Recently, few reports have described a serious condition linked to SARS-CoV-2 that mimics Kawasaki disease called multisystem inflammatory syndrome, especially in children (MIS-C) and young adults. In this work, we report on a severe form of MIS in a young female adult previously infected by SARS-CoV-2. She was treated by plasmapheresis with albumin and steroids, however outcome was fatal. We discuss the pathogenesis of this rare and life threatening entity and suggest some therapeutic regimen. This syndrome should not be misdiagnosed with an infectious or a drug induced cutaneous rash in the current context of COVID-19 pandemic.
Pocos informes han descrito recientemente una situación grave asociada a SARS-CoV-2 que remede la enfermedad de Kawasaki denominada síndrome inflamatorio multisistémico, especialmente en niños (MIS-C) y adultos jóvenes. En este trabajo, reportamos una forma grave de MIS en un adulto joven previamente infectado por SARS-CoV-2. La paciente fue tratada mediante plasmaféresis con albúmina y esteroides, pero sin embargo el resultado fue fatal. Tratamos aquí la patogenia de esta entidad rara y potencialmente mortal, y sugerimos algún régimen terapéutico. No debería confundirse este síndrome con una erupción cutánea infecciosa o causada por un fármaco en el contexto actual de la pandemia por COVID-19.
The 2019 novel coronavirus disease (COVID-19) can cause a wide spectrum of symptoms in humans, ranging from asymptomatic to mild or severe. Therefore, the clinical presentations of this disease may include upper and/or lower respiratory tract involvement with multisystem dysfunction that particularly affects the gastrointestinal, cardiovascular