The microsurgical techniques with free flaps are the “Gold Standard” in the immediate reconstruction of post-cancer defects of the head and neck. However, procedures are complex, requiring a high degree of specialisation, and not exempt from complications and morbidity. The submental flap is an alternative reconstruction technique in the maxillofacial field in cases where the microsurgical reconstruction is not indicated. The objective of this work is to show the benefits of the use of the submental flap in the maxillofacial reconstruction.
Material and method: The experience of the Department of Oral and Maxillofacial Surgery of the H. U. Ramón y Cajal of Madrid from 2009 to 2013 is described, using the records of a total of 20 reconstructions made with submental pedicled flap in patients with intra- and extra-oral cancers.
ResultsThe results were satisfactory in the 19 patients who underwent surgery, according to the criteria for coverage of the defect, aesthetics and functionality. There were 12 elective functional neck dissections, with histological findings, N0. In no case was transfer of cervical tumor disease to the recipient bed detected. There was only local recurrence of the disease in 1 patient.
ConclusionsThe submental flap constitutes a valid alternative for the reconstruction of orofacial defects, especially in elderly patients or patients that, due to deteriorated general condition require less aggressive treatments and reduced surgical times. Requires rule out the presence of cervical lymph node metastatic disease needs to be ruled out prior to surgery. Its use is controversial for the repair of defects after resection of tumours with high levels of tumour-infiltrating lymphocytes.
Las técnicas microquirúrgicas con colgajos libres constituyen el «Gold Standard» en la reconstrucción inmediata de defectos postoncológicos de cabeza y cuello. Sin embargo, son procedimientos complejos, que requieren un alto grado de especialización, no exentosde complicaciones y morbilidad. El colgajo submental constituye una alternativa recons-tructiva en el territorio maxilofacial, en casos en los que la reconstrucción microquirúrgicano está indicada. El objetivo del trabajo es mostrar los beneficios del empleo del colgajosubmental en la reconstrucción maxilofacial.
Material y métodoPresentamos la experiencia recogida en el Servicio de Cirugía Oral y Maxi-lofacial del H.U. Ramón y Cajal de Madrid desde 2009 hasta 2013, registrando un total de 20 reconstrucciones realizadas con colgajo submental pediculado en pacientes con procesosneoplásicos a nivel intra y extraoral.
ResultadosLos resultados fueron satisfactorios en 19 pacientes intervenidos, atendiendo alos criterios de cobertura del defecto, estética y funcionalidad. Se realizaron 12 diseccionescervicales funcionales electivas, con resultado histológico N0. En ningún caso se detectótransferencia de enfermedad tumoral cervical al lecho receptor. Solo se ha evidenciadorecurrencia local de la enfermedad en un paciente.
ConclusionesEl colgajo submental constituye una alternativa válida para la reconstrucciónde defectos orofaciales, especialmente en aquellos pacientes que por edad o estado generaldeteriorado requieren tratamientos poco agresivos y con tiempos quirúrgicos reducidos. Requiere descartar la presencia de enfermedad metastásica ganglionar cervical previamentea su realización. Su empleo es controvertido para la reparación de defectos tras resecciónde tumores con alta linfofilia.
The reconstruction of orofacial defects after ablative surgery has a considerable impact on the quality of life of these patients. The main objective of the reconstruction is to restore both the morphology and the function of lost tissue. Therefore, the first option is microsurgical techniques with free flaps. However, these are complex procedures requiring a high degree of specialisation, not exempt from perioperative vascular complications and morbidity in the donor site of the cut flap, which present certain limitations in patients of advanced age or with high-risk systemic diseases, particularly when the reconstruction is limited to small to medium-sized tissue defects.
