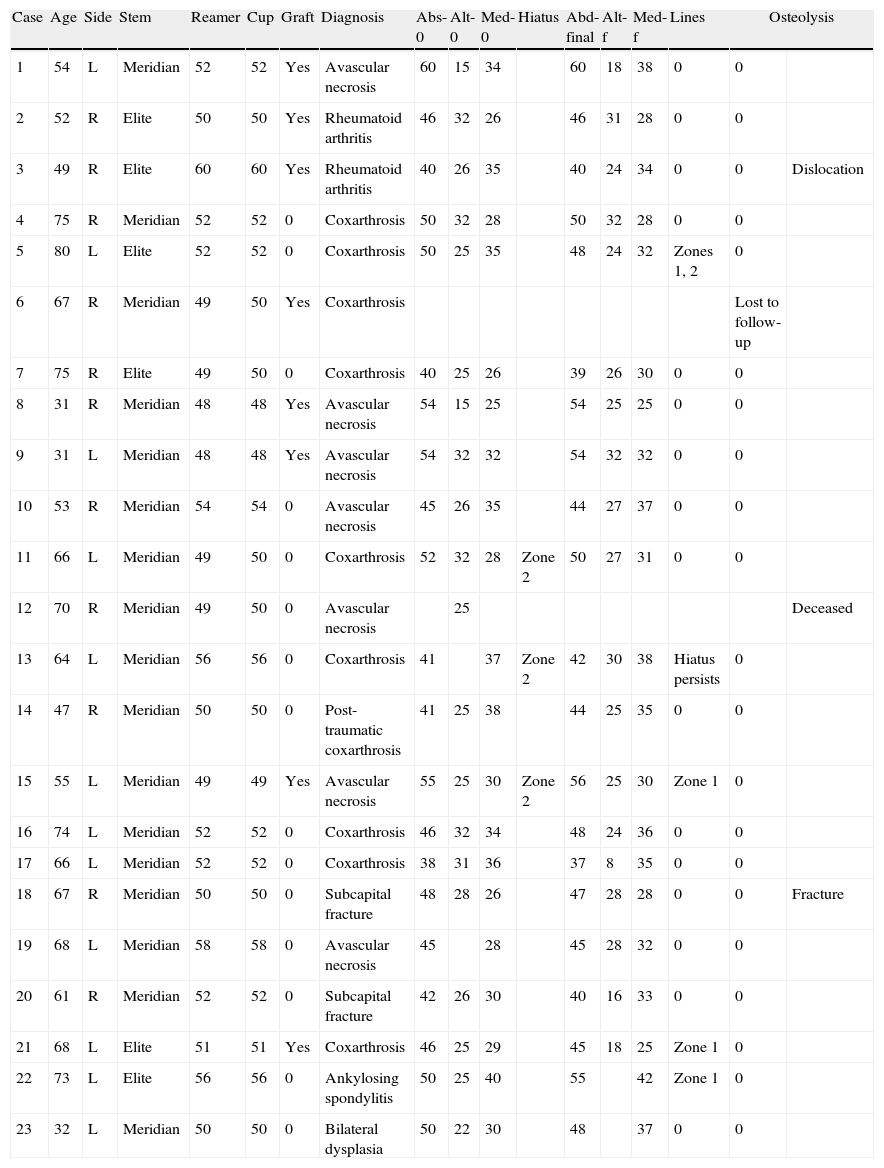
Material and methodBetween March 1998 and March 1999, one of the authors (EGG) implanted 23 Hedrocel monoblock acetabular components (Implex Corp., Allendale, NJ) in our centre as part of a prospective study. The cup used was an elliptical tantalum acetabular cup with an equatorial diameter 2mm greater than the polar diameter. The conventional polyethylene insert was compression moulded on the tantalum cup, penetrating to a depth of between 1 and 2mm, leaving 2–3mm of tantalum for the osseointegration of the implant.13 The acetabular cups had been sterilized in nitrogen with 30kGy of cobalt gamma radiation (Table 1).