and renal systems. SARS-CoV-2 invades cells located in lung, heart and kidney tissue through the angiotensin converting enzyme 2 (ACE2), triggering a dysregulated immune response with massive release of cytokines leading to a cytokine storm in severely affected patients1. Kawasaki disease (KD), particularly its severe form – Kawasaki disease shock syndrome (KDSS) – is rare in adults. Some recent reports have shown that COVID-19 is associated with the appearance of cases of Kawasaki-like disease (KLD), particularly in children. To our knowledge, the following is one of the first cases describing a severe form of KLD in a young adult that was probably secondary to COVID-19. The patient’s husband gave his informed consent for this case report.
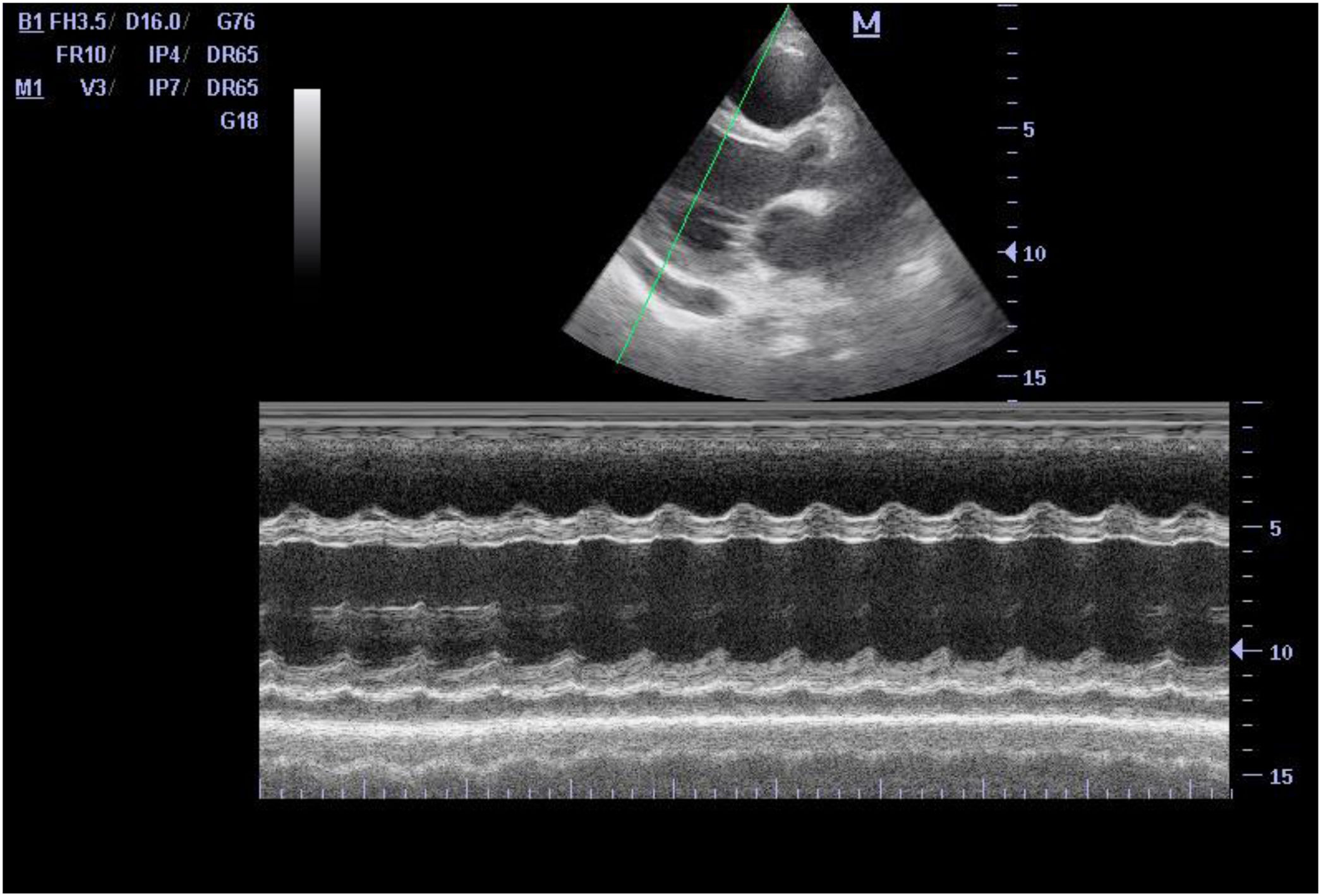
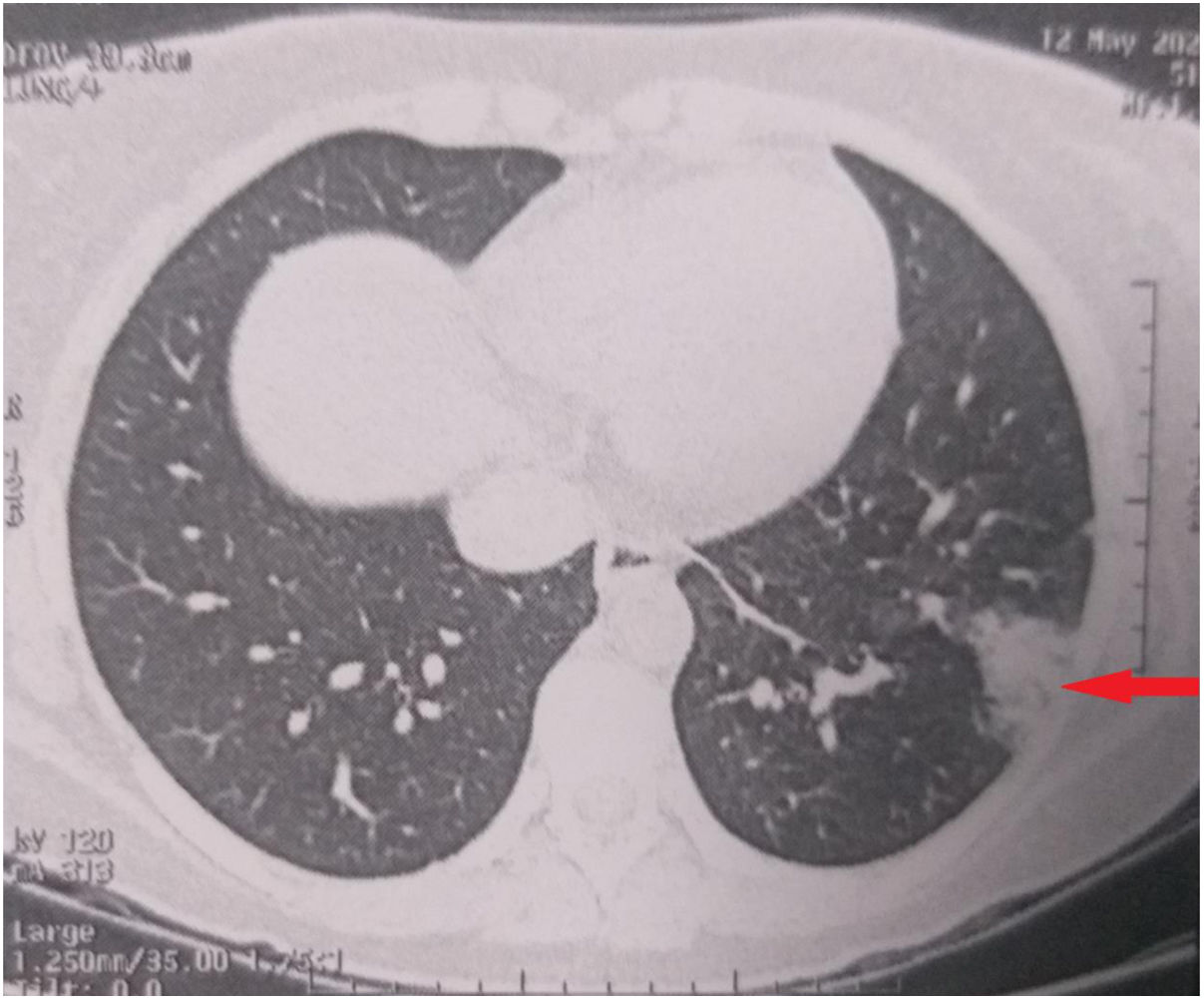
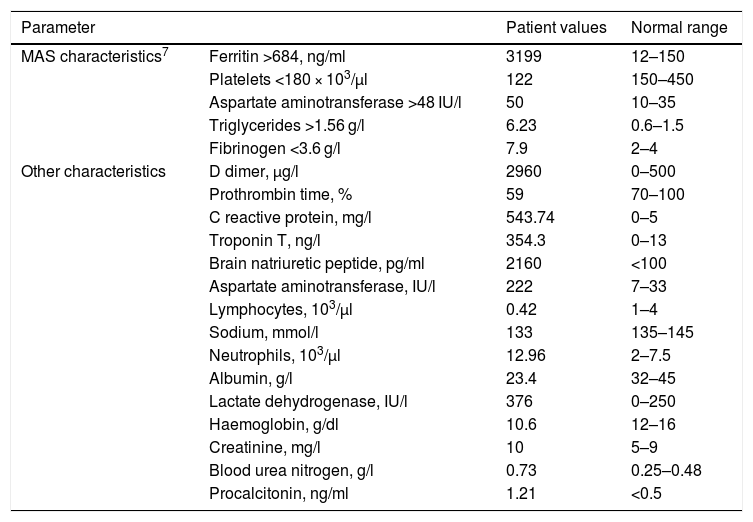
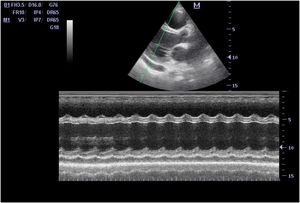
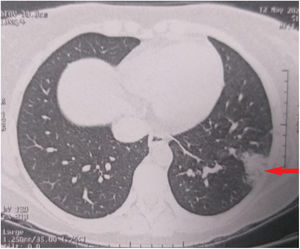
Case reportA previously healthy 28-year-old Caucasian woman (weight 70 kg, body mass index 24.8 kg/m2) presented in the emergency unit with sudden onset skin rash that had started in the post-auricular area 2 days earlier and spread rapidly to other areas of the body. She reported persistent fever, sore throat, dry cough, fatigue, and abdominal pain that had started 7 days prior to admission. She had not taken any drugs before the onset of symptoms. Physical examination revealed fever (39.6 °C), tachycardia (150 beats/min), tachypnoea (26 breaths/min) and low blood pressure (89/45 mmHg). SpO2 was 91% on room air. A generalized and localized rash was observed in the following areas: anterior and posterior