In these cases, the submental flap is an ideal reconstructive alternative in the maxillofacial area for lesions affecting the lower half of the face or the intraoral area.1 This flap was initially described by Martin et al2 in 1993, although it was not until 1996 that Sterne and Hall3 applied it to the reconstruction of an oral defect after resection of an epidermoid carcinoma. It is characterised by a large constant vascular pedicle located in the submental artery branch of the facial artery, which releases from 1 to 4 cutaneous perforators at the level of the anterior digastrics muscle belly. In addition, it provides excellent colour and texture, great versatility and little morbidity in the donor site. Its use for malignant lesions is still controversial due to the risk of transferring the cervical metastatic disease to the recipient site of the flap.4,5
This article describes the surgical technique used to raise the flap, the postoperative complications and the final results obtained.
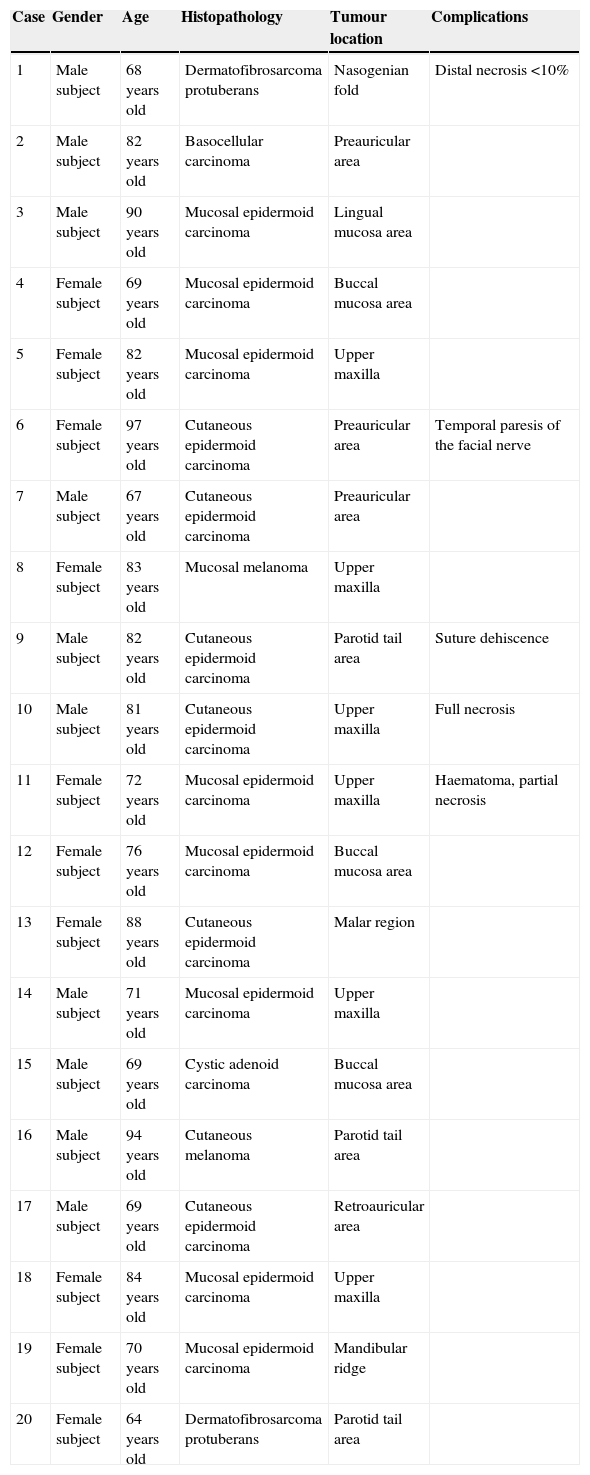
Materials and methodsThis is a retrospective study about the data collected by the Oral and Maxillofacial Surgery Department of the H.U. Ramón y Cajal Hospital of Madrid from 2009 to 2013, amounting to 20 reconstruction procedures of small to medium-sized defects conducted with a pedicled submental flap in patients who had undergone neoplastic processes at an intraoral and extraoral level: 9 cutaneous lesions (3 at a preauricular level, one in the nasogenian fold and one in the malar region, 3 in the parotid tail area and one in the retroauricular area), 4 lesions in the intraoral soft tissue (one in the lingual area and 3 in the buccal mucosa area), one in the mandibular ridge, and 6 at the level of the upper maxilla. Among the lesions described in the histological analysis, we found one mucosal melanoma, 5 cutaneous epidermoid carcinomas, 9 mucosal epidermoid carcinomas, 2 dermatofibrosarcoma protuberans, one cutaneous melanoma, one cystic adenoid carcinoma and one basocellular epithelioma (Table 1).
