Lateral wall fracture has been recognized as an important sign of instability of pertrochanteric fractures. The aim of the present study is to assess the relationship between lateral wall fractures, helical blade telescoping and neck shortening in fractures treated with intramedullary nailing.
Material and methodA descriptive radiological study was performed at our institution. Patients who suffered a pertrochanteric fracture, treated at Hospital 12 de Octubre by intramedullary nailing were included. All fractures were classified according to Evans and AO systems. Preoperative and postoperative radiological assessment was carried out including a lateral wall fracture classification, helical blade telescoping and femoral neck shortening.
Results210 patients were included, 48% had a fracture of the femoral lateral wall. Helical blade telescoping was higher in lower lateral wall fractures with respect to higher fractures. Difference was statistically significant. Neck shortening was higher in fractures with femoral lateral wall disruption; despite not have found any significant differences comparing to fractures with intact lateral wall (p = 0.39). Multivariate analysis showed statistically significant association between helical blade telescoping, neck shortening and lateral wall fracture.
ConclusionsThere is evidence of a higher helical blade telescoping and neck shortening in pertrochanteric fractures with lateral wall fracture treated with intramedullary nails, especially in those with most unstable patterns such us fractures of the lateral wall distal to the vastus ridge.
Describir y cuantificar el efecto que la fractura de pared lateral produce sobre el colapso del foco fractuario y el deslizamiento de la lámina cefálica, en fracturas pertrocantéreas tratadas con clavos intramedulares.
Material y métodoEstudio descriptivo con revisión retrospectiva de imágenes radiológicas de 210 pacientes con fracturas pertrocantéreas tratados mediante enclavado intramedular. Se realizó la valoración radiográfica preoperatoria y postoperatoria de los pacientes, incluyendo la clasificación de las fracturas según los sistemas AO y de Evans. Las fracturas de pared lateral se subdividieron en tres grupos según la altura del trazo de fractura. La valoración radiográfica postoperatoria incluyó el colapso del foco de fractura y el telescopaje de la lámina cefálica.
ResultadosUn 48% del total presentaban fractura de la pared lateral. El telescopaje de la lámina cefálica fue mayor en fracturas de pared lateral por debajo del tubérculo innominado frente a fracturas por encima del tubérculo (p < 0.05). El colapso del foco de fractura también fue mayor en fracturas con trazo bajo; sin embargo, no se llegó a alcanzar la significación estadística (p = 0.39) frente al resto. El análisis multivariante detectó una asociación significativa entre fracturas de la pared lateral, colapso del trazo de fractura y telescopaje de la lámina cefálica.
ConclusionesLa fractura de pared lateral, especialmente los trazos distales, se asocia a un mayor colapso del foco de fractura y mayor telescopaje de la lámina cefálica. Se precisan estudios posteriores para determinar la significación clínica de estos hallazgos.
