In recent years, minimally invasive cardiac surgery (MICS) has been developed and applied to a greater number of pathologies, especially in mitral valve surgeries, as it obtains results comparable to those of conventional techniques while entailing lower surgical trauma and shorter recovery time. MICS requiring one-lung ventilation has been associated to the appearance of unilateral pulmonary edema (UPE), which is a potentially serious complication. The objective is determining the incidence of UPE after mitral MICS and its development associated factors.
Material and methodsObservational descriptive and single-center study analyzing data from patients undergoing mitral valve MICS (right mini-thoracotomy) consecutively collected between the years 2015 and 2017.
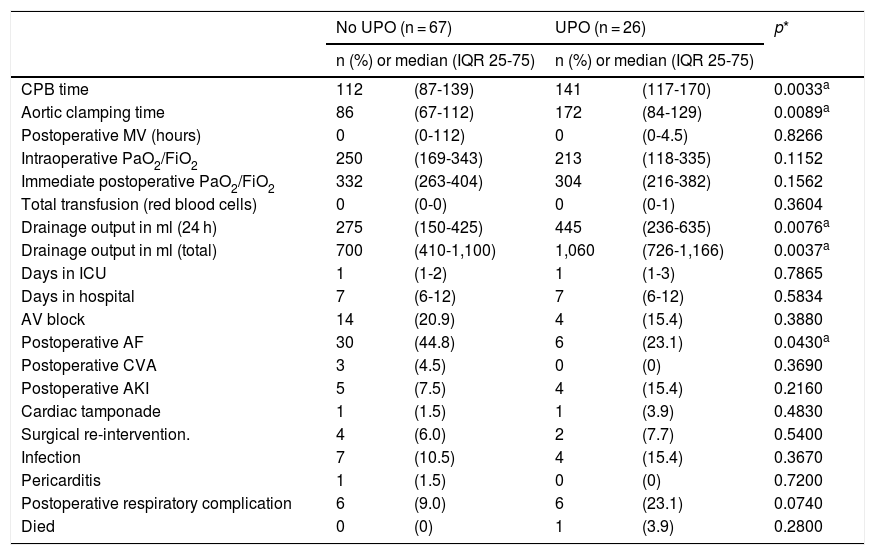
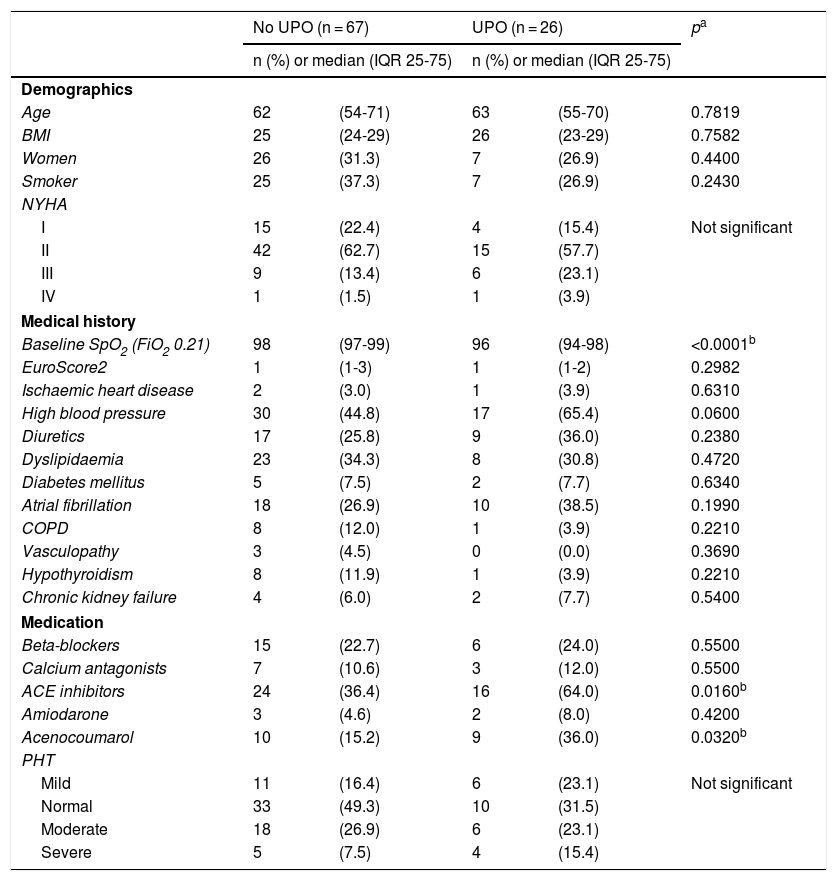
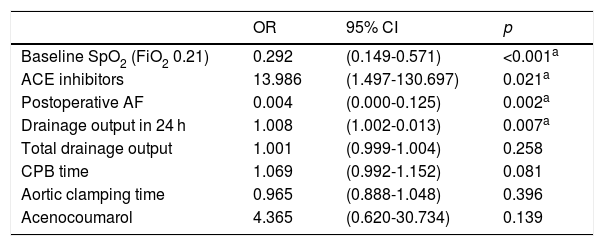
ResultsA total of 93 patients were included and 26 presented UPE. The most common complications after mitral valve MICS were atrial fibrillation (38.7%), UPE (28%) and transient and/or definitive second- or third-degree auriculoventricular block (19.4%). The UPE group had longer ICU stay (3.3 ± 8.0 vs. 1.84 ± 2.23 days) and longer total hospitalization length-of-stay (15.5 ± 34.7 vs. 10.6 ± 7.5 days). The mortality in the UPE group was 3.9%. A significant association was found between the following collected variables and the development of postoperative UPE: preoperative baseline pulse oximetry, preoperative use of ACE inhibitors, postoperative atrial fibrillation and 24 first-hours cumulative chest tube drainage volume on the first 24 h.
ConclusionsThe incidence of UPE is high and its appearance is associated with a longer ICU and total length of stay. More studies are required to understand its pathophysiology and apply measures to help decreasing its appearance.
