Throughout history, multiple outbreaks of contagious diseases have created challenges for health sectors, such as the bubonic plague, Asian flu, cholera, Middle East respiratory syndrome, and Ebola. Such events have been associated with the resulting polarisation, racism, guilt, and psychological distress, the most stigmatising historical clinical issues.1 In the current context of the COVID-19 pandemic, the number of healthcare providers involved in dealing with the health crisis is increasing due to a higher number of cases. Such health professionals face challenges such as stigma and discrimination,2 which have been conceptualised and evaluated through the COVID-19 stigma-discrimination complex (SDC-COVID-19).3 Negative social attitudes and behaviour affect various segments of society, including patients, families, and healthcare professionals.4 Stigma adds an unnecessary burden to the lives of healthcare workers and further entrenches occupational burnout.5 Those people who have overcome COVID-19 infection may also be exposed to stigma even if they no longer carry the virus and are not at risk of spreading it.5
Stigma is considered a trait with a negative connotation that is attributable to a person, given the context of the COVID-19 pandemic. Healthcare professionals in Latin America are more stigmatised due to public fear that they are sources of infection.4,5 In outbreaks of infectious disease, fear and misinformation are variables that account for stigma.4 People who feel stigmatised tend to avoid certain behaviour that is perceived to increase stigma due to concerns about social rejection, exclusion, and physical avoidance, such as refusing to take a COVID-19 test, because a positive result may be the label they see as stigmatising.1
Discrimination is an action or behaviour that is directed toward members of certain groups, and refers to a person or people who behave differently (most commonly, unfairly and demeaningly) towards others based solely on their membership in a specific social group.6 Discrimination can manifest itself in various ways, whether verbal or non-verbal. Regardless of how it manifests itself, discrimination leads those affected to feel isolated, rejected and ignored, and to suffer penalisation, harassment and even various forms of violence.
There are certain basic concepts that are closely related to discrimination, namely prejudice and stereotype. As these three concepts are somewhat intertwined, they are often used side by side. Specifically, stereotypes have a cognitive character, prejudices are more affective, and discrimination is considered a behavioural component of reactions based on the social categorisation process.7 Prejudice refers to a generalised and biased attitude towards a social group, a concept that is the engine that drives discrimination, which can arise over and above experience in the face of an extraordinary circumstance such as the COVID-19 pandemic.6,8
This can generate negative results related to health, in view of it being considered a barrier to accessing health services9 that are essential for the prevention and control of COVID-19. For example, people with greater stigmatising beliefs, who may be symptomatic patients, delay medical attention (deterioration of prognosis), since they do not want to come into contact with a health professional, and in turn, there is a delay in the identification of infectious people who do not attend medical centres (increased viral transmission). In addition, it is crucial to consider that such reactions during the pandemic tend to persist over time, since they are more easily consolidated than suppressed.5,9
Likewise, a relationship has been found between pandemic fear and SDC-COVID-19.10 This may be due to inconsistent public health messaging, along with the spread of misinformation on social media, which reinforces further uncertainty and fear of COVID-19 infection. The combined effect of misinformation and fear generates a growing distrust of healthcare workers, which is reflected in greater stigmatising beliefs, and fear is one of the main triggers in the SDC-COVID-19 that can lead to the development of a COVID-19 stress disorder.11
After a brief review of the scientific literature, we found no Latin American studies to date that include dynamic evaluation of the SDC-COVID-19 and pandemic fear through network analysis. We, therefore, believe it is essential to explore how the elements of the two are mutually reinforcing through network analysis in Peruvian students of health sciences.
We conducted an exploratory, correlational, cross-sectional study in the metropolitan city of Lima, Peru, during the second Peruvian pandemic wave in March and April 2021. The following instruments were considered, in their Spanish versions: the Stigma-Discrimination Scale Related to Coronavirus Disease towards Healthcare workers, consisting of five items that evaluate the SDC-COVID-19, and the Fear of COVID-19 Scale (FCV-19S),3 which includes seven items to evaluate the most prevalent fear reactions to COVID-19; this measure has adequate evidence of reliability in the Peruvian sample.12 The internal consistency estimates in the present study were >0.85.
This study included 645 Peruvian adults (79.35% female; mean age, 28.54 years). Due to the social distancing and restricted mobility measures introduced by the government, it became necessary to use online survey methods. Participants were recruited using a snowball sampling technique through social media, such as WhatsApp groups, Facebook and Google groups, and were encouraged to invite their family and friends to take part in the survey. The survey was created and administered using Google Forms and included informed consent, which was obtained from all participants enrolled in the study.