The result of the synthesis of a pertrochanteric hip fracture depends on several factors, some of which such as age, the presence of comorbidities, degree of independence, bone mineral quality or the initial type of fracture cannot be modified. Other factors can be modified, as they depend almost entirely on the surgeon. These factors include the capacity to recognise the most unstable fracture patterns, the choice of implant in each case, and the ability to appropriately carry out the surgical technique of reducing the fracture and fixing it internally.1–3
Pertrochanteric fractures may be classified as stable or unstable. The classical criteria for instability include the presence of a long posteromedial section, comminution in the calcar region, subtrochanteric extension and inverse angulation patterns.1–3 The primary aim of treatment in any case is to achieve stable fixation, so the patient is able to immediately apply loading, thereby achieving rehabilitation as early as possible.4–8
Over the past 2 decades lateral wall fracture has come to be seen as an increasingly important criterion for pertrochanteric fracture instability. The integrity of the lateral wall functions as a flying buttress for the proximal femoral fragment; however, its insufficiency gives rise to a characteristic fracture pattern with proximal fragment varus collapse and medialisation of the femoral diaphysis. This is now sufficiently important for the AO to have recently revised and modified its own pertrochanteric fractures classification.9 The new system takes into account the degree of greater trochanter comminution based on 2 parameters, the thickness and height of the remaining lateral wall of the trochanter. 31A1 fractures are considered to be stable with an intact lateral wall, while 31A2 fractures are considered to be unstable with an incompetent lateral wall. The presence of fracture fragments under the innominate tubercle leads to direct classification of the fracture as 31A3.9
The use of screw-sliding plate type devices (DHS) in the treatment of fractures with lateral wall lesion has been associated with a high number of complications. Shortening of the femoral necks and the varus collapse of the proximal fragment often leads to mechanical failure of the implant. Consolidation in a poor position has also been described as a potential complication, as this involves a biomechanical hip alteration with the final result of an alteration in patient gait and autonomy.10–13 Due to these reasons the recommendation now is for the synthesis of these unstable fracture patterns using intramedullary nails. Devices of this type ensure a better biomechanical environment than those provided by extramedullary devices, reducing the risk of complications such as those described above.1,3–5
Intramedullary nails usually have a sliding mechanism for the screw or head plate that permits collapse of the fracture focus. However, the inherent instability of fractures of this type means that they tend to collapse as has been described. Complications have been described such as the loss of femoral offset as well as offset of the abductor lever in this type of fracture, even when they have been appropriately treated by interlocking.11 Excessive sliding of the plate may cause irritation in the soft tissues of the side of the thigh or discomfort due to osteosynthesis material.
