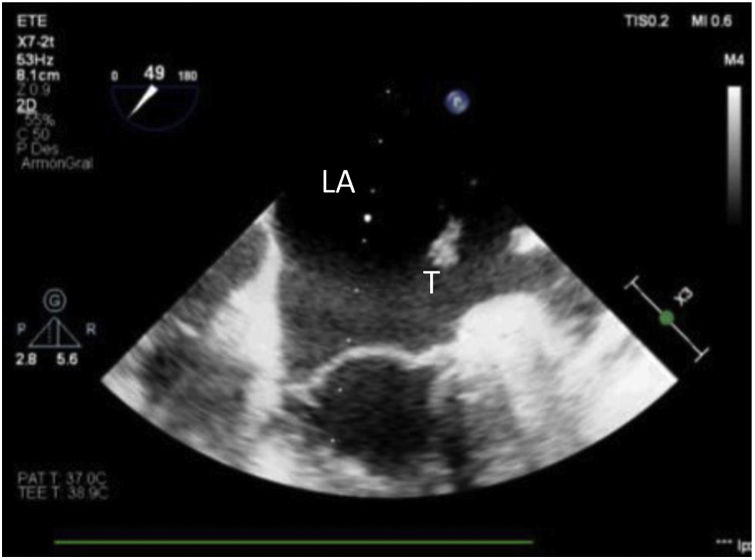
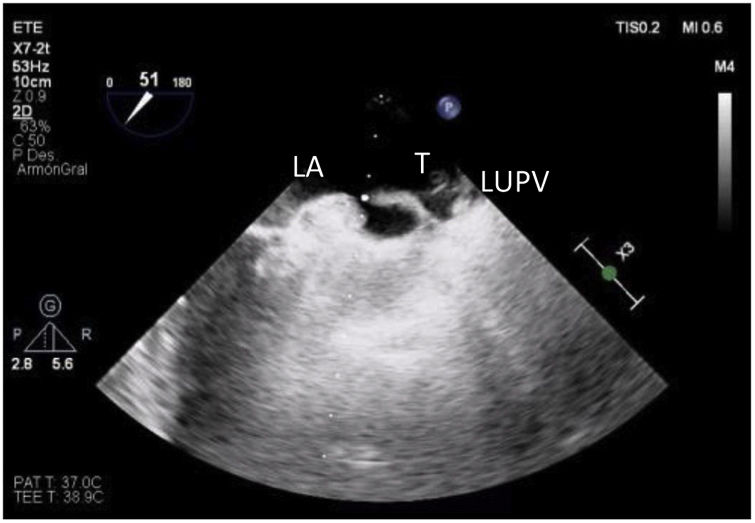
A 61-year-old man with no predisposition to thrombosis underwent sequential double lung transplantation without extracorporeal membrane oxygenation (ECMO) support due to terminal stage COPD. After implantation and reperfusion of both lungs, a complete transoesophageal echocardiography study was performed to check the pulmonary venous anastomosis. The study showed a large, heterogeneous, dense, hyperechoic free-floating mass in the left atrium compatible with a clot in transit from the pulmonary circulation. The surgical team were notified of this finding so that they could reopen the anastomosis and remove the clot to prevent a major complication. There were no clinical manifestations when the patient was awakened.
Un varón de 61 años sin predisposición trombótica es sometido a trasplante bipulmonar como último tratamiento para su EPOC terminal sin soporte de ECMO. Tras el implante y la reperfusión de ambos pulmones, se realizó un examen ecocardiográfico transesofágico completo para comprobar principalmente las anastomosis de las venas pulmonares. En este estudio se identificó una gran masa móvil, hiperecogénica, densa y heterogénea en la aurícula izquierda, compatible con un trombo en tránsito desde la circulación venosa pulmonar. Este hallazgo fue comunicado al equipo quirúrgico inmediatamente para reabrir la anastomosis y retirar el coágulo antes de mayores consecuencias. No hubo manifestaciones clínicas cuando se despertó al paciente.