Carcinoid syndrome is a relatively rare condition that may affect the liver and the right heart. Some of these cases may require surgical treatment with a multidisciplinary approach.
Case reportWe report the case of a patient with progressive dyspnoea, arterial hypotension and facial flushing, diagnosed with liver and cardiac involvement from carcinoid syndrome. The patient was taken to surgery in two different occasions, first for metastatic liver resection, and then to subsequent cardiac surgery for tricuspid valve replacement.
ConclusionsWe report here a case review, including the clinical course, the intra-operative management, and the information available in the literature regarding which procedure to perform initially in these types of cases which are not very common in clinical practice.
El síndrome carcinoide es una condición relativamente rara que puede afectar el hígado y el corazón derecho. En algunos pacientes se requiere tratamiento quirúrgico y un manejo multidisciplinario.
Presentación del casoPresentamos una paciente con diagnóstico de síndrome carcinoide con compromiso hepático y cardíaco quien inició con disnea progresiva hasta el reposo, hipotensión arterial y rubor facial. La paciente fue llevada a cirugía en dos tiempos: la resección de las metástasis hepáticas inicialmente y, en un segundo tiempo, cirugía cardíaca para el cambio de la válvula tricúspide. Ambas intervenciones se realizaron con éxito y sin complicaciones.
ConclusiónPresentamos aquí una revisión del caso, la evolución y el manejo intraoperatorio y la información disponible en la literatura para decidir cual procedimiento se debe realizar en primera instancia, ya que estos casos no son frecuentes en la práctica clínica.
A carcinoid tumour is a tumour of malignant behaviour arising from neuroendocrine system cells, with the ability to produce bioactive substances such as vasoactive peptides and amines. The incidence of carcinoid tumours is approximately 1 case for every 100,000 people, and close to 50% go on to develop carcinoid syndrome.1,2 However, a more recent report found a much higher incidence of 3.65 cases for every 100,000.3
The most common sites for carcinoid tumours are the gastrointestinal tract (67.5%) and the lungs (25.3%). In the gastrointestinal tract, the sites most commonly affected are the small bowel, the rectum and the stomach.4
The vasoactive hormones secreted by the tumour give rise to the so-called “carcinoid syndrome”, characterised by facial flushing, arterial hypotension, diarrhoea, pruritus and bronchospasm. These vasoactive substances include serotonin, 5-hydroxytryptamine, 5-hydroxytryptophan, kallicrein, hystamine, prostaglandins, adrenocorticotopic hormone, insulin, catecholamines, parathormone, gonadotropins and substance P.5
Once the intestinal wall is invaded, carcinoid tumour cells may extend beyond it and spread through the lymphatic and vascular systems. Tumour cells reach the liver through the portal circulation, reducing the liver's ability to metabolise the products derived from these tumours. When tumour cells are implanted in the liver, their humoral products may reach the right heart through the inferior vena cava (IVC).5 Pulmonary stenosis and tricuspid regurgitation are usually the predominant cardiac manifestations of this syndrome.
The current pharmacological management of carcinoid syndrome includes somatostatin analogues such as octreotide and lanreotide and, on occasions, high doses of octreotide are required for adequate symptom control.6
Cardiac surgery is indicated when the patient develops heart failure, specifically right ventricular failure and/or when there is severe valve dysfunction.7 Cardiac surgery offers definitive treatment for these patients and, over the past two decades, it has resulted in a significant reduction in mortality associated with this disease.8,9
Few cases are described in the medical literature regarding the surgical treatment of liver metastases and heart disease in carcinoid syndrome.10,11 This case report describes a two-stage surgical treatment of carcinoid tumour metastatic disease: liver resection in the first stage, and tricuspid valve replacement in the second stage.
Clinical caseInformed consent was obtained from the patient for the discussion and publication of this case.
A 45-year-old female patient presented with progressive dyspnoea even at rest, associated with sudden episodes of hot flashes, diarrhoea, cough and facial flushing that started in the previous five months. There were no significant findings in her clinical history, and her surgical history included appendectomy and cholecystectomy performed more than ten years before, with no anaesthetic or surgical complications.
The patient was admitted to the hospital for work-up considering that the initial physical examination revealed the presence of dyspnoea and, on auscultation, a grade 4/4 holosystolic murmur.
In the initial trans-thoracic echocardiogram (TTE), left ventricular ejection fraction (LVEF) was 60%, right ventricular function was normal, but the right ventricle was significantly dilated with severe tricuspid regurgitation associated with moderate pulmonary insufficiency and mild pulmonary stenosis. Cardiac catheterisation revealed normal coronary arteries. Pulmonary artery pressures were normal and only a moderate elevation of the inferior vena cava and right atrial (25mmHg) pressures was found, due to tricuspid regurgitation and end-diastolic right ventricular pressure increase (35/18mmHg), probably due to pulmonic valve insufficiency.
Abdominal computed tomography imaging showed a liver mass 14cm in diameter involving segments II and IVa, as well as other smaller liver lesions; predominant lesions were in hepatic segments I, II, VII, VIII and X. There was no description of the presence of portal hypertension and no description of IVC status.