Summary of the most significant values from the series studied, with differences between reaming size and the diameter of the implant used, and the association of post-operative hiatus and radiolucent lines.
| Case | Age | Side | Stem | Reamer | Cup | Graft | Diagnosis | Abs-0 | Alt-0 | Med-0 | Hiatus | Abd-final | Alt-f | Med-f | Lines | Osteolysis | |
| 1 | 54 | L | Meridian | 52 | 52 | Yes | Avascular necrosis | 60 | 15 | 34 | 60 | 18 | 38 | 0 | 0 | ||
| 2 | 52 | R | Elite | 50 | 50 | Yes | Rheumatoid arthritis | 46 | 32 | 26 | 46 | 31 | 28 | 0 | 0 | ||
| 3 | 49 | R | Elite | 60 | 60 | Yes | Rheumatoid arthritis | 40 | 26 | 35 | 40 | 24 | 34 | 0 | 0 | Dislocation | |
| 4 | 75 | R | Meridian | 52 | 52 | 0 | Coxarthrosis | 50 | 32 | 28 | 50 | 32 | 28 | 0 | 0 | ||
| 5 | 80 | L | Elite | 52 | 52 | 0 | Coxarthrosis | 50 | 25 | 35 | 48 | 24 | 32 | Zones 1, 2 | 0 | ||
| 6 | 67 | R | Meridian | 49 | 50 | Yes | Coxarthrosis | Lost to follow-up | |||||||||
| 7 | 75 | R | Elite | 49 | 50 | 0 | Coxarthrosis | 40 | 25 | 26 | 39 | 26 | 30 | 0 | 0 | ||
| 8 | 31 | R | Meridian | 48 | 48 | Yes | Avascular necrosis | 54 | 15 | 25 | 54 | 25 | 25 | 0 | 0 | ||
| 9 | 31 | L | Meridian | 48 | 48 | Yes | Avascular necrosis | 54 | 32 | 32 | 54 | 32 | 32 | 0 | 0 | ||
| 10 | 53 | R | Meridian | 54 | 54 | 0 | Avascular necrosis | 45 | 26 | 35 | 44 | 27 | 37 | 0 | 0 | ||
| 11 | 66 | L | Meridian | 49 | 50 | 0 | Coxarthrosis | 52 | 32 | 28 | Zone 2 | 50 | 27 | 31 | 0 | 0 | |
| 12 | 70 | R | Meridian | 49 | 50 | 0 | Avascular necrosis | 25 | Deceased | ||||||||
| 13 | 64 | L | Meridian | 56 | 56 | 0 | Coxarthrosis | 41 | 37 | Zone 2 | 42 | 30 | 38 | Hiatus persists | 0 | ||
| 14 | 47 | R | Meridian | 50 | 50 | 0 | Post-traumatic coxarthrosis | 41 | 25 | 38 | 44 | 25 | 35 | 0 | 0 | ||
| 15 | 55 | L | Meridian | 49 | 49 | Yes | Avascular necrosis | 55 | 25 | 30 | Zone 2 | 56 | 25 | 30 | Zone 1 | 0 | |
| 16 | 74 | L | Meridian | 52 | 52 | 0 | Coxarthrosis | 46 | 32 | 34 | 48 | 24 | 36 | 0 | 0 | ||
| 17 | 66 | L | Meridian | 52 | 52 | 0 | Coxarthrosis | 38 | 31 | 36 | 37 | 8 | 35 | 0 | 0 | ||
| 18 | 67 | R | Meridian | 50 | 50 | 0 | Subcapital fracture | 48 | 28 | 26 | 47 | 28 | 28 | 0 | 0 | Fracture | |
| 19 | 68 | L | Meridian | 58 | 58 | 0 | Avascular necrosis | 45 | 28 | 45 | 28 | 32 | 0 | 0 | |||
| 20 | 61 | R | Meridian | 52 | 52 | 0 | Subcapital fracture | 42 | 26 | 30 | 40 | 16 | 33 | 0 | 0 | ||
| 21 | 68 | L | Elite | 51 | 51 | Yes | Coxarthrosis | 46 | 25 | 29 | 45 | 18 | 25 | Zone 1 | 0 | ||
| 22 | 73 | L | Elite | 56 | 56 | 0 | Ankylosing spondylitis | 50 | 25 | 40 | 55 | 42 | Zone 1 | 0 | |||
| 23 | 32 | L | Meridian | 50 | 50 | 0 | Bilateral dysplasia | 50 | 22 | 30 | 48 | 37 | 0 | 0 | |||
The series included 23 patients (10 males and 13 females): 12 left hips and 11 right hips. The mean age at the time of surgery was 63 years (range: 50–70 years) for men and 57 (range: 31–80) for women. Four patients were under the age of 40; 19 were between 50 and 70 years of age, and 4 patients were over the age of 70. The diagnoses included 9 primary arthrosis, 7 avascular necrosis, 2 pseudoarthrosis following subcapital fractures synthesized with cannulated screws, 1 post-traumatic arthrosis, 1 ankylosing spondylitis, and 1 hip dysplasia.