The aim of this study is to describe the radiological behaviour of fractures of this type when they are appropriately treated using intramedullary nails. To this end we quantify the degree of fracture focus collapse, estimating this by the degree of femoral necks shortening and plate telescoping.
Material and methodThis is a descriptive study with a retrospective review of radiological imaging tests. Selected cases were extracted from a previous database of 210 patients operated in our hospital from 2013 to 2015 for pertrochanteric hip fractures; this database was prepared and used for previous publications by our institution.2 The inclusion criteria were: patients of either sex and any age with pertrochanteric fractures, diagnosed and then treated using intramedullary nails and followed up in our hospital. The exclusion criteria were: patients with another type of fracture or pertrochanteric fractures treated using another type of implant, patients with multiple trauma or pathological fractures and patients who were treated but not followed-up in our hospital.
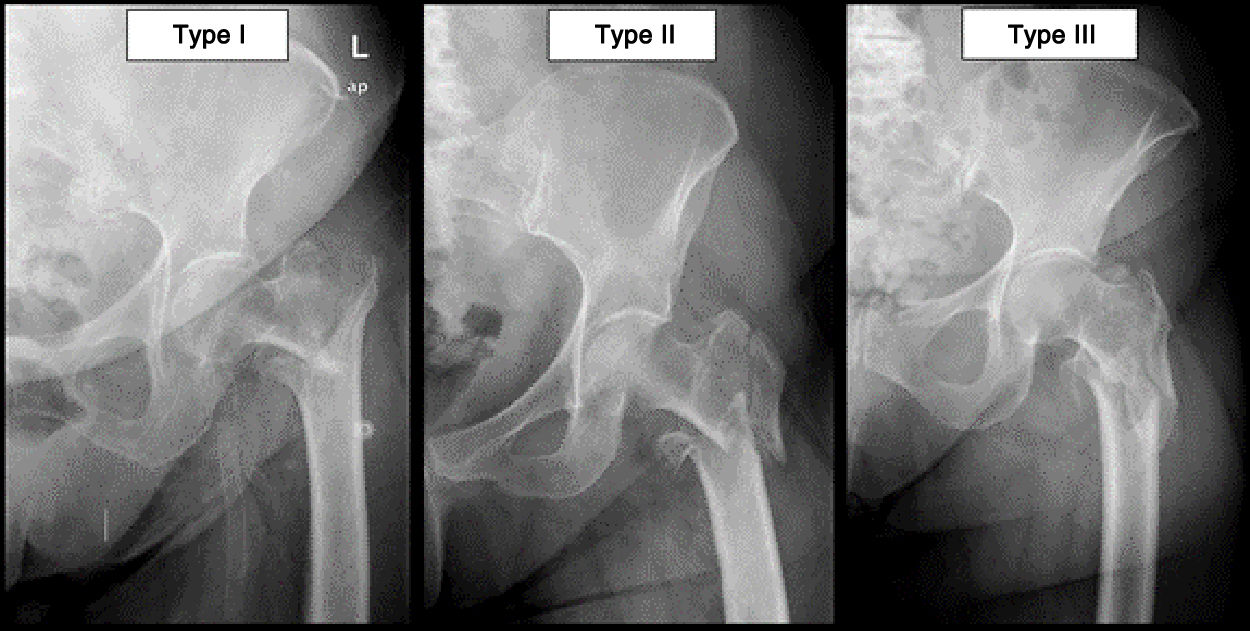
The main researchers (VJD, IAM and JMPG) reviewed the simple preoperative and postoperative X-ray images that were available for each patient. Although it would have been preferable to obtain a preoperative computed tomography image to better evaluate the lateral wall, given the infrastructure of our hospital this was not possible. In the preoperative evaluation fractures were classified according to Evans’ classification and the AO system. Once they had been classified, they were divided into 2 groups: patients with AO-31A2 and AO-31A3 fractures, as well as Evans IVV were included in the group of lateral wall fractures. The patients with AO-31A1 and Evans I-III fractures were included in the group of patients with a complete lateral wall. To better define the type of lateral wall lesion, this group was subdivided into 3 subgroups according to the descriptions used in previous publications.5,9–11 (Fig. 1). We consider type I lateral wall fractures to be all those with a fracture path that breaks above the innominate tubercle.9 We consider type II lateral wall fractures to be all those with a fracture path between the innominate tubercle and a line drawn at the height of the lesser trochanter.5 Lastly, we consider type III lateral wall fractures to be all those with a path that breaks below the lesser trochanter.5 In this study type I fractures were denominated upper fractures, while types II and III were denominated lower fractures.
All of the patients included in the study were operated by the Traumatology Unit of our hospital, using the same type of intramedullary nail implant (PFN-A, Synthes. Switzerland). Nails at an angle of 130° were used in all of the patients, except for 7 patients who required an angle of 125°.
We included the following parameters in the postoperative radiological evaluation: Tip to Apex distance (TAD), plate telescoping and collapse of the fracture focus, measuring the degree of shortening of the femoral neck. These parameters were calculated by measurements in the first and final postoperative examination radiographies undertaken in out-patient surgeries and detecting the differences in the values obtained. The first postoperative examination in the surgery usually takes place 2 weeks after surgery, while the final one occurs at a variable time, depending on the characteristics of the patient, and it may vary from 6 to 12 months.
The computer program used in this study was the iSite radiological system (Phillips, Eindhoven, the Netherlands).