Lesions described in the histological analysis.
| Case | Gender | Age | Histopathology | Tumour location | Complications |
|---|---|---|---|---|---|
| 1 | Male subject | 68 years old | Dermatofibrosarcoma protuberans | Nasogenian fold | Distal necrosis <10% |
| 2 | Male subject | 82 years old | Basocellular carcinoma | Preauricular area | |
| 3 | Male subject | 90 years old | Mucosal epidermoid carcinoma | Lingual mucosa area | |
| 4 | Female subject | 69 years old | Mucosal epidermoid carcinoma | Buccal mucosa area | |
| 5 | Female subject | 82 years old | Mucosal epidermoid carcinoma | Upper maxilla | |
| 6 | Female subject | 97 years old | Cutaneous epidermoid carcinoma | Preauricular area | Temporal paresis of the facial nerve |
| 7 | Male subject | 67 years old | Cutaneous epidermoid carcinoma | Preauricular area | |
| 8 | Female subject | 83 years old | Mucosal melanoma | Upper maxilla | |
| 9 | Male subject | 82 years old | Cutaneous epidermoid carcinoma | Parotid tail area | Suture dehiscence |
| 10 | Male subject | 81 years old | Cutaneous epidermoid carcinoma | Upper maxilla | Full necrosis |
| 11 | Female subject | 72 years old | Mucosal epidermoid carcinoma | Upper maxilla | Haematoma, partial necrosis |
| 12 | Female subject | 76 years old | Mucosal epidermoid carcinoma | Buccal mucosa area | |
| 13 | Female subject | 88 years old | Cutaneous epidermoid carcinoma | Malar region | |
| 14 | Male subject | 71 years old | Mucosal epidermoid carcinoma | Upper maxilla | |
| 15 | Male subject | 69 years old | Cystic adenoid carcinoma | Buccal mucosa area | |
| 16 | Male subject | 94 years old | Cutaneous melanoma | Parotid tail area | |
| 17 | Male subject | 69 years old | Cutaneous epidermoid carcinoma | Retroauricular area | |
| 18 | Female subject | 84 years old | Mucosal epidermoid carcinoma | Upper maxilla | |
| 19 | Female subject | 70 years old | Mucosal epidermoid carcinoma | Mandibular ridge | |
| 20 | Female subject | 64 years old | Dermatofibrosarcoma protuberans | Parotid tail area |
The patient is laid on the supine decubitus position, with the head extended and slightly inclined towards the opposite side of the lesion. The upper limit of the flap is marked at 1cm below the mandible base, and the lower limit is marked upon verification of direct closure using the “pinch test”. The length of the cutaneous pad may be extended between both mandible angles if necessary, but it is usually designed between the symphysis and the mandible angle. The ipsilateral anterior digastric muscle belly and the submental vessels are usually located at 5.5cm before the mandible angle (Fig. 1).
Flap dissection begins from the side opposite to the pedicle, affecting from the skin and subcutaneous tissue to the platysma muscle. The flap is separated on a subplatysmal level until the digastric muscle and the submaxillary gland are exposed. At this point, the identification of the marginal nerve and the dissection of the submaxillary gland are required. The facial artery is located at the upper end of this gland, while the submental pedicle is located at its origin. Then, the contralateral side is separated and the anterior digastric muscle belly is incorporated into the flap. Some authors (Patel et al.)6 also incorporate the mylohyoid muscle into the ipsilateral side, so as to further protect the pedicle, although this increases the thickness of the flap.