All the surgical interventions were performed with the patients lying on their side using a direct lateral approach (after Hardinge)14. The acetabulum was prepared with ball reamers. The component implanted was 1mm larger than the last reamer in 6 cases and 2mm larger in 2 cases. In the remaining 15 cases, the reamer and the implant were the same size, since the latter had a peripheral diameter that was oversized. This design did not allow for supplementary fixation with screws, as it was a monoblock implant. In 8 cases, milled autograft (taken from the last reamings) was added in the bottom of the acetabular cup.
On the femoral side, the decision as to the choice of implant depended on the patient's age, the femoral bone stock, and on the morphology of the proximal femur. In 17 cases, an uncemented Meridian stem (Howmedica, Rutherford, NJ, USA) was used. In the remaining 6 cases a cemented, Charnley Elite stem (Depuy, Warsaw, IN, USA) was used. In all cases, a 28-mm chromium–cobalt head was implanted.
All the patients received prophylactic intravenous antibiotic treatment, consisting of 1g of cephazolin every 8hours for 48hours and anti-thrombotic prophylaxis with 40mg of subcutaneous enoxaparin daily for 4 weeks. Drains were removed after 48hours. Rehabilitation of walking was started at 48hours using two canes and partial loading. Full loading was begun at six weeks.
All patients were prospectively assessed with post-operative clinical–radiological evaluations performed at 3, 6, and 12 months and then yearly after that. The clinical evaluation included the assessment of pain, function, and degree of joint mobility as per the Merle D’Aubigné-Postel rating scale that varies from 1 (continuous, disabling pain in any position, patients cannot walk and total mobility is less than 30°) up to 6 (patients are pain-free, walk normally, and their degree of joint mobility is greater than 211°). Degrees 5 and 6 are considered to be a good clinical outcome and degrees 4 and less are considered to represent a poor outcome.15
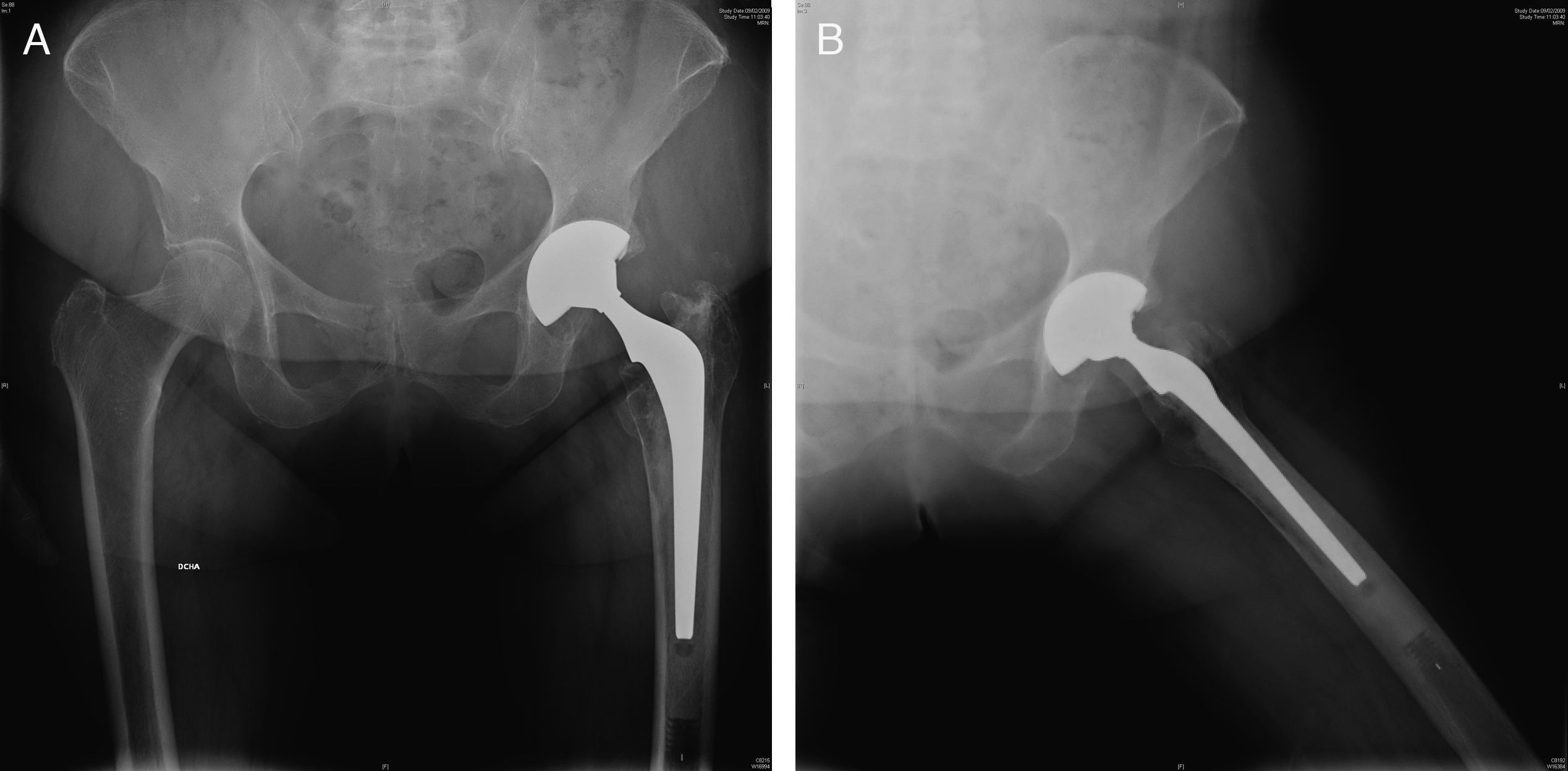
The radiological assessment included an anteroposterior X-ray of the pelvis and a lateral Lauenstein projection. All the X-rays were analyzed by an independent observer (RFF), who had not been involved in any of the surgeries and was unaware of the patients’ clinical outcomes. The abduction angle of the acetabular cups was measured taking the line between the bases of both Köhler's tear drops as a reference. The vertical distance from the centre of hip rotation to this line was also measured in order to assess possible vertical migrations of the acetabular cups and the horizontal distance between the centre of hip rotation and Köhler's line to evaluate medial migration.
Post-operative hiatus, radiolucent lines, and osteolysis were identified in the three zones described by DeLee and Charnley.16 The regions in which the surface of the implant was not in contact with native bone on the immediate post-operative X-ray were classified as post-operative hiatus.17 The regions where lines appeared were defined as radiolucencies if there had not been any post-operative hiatus. These lines were checked on a yearly basis to evaluate progression, if any.