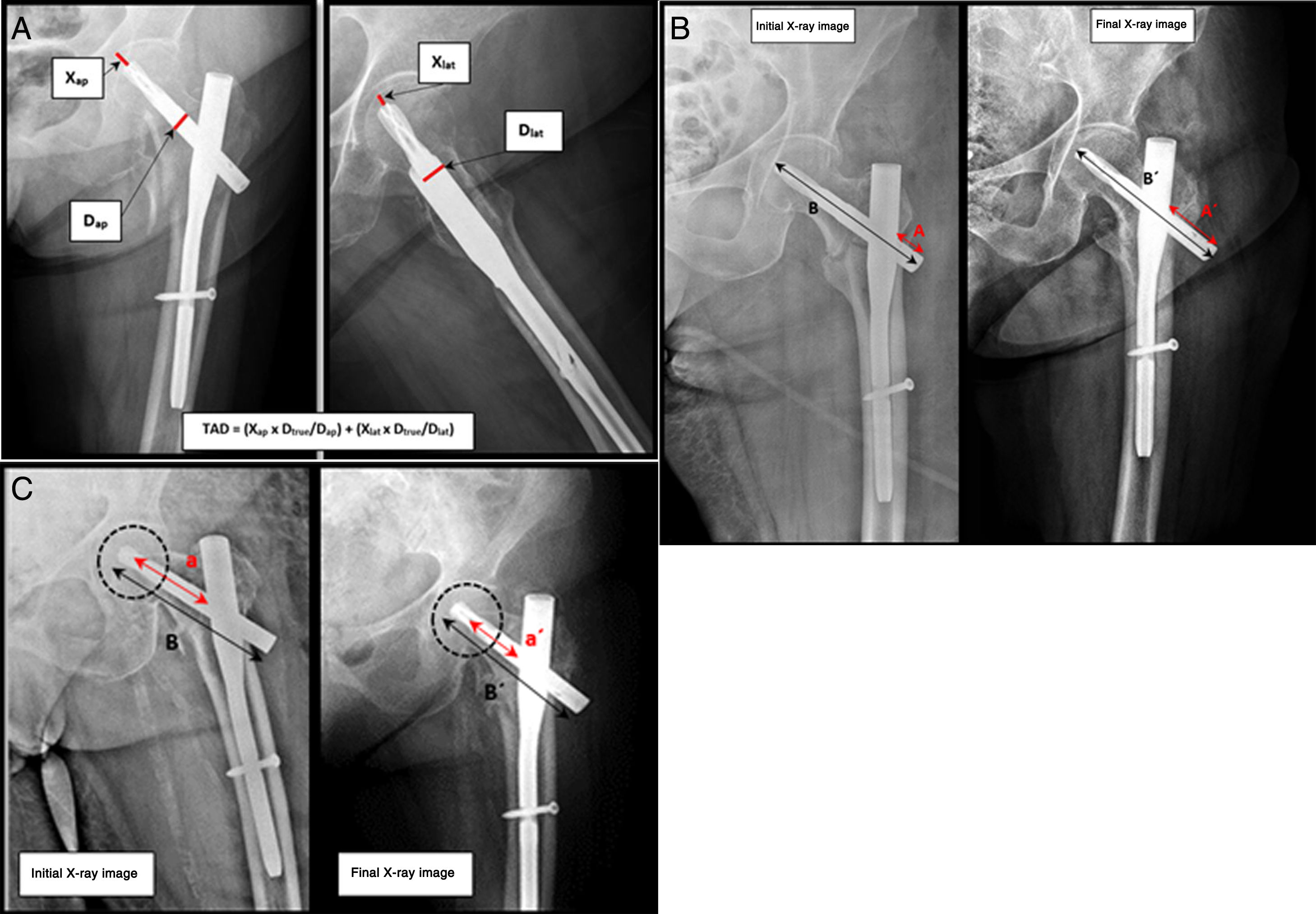
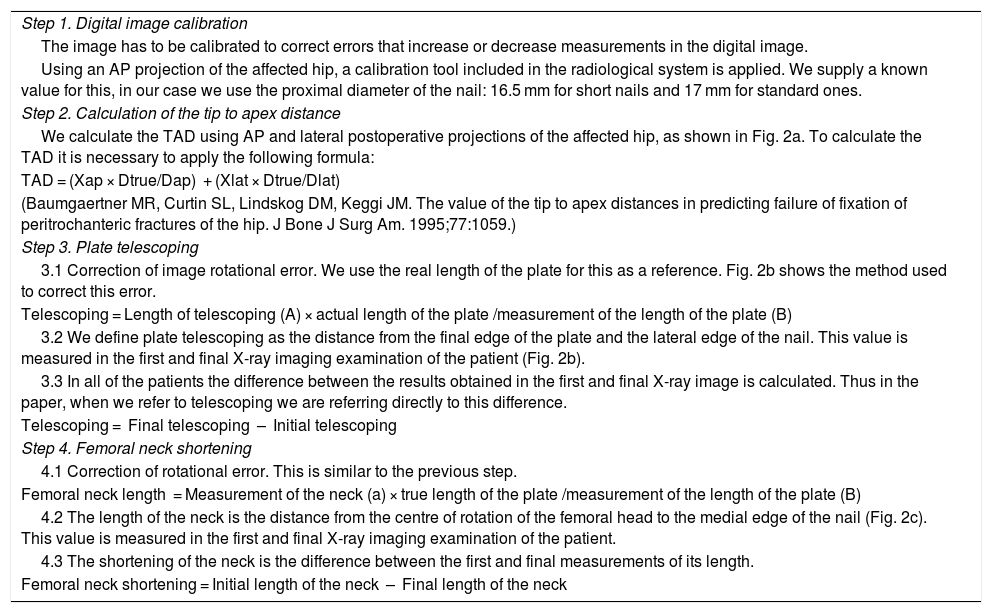
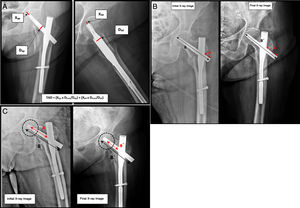
Table 1 contains a step-by-step description of how the different radiological parameters were evaluated. Figs. 2 a–c are also appended, with examples of the mathematical calculations used during the process.