If the length of the pedicle is sufficient to allow the flap a good rotation arc, the remaining branches and tributary arteries of the facial artery are ligated. However, if the length of the pedicle is not sufficient, it may be increased by using a “reverse flow” design3,7 proximally ligating the facial artery to the origin of the submental artery. The length of the venous pedicle may be increased by dissecting a communicating branch between the facial vein and the external jugular vein. By ligating the facial vein, the Y-vascular pattern turns into a V-vascular pattern, increasing the length of the pedicle by up to 5cm.
The flap is then pedicled to the submental artery and vein. A tunnel may be made to the defect site and the flap may be sutured to the defect. A direct closure is performed on the donor site.
Some modifications to the incision design might be required to perform a functional neck dissection, and it is advisable to start from the flap dissection to protect the submental pedicle.
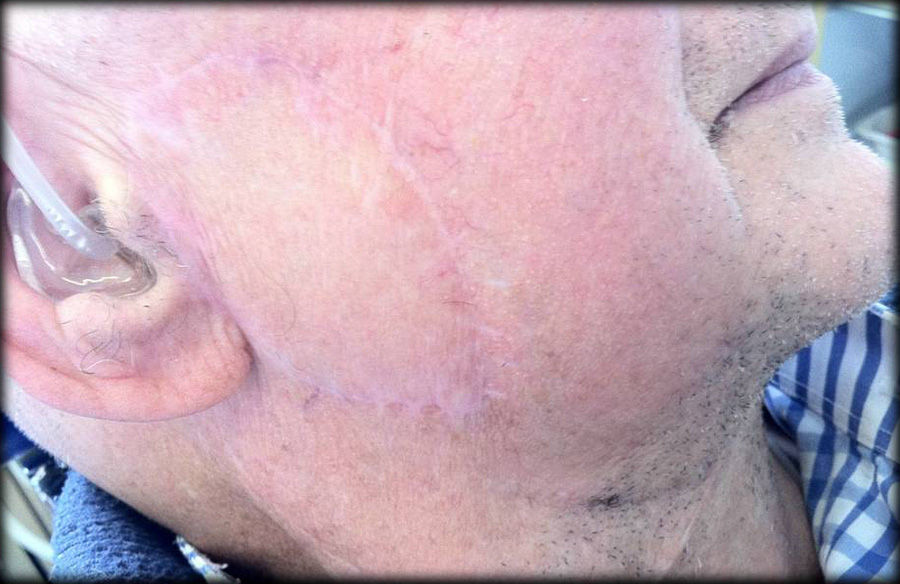
ResultsThis study involved 10 male subjects and 10 female subjects, from 64 to 97 years old. Upon resection of the tumour, the reconstruction of defects with submental flap was satisfactory in 19 out of 20 patients, according to aesthetics and functionality criteria, without any speech or deglutition complications (Figs. 2–5). One of the patients who underwent a defect reconstruction procedure after hemimaxillectomy due to mucosal epidermoid carcinoma presented full flap necrosis due to a haematoma in the surgical bed and subsequent vein thrombosis. Another case of partial necrosis was recorded (30%) in a patient who underwent surgery due to mucosal epidermoid carcinoma in the upper maxilla, also as a result of a haematoma in the surgical bed. Another patient who underwent surgery due to dermatofibrosarcoma protuberans in the nasogenian fold presented distal flap necrosis amounting to 10% of the surface. Lastly, there was a case of temporal paresis of the marginal branch of the facial nerve.
All the donor sites recovered properly. There was suture dehiscence in the recipient site (suture between the submental flap and the cervical incision) of a patient who underwent surgery for the removal of a cutaneous epidermoid carcinoma from the parotid tail area, associated with functional neck dissection, which was subject to local treatment and subsequently healed by secondary intention, with an acceptable aesthetic result.
There were 12 elective functional neck dissections after cutting the flap, all of which had a histological result of N0. In no case was transfer of cervical tumour disease to the recipient site detected. There was only local recurrence of the tumour in one patient.