An acetabular component was considered to be radiographically loosened when a linear migration of 3mm or more, a change in the abduction angle of more than 5°, or a complete radiolucent line 2mm thick or thicker was observed.18 Polyethylene wear was measured as per the method described by Kim et al., considering the zero position as the measurement performed based on the 3-month post-operative X-ray.19 The known diameter of the femoral head (28mm) was used to standardize measurements. Statistical analyses were carried out using the SPSS 11.0 statistical software package for Windows, and the level of statistical significance was considered as a value of p<0.05.
ResultsThe mean follow-up of the series was 12 years (range: 2–13). One patient died a year and a half after the intervention due to reasons unrelated to the surgery itself. Another patient was lost to follow-up three years after surgery. Both implants had been clinically and radiographically correct at the time of the last check-up. These implants were excluded from the study. This acetabular cup had a 100% 12-year survival rate for loosening.
The 23 hips in this series had a mean pre-operative pain score of 3 on the Merle D’Aubigné-Postel rating scale; this value improved to 5.4 at the end of the first year and was maintained until completion of follow-up. Pre-operative walking capacity was 2.7 and improved to 5.3 one year following the procedure and was 5.2 at the end of the follow-up period. The degree of articular mobility prior to surgery was 3.0 (61–100°) and improved to values of between 4.0 and 5.0 (101–160° and 161–210°) post-operatively, with a mean of 4.4 at last revision. All the patients displayed a good clinical outcome. None of the patients reported pain in the gluteal region or in the groin when asked specifically about this at the end of follow-up.
The mean value of the abduction angle of the acetabular components was 47.29° (range: 38–60°). The mean height at the centre of rotation of the hip was 23.62mm (range: 10–32). The mean horizontal distance was 31.52mm (range: 25–40).
On the initial post-operative X-ray, post-operative hiatus was identified in three cases (two with a difference between the reamer size and the implant diameter of 2mm and a third one with 3mm of difference). In two cases, these gaps were filled in and in the hiatus only persisted in zone 2 at 12 years of follow-up. Non-progressive, radiolucent lines of less than 2mm in DeLee and Charnley's zone 1 appeared in 4 cases (Fig. 1). None of the acetabular components exhibited osteolysis. All components are currently considered to be osseointegrated. The mean linear wear took place at a rate of 0.158mm/year. At present, the mean wear is 1.9mm (range: 0.6–3.1). No statistically significant associations have been found between the age of the patient or the abduction angle of the acetabular component and the rate of wear of the polyethylene (p=0.99 and p=0.68, respectively).
Insofar as complications are concerned, we had one incomplete, intra-operative femoral fracture when inserting the uncemented stem; the fracture was treated intra-operatively by means of two cerclages. This did not affect the subsequent integration of the stem. We have had one episode of posterior traumatic luxation of the hip 4 years post-operatively; it was successfully treated with conservative therapeutic measures. Another patient presented deep vein thrombosis during the immediate post-operative period.
DiscussionTantalum acetabular cups exhibit excellent survival rates with 10 years of follow-up.20 Studies of classical, uncemented components reveal osseointegration rates of around 30%.21 Tantalum has a porosity of close to 80%, which fosters greater integration. Integration is good even in cases in which the bone on which it is implanted is compromised, such as in high dysplasia. Macheras has reported an osseointegration rate of 100% in 27 hips with high dysplasia.22 Load transfer in acetabular cups made of tantalum is more similar to that of cemented polyethylene acetabular cups. The load is transferred physiologically to the superomedial area of the acetabulum, since tantalum's modulus of elasticity is close to that of the host bone. This is reflected in good clinical outcomes, as demonstrated by the fact that not a single patient reported pain in the groin.