Step-by-step description of the radiographic measurement method.
| Step 1. Digital image calibration |
| The image has to be calibrated to correct errors that increase or decrease measurements in the digital image. |
| Using an AP projection of the affected hip, a calibration tool included in the radiological system is applied. We supply a known value for this, in our case we use the proximal diameter of the nail: 16.5 mm for short nails and 17 mm for standard ones. |
| Step 2. Calculation of the tip to apex distance |
| We calculate the TAD using AP and lateral postoperative projections of the affected hip, as shown in Fig. 2a. To calculate the TAD it is necessary to apply the following formula: |
| TAD = (Xap × Dtrue/Dap) + (Xlat × Dtrue/Dlat) |
| (Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip to apex distances in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone J Surg Am. 1995;77:1059.) |
| Step 3. Plate telescoping |
| 3.1 Correction of image rotational error. We use the real length of the plate for this as a reference. Fig. 2b shows the method used to correct this error. |
| Telescoping = Length of telescoping (A) × actual length of the plate /measurement of the length of the plate (B) |
| 3.2 We define plate telescoping as the distance from the final edge of the plate and the lateral edge of the nail. This value is measured in the first and final X-ray imaging examination of the patient (Fig. 2b). |
| 3.3 In all of the patients the difference between the results obtained in the first and final X-ray image is calculated. Thus in the paper, when we refer to telescoping we are referring directly to this difference. |
| Telescoping = Final telescoping – Initial telescoping |
| Step 4. Femoral neck shortening |
| 4.1 Correction of rotational error. This is similar to the previous step. |
| Femoral neck length = Measurement of the neck (a) × true length of the plate /measurement of the length of the plate (B) |
| 4.2 The length of the neck is the distance from the centre of rotation of the femoral head to the medial edge of the nail (Fig. 2c). This value is measured in the first and final X-ray imaging examination of the patient. |
| 4.3 The shortening of the neck is the difference between the first and final measurements of its length. |
| Femoral neck shortening = Initial length of the neck – Final length of the neck |
a. Method to calculate the Tip to Apex Distance (TAD). Anteroposterior and lateral projections of a left hip with an intramedullary nail (PFN-A, Synthes) (source: Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of tip to apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone J Surg Am. 1995;77:1059). b. Method to calculate telescoping of the cephalic plate (source: Paul et al.11). c. Method to calculate the femoral neck shortening (source: Paul et al.11).
All measurements were collected in a database and statistically analysed using version 9.4 of SAS software.
Descriptive analysis was performed of all of the variables, including the average and standard deviation. The limit of statistical significance was set at P < .05.
The difference between the values of the different parameters obtained in the first and final postoperative examinations was evaluated using the Student t-test.
Pearson’s correlation test was used to evaluate the relationship between the TAD and plate telescoping, as well as the relationship between the TAD and femoral neck shortening.