trunk, upper and lower extremities, hands and feet. The patient also presented conjunctivitis with no cervical lymphadenopathy (Fig. 1). She was immediately transferred to the intensive care unit (ICU) under oxygen support (10 l/min with a non-rebreather mask) where aggressive treatment with crystalloids (500 ml), continuous infusion of norepinephrine (0.1 μg/kg/min), and empirical antibiotic therapy (IV ceftriaxone 2 g/day, and continuous infusion of vancomycin 2 g/24 h) was started. Point of care echocardiography revealed severe systolic (LVEF approximately 15%) and diastolic dysfunction, with biventricular distention and small pericardial effusion (Fig. 2). On this basis, dobutamine was started (10 μg/kg/min) and the patient was intubated. Laboratory tests performed at admission showed signs of disseminated intravascular coagulation and sepsis (Table 1). However, blood, urine, and cerebrospinal fluid cultures were negative. After stabilizing the patient, a chest computed tomography (CT) scan revealed small alveolar condensation in the left lung (Fig. 3). The multiplex rt-PCR of nasopharyngeal and tracheal aspirate samples did not detect the presence of any viral or bacterial pathogens (adenovirus, human coronavirus [HKU1, NL63, 229E, OC43], MERS* coronavirus, SARS-CoV-1, SARS-CoV-2, human metapneumovirus, human rhinovirus, enterovirus, influenza virus [A, A1H1, AH1-2009, B], parainfluenza virus [1, 2, 3 and 4], respiratory syncytial virus, or Bordetella pertussis, Bordetella parapertussis, Chlamydophila pneumoniae, Mycoplasma pneumoniae). However, the rapid IgG/IgM test for COVID-19 was positive for IgG antibodies, and negative for IgM antibodies.