Monoblock acetabular cups raise certain additional technical issues. They do not allow for additional fixation with screws when the initial fixation is not satisfactory. Visualization of the acetabular cup in the patient through the metal implant is hindered by the fact that the polyethylene is already there. In addition, this design has a high friction coefficient and adheres to soft tissues if we have not been careful in retracting them. Furthermore, if we fail to centre the implant properly in the acetabular ring, when impacting it, the acetabular cup may shift cranially when it hits the edge of the acetabulum.12 In this series, the orientation of the components has proved satisfactory. Studies with digital radiographic assessment systems, such as EBRA (Ein-Bild-Rontgen-Analyse method) prove how tantalum acetabular cups do not display significant migration.10,20,23 We have also not detected significant migrations.
On the other hand, the elliptical design and the larger peripheral diameter mean that when it adheres strongly to the peripheral bone, it keeps it from sitting in the fundus of the acetabular cup; this conditions the presence of polar hiatus on the post-operative X-rays. Tantalum's osteoconductive capacity causes these hiatuses between implant and bone to be filled by bone growth in the fundus of the acetabular cup, with hiatus of up to 5mm being filled in within 24 weeks. There is an incidence of up to 29% in some series; as the authors gained experience with the implant, these post-operative gaps became less common.20 The size of the hiatus is generally related to the difference between the reamer and the size of the implant. McKenzie24 found hiatus of less than 1mm when the reamer matched the implant size, and 1.4 or 3.9 when the difference with respect to the reamer was 2 or 4mm, respectively. Gruen25 finds more hiatus with the tantalum designs than in titanium designs, but the latter fill in completely. In a series of 574 tantalum acetabular cups, this author found hiatus in 80 hips (19%), although 84% of them had filled in. In our series, we detected post-operative hiatus in three implants, two of which had filled in. Grafting in the fundus of the acetabulum in 8 cases and the fact that the implants had not been very oversized appears to have had an influence on this rate being lower than in the series of these other authors who did not graft.10
The incidence of radiolucent lines with tantalum implants is very low. Some series do not present a single one.10,20 In Gruen's series, the incidence rate is 9%, 30 out of 334 hips, all of them less than 1mm, non-progressive, and located in a single zone.25 We found radiolucent lines in four implants, none of which were progressive. The incidence of radiolucent lines in tantalum implants is lower than that of titanium implants. In the latter, there is a higher incidence of acetabular cups with stable fibrous fixation.25 Our series shows how integration of the tantalum acetabular cups is good and is maintained long term.
The monoblock design avoids wear between the polyethylene insert and the cup; this reduces the number of wear particles generated. Moreover, because peripheral integration is good and there are no screwholes, the particles do not have access to the bone-implant interface and no osteolytic cavities were seen. In the different series reviewed using this design, we have not found any reference to peri-implant osteolysis.10,20,25 In our series, none of the implants presented areas of osteolysis.
Although in series such as that reported by Macheras,20 with 8–10 years of follow-up, the authors report that they have not found any wear in the polyethylene, that has not been the case with our series. The rate of wear in our series has been 0.158mm/year, which is very much in keeping with that of other contemporary designs, as well as with the classical, non-high density, cross-linked polyethylene.26 We do not know whether the wear in the polyethylene may compromise the survival of these implants over the long run.
The limitation of this series is that it includes few patients, although given the prospective nature of the series, this has enhanced the quality of the follow-up. On the other hand, the patient group presents a heterogeneous make-up in terms of ages and diagnoses, making it a non-uniform series, lacking a control group. In addition, the acetabular cups were used with two different stem designs, which may have a bearing on the evolution of the acetabular cups.
We can conclude that the use of acetabular components made of trabecular metal in primary joint replacement surgery provides outstanding clinical and radiographic results. Longer follow-up times are needed to assess whether the wear of the polyethylene in monoblock implants may condition the survival of acetabular cups despite good integration. Another area of concern has to do with the possibility of having to revise integrated acetabular cups due to the wear of the polyethylene without the possibility of only replacing the insert.
Level of evidenceLevel of evidence II.
Protection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflict of interests to declare.
Please cite this article as: Fernández-Fernández R, et al. Componente acetabular monobloque de tantalio. Seguimiento a largo plazo. Rev esp cir ortop traumatol. 2011;55(5):352–357.