The Wilcoxon and Kruskal-Wallis non-parametric tests were used to study possible associations between the different fracture patterns and plate telescoping, as well as those between fracture patterns and focus collapse.
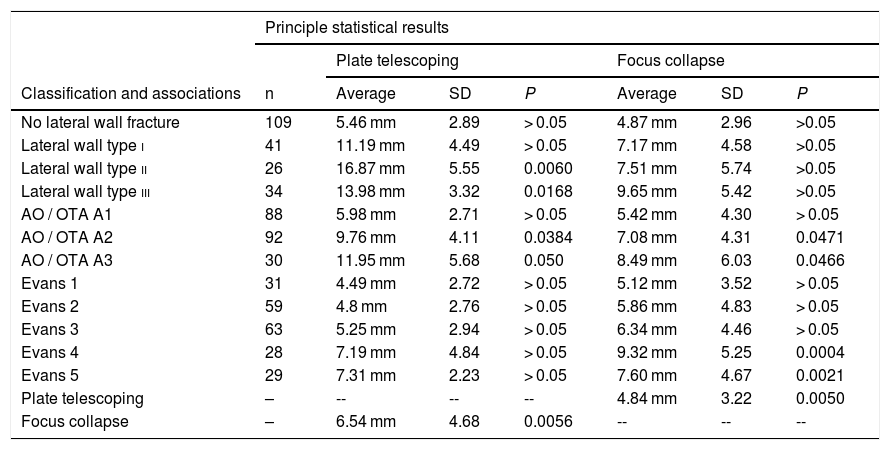
ResultsOf the total number of 210 patients included in our database, 48% had pertrochanteric fractures with lateral wall disruption. In 12% of the patients, the lateral wall fracture was detected in the postoperative study rather than initially. The distribution of the different fracture patterns is shown in Table 2 together with descriptive analysis of the results and chief statistical associations.
Distribution of the patients according to type of fracture and the main statistical associations with fracture focus collapse and plate telescoping.
| Principle statistical results | |||||||
|---|---|---|---|---|---|---|---|
| Plate telescoping | Focus collapse | ||||||
| Classification and associations | n | Average | SD | P | Average | SD | P |
| No lateral wall fracture | 109 | 5.46 mm | 2.89 | > 0.05 | 4.87 mm | 2.96 | >0.05 |
| Lateral wall type i | 41 | 11.19 mm | 4.49 | > 0.05 | 7.17 mm | 4.58 | >0.05 |
| Lateral wall type ii | 26 | 16.87 mm | 5.55 | 0.0060 | 7.51 mm | 5.74 | >0.05 |
| Lateral wall type iii | 34 | 13.98 mm | 3.32 | 0.0168 | 9.65 mm | 5.42 | >0.05 |
| AO / OTA A1 | 88 | 5.98 mm | 2.71 | > 0.05 | 5.42 mm | 4.30 | > 0.05 |
| AO / OTA A2 | 92 | 9.76 mm | 4.11 | 0.0384 | 7.08 mm | 4.31 | 0.0471 |
| AO / OTA A3 | 30 | 11.95 mm | 5.68 | 0.050 | 8.49 mm | 6.03 | 0.0466 |
| Evans 1 | 31 | 4.49 mm | 2.72 | > 0.05 | 5.12 mm | 3.52 | > 0.05 |
| Evans 2 | 59 | 4.8 mm | 2.76 | > 0.05 | 5.86 mm | 4.83 | > 0.05 |
| Evans 3 | 63 | 5.25 mm | 2.94 | > 0.05 | 6.34 mm | 4.46 | > 0.05 |
| Evans 4 | 28 | 7.19 mm | 4.84 | > 0.05 | 9.32 mm | 5.25 | 0.0004 |
| Evans 5 | 29 | 7.31 mm | 2.23 | > 0.05 | 7.60 mm | 4.67 | 0.0021 |
| Plate telescoping | – | -- | -- | -- | 4.84 mm | 3.22 | 0.0050 |
| Focus collapse | – | 6.54 mm | 4.68 | 0.0056 | -- | -- | -- |
In bold type, statistical significance P < .05.