En los últimos años la cirugía cardíaca mínimamente invasiva (CCMI) se ha desarrollado y aplicado a mayor número de dolencias, especialmente en cirugías sobre la válvula mitral, por presentar resultados comparables a las técnicas convencionales con menor agresividad y tiempo de recuperación. La CCMI que necesita ventilación unipulmonar se ha asociado a la aparición de edema pulmonar unilateral (EPU), que constituye una complicación potencialmente grave. El objetivo es determinar la incidencia de EPU tras CCMI mitral y los factores asociados a su desarrollo.
Material y métodosEstudio observacional descriptivo y unicéntrico. Se analizaron los pacientes tratados con CCMI sobre válvula mitral (minitoracotomía derecha), recogidos de manera consecutiva entre los años 2015 y 2017.
ResultadosSe incluyó a un total de 93 pacientes, de los cuales 26 presentaron EPU. Las complicaciones más habituales tras la CCMI mitral fueron: fibrilación auricular (38,7%), EPU (28%) y bloqueo auriculoventricular de segundo o tercer grado transitorio o definitivo (19,4%). El grupo EPU presentó mayor tiempo de estancia en UCI (3,3 ± 8,0 vs. 1,84 ± 2,23 días) y mayor tiempo total de hospitalización (15,5 ± 34,7 vs. 10,6 ± 7,5 días). La mortalidad en el grupo EPU fue del 3,9%. Se encontró asociación significativa entre las siguientes variables recogidas y el desarrollo de EPU postoperatorio: pulsioximetría basal preoperatoria, uso preoperatorio de IECA, fibrilación auricular postoperatoria y volumen de drenajes en las primeras 24 h.
ConclusionesLa incidencia de EPU es elevada y su aparición se asocia a mayor estancia en UCI y mayor tiempo total de hospitalización. Se requieren más estudios para comprender su fisiopatología y aplicar medidas que ayuden a disminuir su aparición.