DiscussionSeveral flaps have been described by different authors for the reconstruction of cutaneous defects in the two lower thirds of the face and intraoral defects. However, little mobility and lack of reliability are common disadvantages to all of these. The submental flap constitutes a reliable and valid alternative to microvascularised flaps, particularly in elderly patients or patients who, due to deteriorated general condition, require less aggressive treatments and reduced surgical times, especially when reconstruction is limited to small to medium-sized cutaneous defects.8–10
In our experience, it has generally been demonstrated that the flap has a long pedicle and ample rotation arc and may cover a large surface. Karacal et al.11 reported the use of flaps between 4cm×6cm and 6cm×8cm for the reverse pattern. A cutaneous pad of up to 7cm×18cm has been suggested, depending on the laxity of the submentonian skin.2 As to quality, this flap is an ideal replacement for the facial area, given its similarity with the texture and colour of the skin. Direct closure of the donor site with minimal scarring is an additional advantage.5,12
The vascular anatomy of the submental flap has been deeply studied. Faltaous and Yetman13 demonstrated that this flap is safe, since it has a reliable blood supply running through its middle axis and a long vascular pedicle. Stern et al.3 divided facial vessels proximally to the origin of the submentonian artery. Thus, the blood supply was based on the retrograde flow from the distal end of the facial vessels. This variant is called “flap with reverse flow” and it allows for an additional increase of the pedicle length, which covers defects located in the upper half of the face.7
There is controversy in the literature regarding the potential risk of this flap to transfer cervical metastatic disease to the recipient site, as well as the impossibility of conducting a rigorous level I neck dissection. However, the dissection plane of the flap is subplatysmal, which is the same as is used for neck dissection. Therefore, if anatomical planes are respected, the chances of tumour dissemination may be reduced.4,5,14 Chow et al.15 revised 10 cases of reconstruction with submental flap after the resection of aggressive oropharyngeal tumours and discovered that disease recurrence was more related to the aggressiveness of the primary tumour than to the oncological “transgression” resulting from this flap. In our series, locoregional tumour disease recurrence and transfer of the tumour disease in the recipient site have not been detected in any case. Therefore, our findings support the oncological safety of this flap, provided that it is used in patients with no cervical lymph node disease at the time of surgery (clinical and radiological results of N0). If surgeons observe suspicious nodes during neck dissection, they should refrain from performing a submental flap and choose another reconstructive option.16
ConclusionsThe submental flap introduced by Martin et al. in 1991 is a valid alternative for the reconstruction of complex orofacial defects in cases where microsurgical reconstruction techniques are contraindicated. Apart from its similarity to resected tissue, as it occurs with other local regional cervical flaps, the submental flap offers additional advantages, such as reduced surgical time and versatility to become a myocutaneous, myofascial, osteomyocutaneous or even free flap. It has been shown to be particularly adequate for defects in the buccal mucosa, upper maxilla and facial skin. Furthermore, the donor site allows for direct closure with good aesthetic results and no complications for neck mobility. It is especially indicated in patients of advanced age or deteriorated general condition requiring less aggressive treatments and reduced surgical times. The presence of cervical lymph node metastatic disease needs to be ruled out prior to surgery and its use is contraindicated in cases with high levels of tumour-infiltrating lymphocytes.
Ethical disclosuresProtection of people and animalsThe authors state that no experiments were performed on human beings or animals as part of this investigation.
Data confidentialityThe authors state that they have followed the protocols of their workplace about the publication of patient data and that all the patients included in the study have received enough information and have given their written informed consent to participate in that study.
Right to privacy and informed consentThe authors state that this article does not contain patient data.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Sagüillo K, García-Serrano G, Almeida F, Núñez J, Picón N, Acero J. El colgajo submental en reconstrucción de defectos orofaciales. Rev Esp Cir Oral Maxilofac. 2015;37:196–201.