Statistical analysis revealed that patients with lower lateral wall fractures (types ii and iii) had a greater magnitude of plate telescoping than did patients with upper fractures or an intact lateral wall. The difference in magnitude was found to be statistically significant (P < .001). Likewise, patients with upper lateral wall fractures had greater protrusion of the plate than did patients with an intact lateral wall; nevertheless, in this case no statistically significant difference was found (P = .2383).
With respect to fracture focus collapse, statistical analysis found no statistically significant differences in general between patients with an intact lateral wall and those with lateral wall fractures (P = .3925). Nevertheless, patients with lateral wall fracture had greater shortening of the femoral neck, especially those with lower fracture paths.
Multivariate analysis showed that there is a significant association between lateral wall fractures, protrusion of the plate and fracture focus collapse.
Pearson’s correlation test ruled out the existence of an association between the TAD and plate telescoping or femoral neck shortening.
DiscussionThe precise definition of the lateral wall of the femur is still somewhat controversial, and this therefore also applies to what we consider to be a lateral wall fracture. Palm14 defined lateral wall fractures as those which broke below the innominate tubercle. Based on this statement Futaruma et al.5 developed a lateral wall fracture classification system that describes 3 types of fracture: type I or pertrochanteric fractures associated with lateral wall fractures, type II or fractures with a transverse pattern, and type III or fractures with an inverse oblique pattern. However, Babhulkar15 included all pertrochanteric fractures that involved the greater trochanter under the heading of lateral wall fractures, proposing a modification of the AO/OTA classification with the following fracture types: type A or fractures with a lesion of the lateral wall of the greater trochanter, type B or fractures with lesion of the posterior wall of the greater trochanter, and type C or shattered fractures. More recently the AO modified its own classification, including comminution of the greater trochanter as a lateral wall fracture.9 Based on these previous descriptions, in this study we decided to include fractures with comminution of the greater trochanter within the group of lateral wall fractures, classifying them according to the height of the path as upper fractures (type i) or lower fractures (types ii and iii) as was described above.
Lateral wall fracture may occur due to iatrogenic causes. Several studies have warned about the appearance of this fatal complication during lateral wall drilling or the insertion of a cephalic screw using DHS type devices.12,16,17 Kokorogghianis17 describe how initially stable fractures may become highly unstable ones following the iatrogenic fracture of the lateral wall. It is important to be aware of the development of this potential complication and take it into account, as if it appears during the implantation of a DHS type device, it may threaten the final results of fixing the fracture. The incidence of this complication varies from 13% to 33%, 13,16,18,19 and it is usually associated with a risk 7–14 times higher of complications and repeat operations on fractures treated using DHS. In our study 12% of the lateral wall fractures were detected while reviewing postoperative radiographies. This may have occurred due to 2 reasons: due to underestimation of the lateral wall fracture when evaluating the initial simple X-ray images, or because of iatrogenic fractures that occurred during intramedullary nailing. In the latter case lateral wall fracture may occur, as it does with DHS type devices, during drilling or the insertion of the cephalic plate. In our series 86% of the lateral wall fractures detected postoperatively occurred at the same height or distal from the point of insertion of the cephalic plate into the lateral wall; the remaining 14% were catalogued as upper fractures, possibly due to underestimation of the preoperative X-ray images. Respecting nail angle, in 100% of the cases in which this type of complication was detected, nails at 130° degrees had been used; nevertheless, we are unable to establish a clear association between nail angle and iatrogenic fracture in this study given that, with some exceptions, this angle was used in the majority of our series.