Laboratory parameters, results, and normal ranges.
| Parameter | Patient values | Normal range | |
|---|---|---|---|
| MAS characteristics7 | Ferritin >684, ng/ml | 3199 | 12–150 |
| Platelets <180 × 103/μl | 122 | 150–450 | |
| Aspartate aminotransferase >48 IU/l | 50 | 10–35 | |
| Triglycerides >1.56 g/l | 6.23 | 0.6–1.5 | |
| Fibrinogen <3.6 g/l | 7.9 | 2–4 | |
| Other characteristics | D dimer, μg/l | 2960 | 0–500 |
| Prothrombin time, % | 59 | 70–100 | |
| C reactive protein, mg/l | 543.74 | 0–5 | |
| Troponin T, ng/l | 354.3 | 0–13 | |
| Brain natriuretic peptide, pg/ml | 2160 | <100 | |
| Aspartate aminotransferase, IU/l | 222 | 7–33 | |
| Lymphocytes, 103/μl | 0.42 | 1–4 | |
| Sodium, mmol/l | 133 | 135–145 | |
| Neutrophils, 103/μl | 12.96 | 2–7.5 | |
| Albumin, g/l | 23.4 | 32–45 | |
| Lactate dehydrogenase, IU/l | 376 | 0–250 | |
| Haemoglobin, g/dl | 10.6 | 12–16 | |
| Creatinine, mg/l | 10 | 5–9 | |
| Blood urea nitrogen, g/l | 0.73 | 0.25–0.48 | |
| Procalcitonin, ng/ml | 1.21 | <0.5 | |
These findings led us to a diagnosis of Kawasaki disease shock syndrome secondary to COVID-19, and the patient was treated with therapeutic doses of low-molecular-weight heparin, methylprednisolone (2 mg/kg/day), a single dose of 500 mg of acetylsalicylic acid, and plasmapheresis with albumin was started. Despite these measures, the patient’s haemodynamic status deteriorated rapidly, and 48 h after admission she presented cardiac arrest refractory to cardiopulmonary resuscitation. Permission to perform an autopsy was sought, but her husband refused the request.
DiscussionKD, a rare idiopathic syndrome, is an acute vasculitis of childhood that leads to coronary artery aneurysms in 25% of untreated cases2. It has been suggested that this entity is likely due to hyperinflammation and runaway immune response derived from various infections3. It could also have a genetic component. According to Italian guidelines, diagnosis of KD is consensual and clinically based on the presence of certain criteria: persistent fever, swollen lymph nodes, rash, and enanthema4. Some patients present a severe form of KD, called KDSS, that causes circulatory collapse, respiratory failure and poor peripheral perfusion.
Hundreds of children and adolescents in western countries (the UK, France, Italy, Spain and the USA) have developed a serious SARS-CoV-2-related condition that mimics KD, called KLD or multisystemic inflammatory syndrome in children (MIS-C), also known a paediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS)5–7. Some case reports have described young adults with COVID-19 and moderate cardiac dysfunction presenting the same syndrome within a week of the onset of symptoms, with favourable outcomes8,9.
In the above case, prolonged fever of more than 38.5 °C, cytokine storm (attested by the inflammatory status), and shock caused by myocarditis and vasoplegia triggered a severe form of KLD with refractory circulatory collapse. In fact, this disorder had clinical symptoms similar to those found in KDSS, together with biochemical evidence of macrophage activation syndrome (MAS)7.
Due to its rarity, this condition can be confused with toxic shock syndrome or a drug-induced skin condition, which can delay or prevent early treatment.
Treatment of MIS-C is based on immunomodulators such as corticosteroids and/or plasmapheresis, since resistance to intravenous immunoglobulin has been reported7. However, intravenous immunoglobulin appears to be effective in adult patients8,9. In our patient, the fatal outcome was probably due to the severity of the myocardial damage, probably due to the direct action of coronavirus on the myocardium, and the indirect effect of inflammation10.
ConclusionThis case shows that COVID-19 pneumonia can lead to Kawasaki-like multisystem inflammatory syndrome in adults. It is essential to consider this disease in patients presenting with a rash in the context of the current COVID-19 pandemic, as diagnosis would lead to prompt treatment with intravenous immunoglobulin, plasmapheresis and steroids, and prevent fatalities.
Author contributionsYoussef Elouardi: Concept, Writing of the original draft, Writing, review and editing, Research, Visualization, Validation.
Houssam Rebahi: Terminology, Writing - review and editing, Validation.
Youssef Zarrouki: Visualization, Research.
Amra Ziadi: Research, Supervision.
Said Younouss: Terminology, Review, Validation.
Mohamed Abdenasser Samkaoui: Terminology, Review and editing, Validation.
FundingThis study did not receive any financial support.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Elouardi Y, Rebahi H, Zarrouki Y, Ziadi A, Younous S, Samkaoui MA. Síndrome inflamatorio multisistémico de tipo Kawasaki asociado a COVID-19 en un adulto. Rev Esp Anestesiol Reanim. 2022;69:43–47.