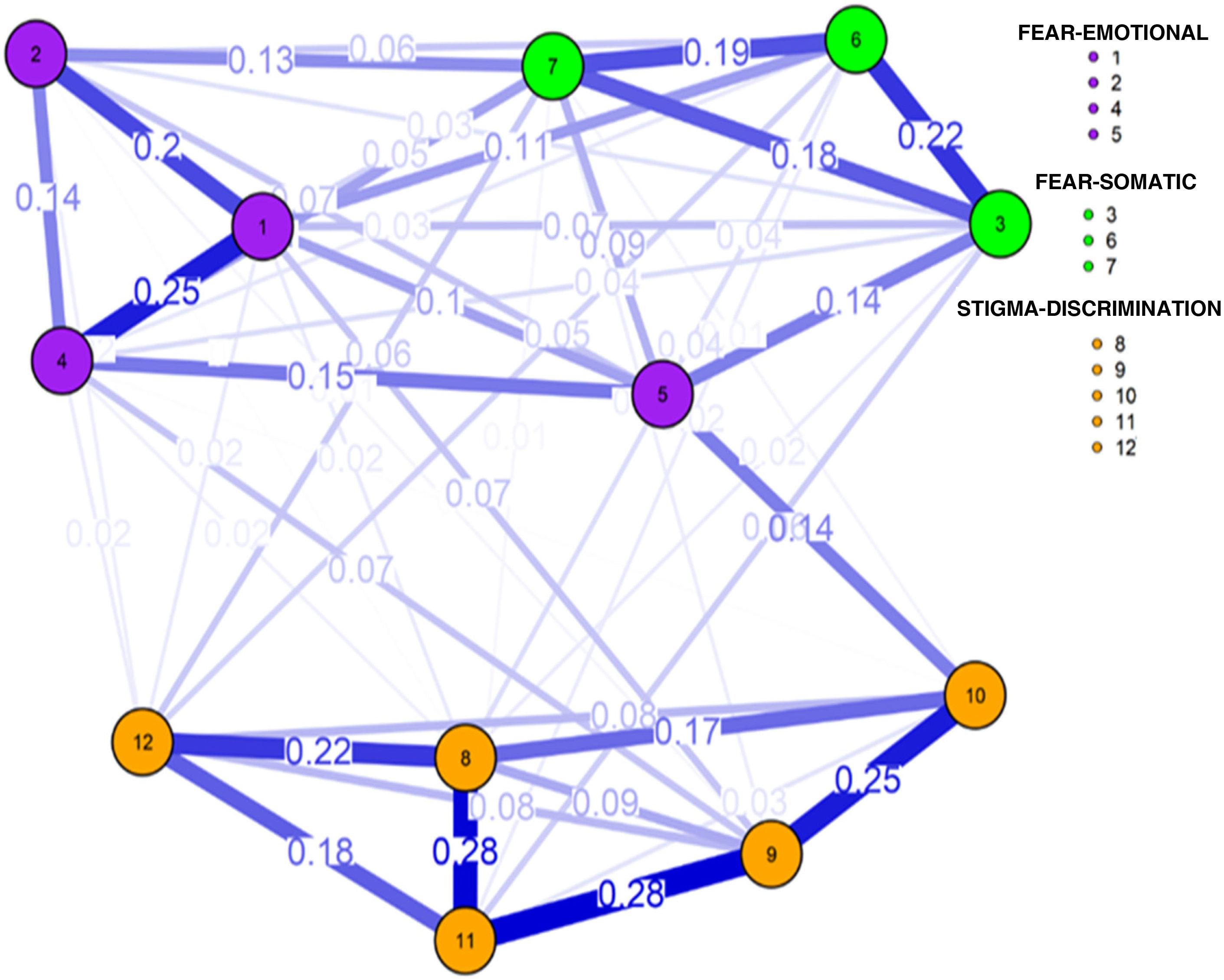
Through the R qgraph package and the graph-fused LASSO (least absolute shrinkage and selection operator), the patterns of the interactive system whose connections represent partial correlations on the network graph were assessed graphically; LASSO estimator allowed spurious relationships to be eliminated.13,14
The items (nodes) are interconnected by lines or edges that represent the partial correlations that tend to be located in the network according to the sum of connections with other nodes.13,14 This network approach favours instrumental and transdiagnostic evaluation in the clinical setting.15 The network approach includes measures of centrality; strength index is the most stable measure for determining the importance of network system components,16 which were grouped into three domains using a network clustering algorithm.15
Table 1 shows the descriptive statistics of the participants' responses to the measures used. These data indicate a greater report in network measures one and four of the FCV-19S and component nine linked to the SDC-COVID-19. Such measures reported the highest measures of network strength centrality.