Comparative studies between DHS and intramedullary nails have shown less collapse of the fracture focus in unstable patterns treated with nails.20–22 Notwithstanding this, studies have been published which demonstrate that also there is less risk of collapse, loss of femoral offset and offset of the abductor lever arm may also develop when intramedullary devices are used.11 Shortening of the femoral neck and telescoping of the osteosynthesis material, even when it is properly nailed, have been reported and quantified beforehand with varied results. Paul11 carried out a prospective study which compared plate telescoping, femoral neck offset and offset of the abductor lever arm between stable and unstable fracture patterns treated with intramedullary nails. Plate telescoping was 3 times greater in the unstable patterns, with a statistically significant difference (P < .0007). Loss of femoral neck and abductor lever arm offset was also greater in the group of unstable fractures. Gilat21 analysed 48 fractures that had been treated with intramedullary nails. This study found no differences in terms of fracture collapse between stable and unstable patterns. Both studies are heterogeneous regarding fracture stability definition and the methods of radiographic analysis; additionally, neither of them specifically analyses the influence of the lateral wall. We went one step further in this study, analysing the affect specifically produced by lateral wall fractures on the behaviour of the intramedullary device. Statistical analysis revealed, as did the results obtained by Paul,11 which the patients with unstable fracture patterns had greater plate telescoping and greater collapse of the fracture focus in comparison with patients with stable forms. The type of lateral wall fracture has also been shown to be a determining factor in the behaviour of the nail sliding mechanism, as lower lateral wall fractures are associated with greater protrusion a and collapse of the focus than is the case with upper lateral wall fractures or patients with an intact lateral wall. Thus fractures under the innominate tubercle seem to be a risk factor for the plate to slide and protrude in the lateral region following greater collapse of the fracture focus.
Gupta10 described average telescoping of 3.4 mm in the sliding screw after unstable fractures treated with DHS. Jacobs23 reported telescoping of 5.3 mm in stable fractures, vs 15.7 mm in unstable fractures. Larsson24 reported telescoping of 6.3 mm in stable forms vs 12.4 mm in unstable ones. Paul11 described telescoping of 3.3 mm in unstable fractures with intramedullary devices as opposed to 1.2 mm in stables ones, and this difference was statistically significant. Our study shows average telescoping of 5.46 mm in stable fractures and varying degrees of telescoping within a range from 11.95 mm to 16.87 mm in fractures with a lateral wall lesion. This difference too was statistically significant. Collapse of the focus was also greater in the case of fractures with a lateral wall lesion, although in this case statistical significance was not attained.
One of the chief weaknesses of our study is that it is a purely radiological descriptive study, so that we are unable to establish the degree to which our findings are of clinical significance in terms of normal gait alterations or pain in the side of the thigh due to protrusion of the material. There is a lack of agreement in the current literature on this aspect. Paul et al.11 reported that patients with this type of fracture behaviour shown radiographically were significantly associated with poorer biomechanical parameters and alterations in normal gait. Nevertheless, studies such as the one by Reindl et al.25 or Hardy et al.26 did not show any significant functional differences.
Finally, we are aware of the weaknesses of this study, such as its descriptive design and the retrospective review of radiographical studies. As we pointed out above, in this study we quantify the collapse and displacement of osteosynthesis material in fractures that affect the lateral wall, although we are unaware of the clinical significance of these findings. However, the sample size is large enough to make is possible to determine the comparative statistical significance in the degree of sliding of the material between the groups studied. On the other hand, the radiological quantification method described throughout this manuscript is reproducible. It was developed taking into account the potential errors that may appear in the digital format images, and it may be used again in future research works on this subject. Further studies are necessary to establish whether this behaviour of intramedullary nails in fracture patterns with lateral wall lesion is clinically significant.
ConclusionsLateral wall fracture, especially in paths distal to the innominate tubercle, is associated with greater fracture focus collapse and more telescoping of the cephalic plate of the nail. Subsequent studies are necessary to determine the clinical significance of these findings.
Level of evidenceLevel of evidence IV.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Jiménez Díaz V, Auñón Martín I, Pardo García JM, Olaya González C, Caba Doussoux P. ¿Afecta la fractura de la pared lateral al grado de colapso y al grado de deslizamiento de la lámina cefálica, en fracturas pertrocantéreas tratadas mediante enclavado intramedular? Estudio radiológico y revisión de la literatura. Rev Esp Cir Ortop Traumatol. 2021;65:108–115.