Mean of the items and strength centrality measures.
| Fear of COVID-19 Scale (FCV-19S) translated into Spanish | Moderate | Strength |
|---|---|---|
| 1. I am very afraid of the coronavirus (COVID-19). | 3.98 | 1.37 |
| 2. Thinking about the coronavirus (COVID-19) makes me uncomfortable. | 3.43 | 0.88 |
| 3. My hands get clammy when I think about the coronavirus (COVID-19). | 2.94 | 0.66 |
| 4. I am afraid of losing my life because of the coronavirus (COVID-19). | 3.99 | 1.01 |
| 5. When I see news and stories about the coronavirus (COVID-19) on social networks, I get nervous or anxious. | 3.51 | 0.90 |
| 6. I can't sleep because I'm worried about catching the coronavirus (COVID-19). | 3.34 | 0.84 |
| 7. My heart races or palpitates when I think about catching the coronavirus (COVID-19). | 3.28 | 0.98 |
| Stigma-Discrimination Scale Related to Coronavirus Disease towards Healthcare workers translated into Spanish | ||
| 8. Should people who work in healthcare services and are in contact with patients with COVID-19 be isolated from society? | 0.65 | 0.81 |
| 9. Am I afraid of being infected by the health personnel I meet on public transport, on the street or at home? | 0.84 | 1.46 |
| 10. Should people who work in healthcare services avoid using public transportation to avoid infecting the population? | 0.68 | 0.99 |
| 11. Should health personnel avoid going home so as not to infect their family? | 0.54 | 0.82 |
| 12. Should health personnel avoid going out so as not to infect the population? | 0.66 | 0.91 |
Fig. 1 shows the highest ratios between measures 8–11, and 9–11 that reinforce the dynamics of CED-COVID-19. The strongest connections in the FCV-19S were measures one and four, related to symptoms of an emotional nature. The association between items three and six, of a somatic nature, also stood out. Sixteen associations were reported between the measures of the two study instruments. Item 12 reported five interdomain connections, while components one, three and six presented three relationships of this type. The following stood out for their greater magnitude: item one—“When I see news and stories about the coronavirus (COVID-19) on social networks, I get nervous or anxious”—and item 10—“Should people who work in healthcare services avoid using public transportation to avoid infecting the population?"—, which refers to a greater state of anxiety being reinforced by the stigmatising belief that healthcare workers should avoid using public transportation to avoid infection.
Other important relationships were between measure nine—“I am afraid of being infected by the health personnel I meet on public transport, on the street or at home”—and item four—“I am afraid of losing my life because of the coronavirus"—and one—“I am very afraid of the coronavirus”—, which implies that the emotional state of general fear and fear of dying due to COVID-19 is more prevalent than greater prejudice (affective character) of fear of infection by health personnel. The relationship of element 12—“Should health personnel avoid going out so as not to infect the population?”—with somatic symptoms six—“I can't sleep because I'm worried about catching the coronavirus”—and seven—“My heart races or palpitates when I think about catching the coronavirus”—also stand out, which reinforces a greater negative attitude of physical avoidance and social limitation towards medical personnel.
The network centrality measures one, four and nine present higher values of connection between both domains, which enables the guiding of a path of investigation of such constructs. These findings allow us to understand that the emotional nature of fear reinforces stigmatising beliefs towards healthcare workers. In particular, the component of fear of dying shows the prevalence of awareness of death, linked to the theory of terror management by Greenberg and Arndt,17 who explain that all stigmatising behaviour can be considered as an action to avoid the fear of death, where people tend to have a greater prejudice of rejection and social exclusion towards those who symbolise a threat to self-esteem and the individual's world view. Thus, in the context of the current pandemic, healthcare professionals may be stigmatised as sources of infection and a greater threat to survival.8
This study is essential to consolidate future research that explores the development of the two concepts and their relationships with other variables with a greater negative impact due to COVID-19.18,19
Conflicts of interestThe author has no conflicts of interest to declare.