A tumour mass was also found 1.7cm from the ileocecal valve. It was presumably the primary tumour, which disappeared with the use of somatostatin analogues and did not require surgical excision. These findings, together with urinary levels of 5-hydroxyindoleacetic acid (a by-product of 5-hydroxytryptamine metabolism) higher than 500ng in 24h confirmed the diagnosis of carcinoid syndrome.
Following diagnosis, the patient initiated treatment with octreotide (Sandostatin Novartis, Basel, Switzerland) 30mg IM every 28 days, followed by preoperative transarterial chemoembolisation four months before the surgery of the main liver metastases of the carcinoid tumour, in an attempt at debulking before taking it to surgical excision.
Twelve months after the start of treatment and in view of evident symptom improvement, the case was submitted for discussion of the order of the procedures. It was decided to start with hepatectomy in order to avoid potential damage to tricuspid valve replacement from liver metastases while waiting for their resection. The patient was taken to liver surgery and underwent partial right hepatic lobectomy with wedge resection of segments II and IVa.
Upon arrival to the surgical preparation area, the patient was administered 500μg of subcutaneous octreotide.
Fentanyl 2mcg/kg, propofol 1.5mg/kg and cisatracurium 10mg, were used for anaesthesia induction, and tracheal intubation was accomplished uneventfully. A radial artery access was established with a 20G catheter, and a 9French Swan-Ganz introducer (Arrow-Teleflex Corp. Morrisville, NC, USA) was used for right internal jugular access under ultrasound guidance. Maintenance anaesthesia consisted of an oxygen-air mix plus sevoflurane at an end-tidal concentration of 1.5–2.5% (Baxter Health Care Deerfield Il, USA).
The hepatic artery and the portal vein were clamped at the level of the hepatoduodenal ligament, followed by IVC clamping. The latter was not well tolerated by the patient and resulted in an almost immediate drop in blood pressure and cardiac output. This prompted the decision of performing a femoral-jugular veno-venous bypass (without IVC occlusion) with a flow rate ranging between 0.5 and 2.3L/min, maintained during 80min. Cannulation of the femoral vein and the internal jugular vein was performed with a 16Fr arterial perfusion cannula (Edwards Lifescience OptiSite, Irvine, CA 92614-5686, USA). Jugular cannulation was performed by the anaesthetist (double cannulation of the right internal jugular vein under ultrasound guidance) and the femoral cannulation was performed by the surgical and perfusion team. Baseline activated clotting time (ACT) was 121s and was maintained at around 350s with the use of intravenous heparin. In this patient, anticoagulation was managed in accordance with our institutional anticoagulation protocol for bypass circulation.
Central venous pressure (CVP) was maintained at around to 25mmHg, mean arterial pressure was maintained between 60 and 70mmHg with the use of crystalloids and colloids (5% albumin), blood products and vasopressors.
Intra-operative blood loss was approximately 5L and the patient received 6units of red blood cells, 4units of fresh frozen plasma and two doses (500mL) of recombinant human albumin. The patient was transferred to the Intensive Care Unit (ICU) in a stable condition, with an infusion of low-dose noradrenaline. Post-operatively, the patient developed bilateral pleural effusions, more significant on the right side, which were evacuated using chest tubes. The patient remained in the ICU until the tenth post-operative day and was discharged from hospital on day 15.
The report on the liver lesions revealed abundant necrotic material and the presence of argentaffin cells, confirming the diagnosis of a carcinoid tumour. A new TTE was performed four months after liver surgery, showing trivial pulmonic valve abnormalities and a smaller right ventricular dilatation, but the same degree of severe tricuspid regurgitation. Octreotide treatment was maintained during those months, and the patient's symptoms improved almost completely.
Six months after liver resection, the patient was taken back to surgery for tricuspid valve exchange. Anaesthetic induction was achieved with midazolam 5mg, fentanyl 500mcg, propofol 60mg and rocuronium 100mg. Tranexamic acid and octreotide infusions were initiated at 1g/hr and 500mcg/h, respectively. Invasive monitoring included an arterial line and a 9French central catheter (Arrow-Teleflex Corp., Morrisville, NC, USA) placed under ultrasound guidance in the right internal jugular vein. Anaesthesia maintenance was achieved using an oxygen-air mix plus sevoflurane at an end-tidal concentration of 1.5–2.5%. The transoesophageal echocardiography probe was introduced during surgery but did not show new findings different from those of the previous transthoracic echocardiogram, namely, right ventricular dilatation with no functional abnormality and tricuspid annular plane systolic excursion (TAPSE) greater than 20mm, and tricuspid valve diameter of 36mm. Bypass circulation was maintained with no complications during 69min, with 39min of aortic clamping. The tricuspid valve was replaced with a porcine bioprosthetic valve No. 29mm (Medtronic, Minneapolis, USA). There were no major complications during surgery and there was no need to use blood products or vasopressors. At the end of the valve replacement surgery, the patient was transferred to the ICU, with no ensuing complications.
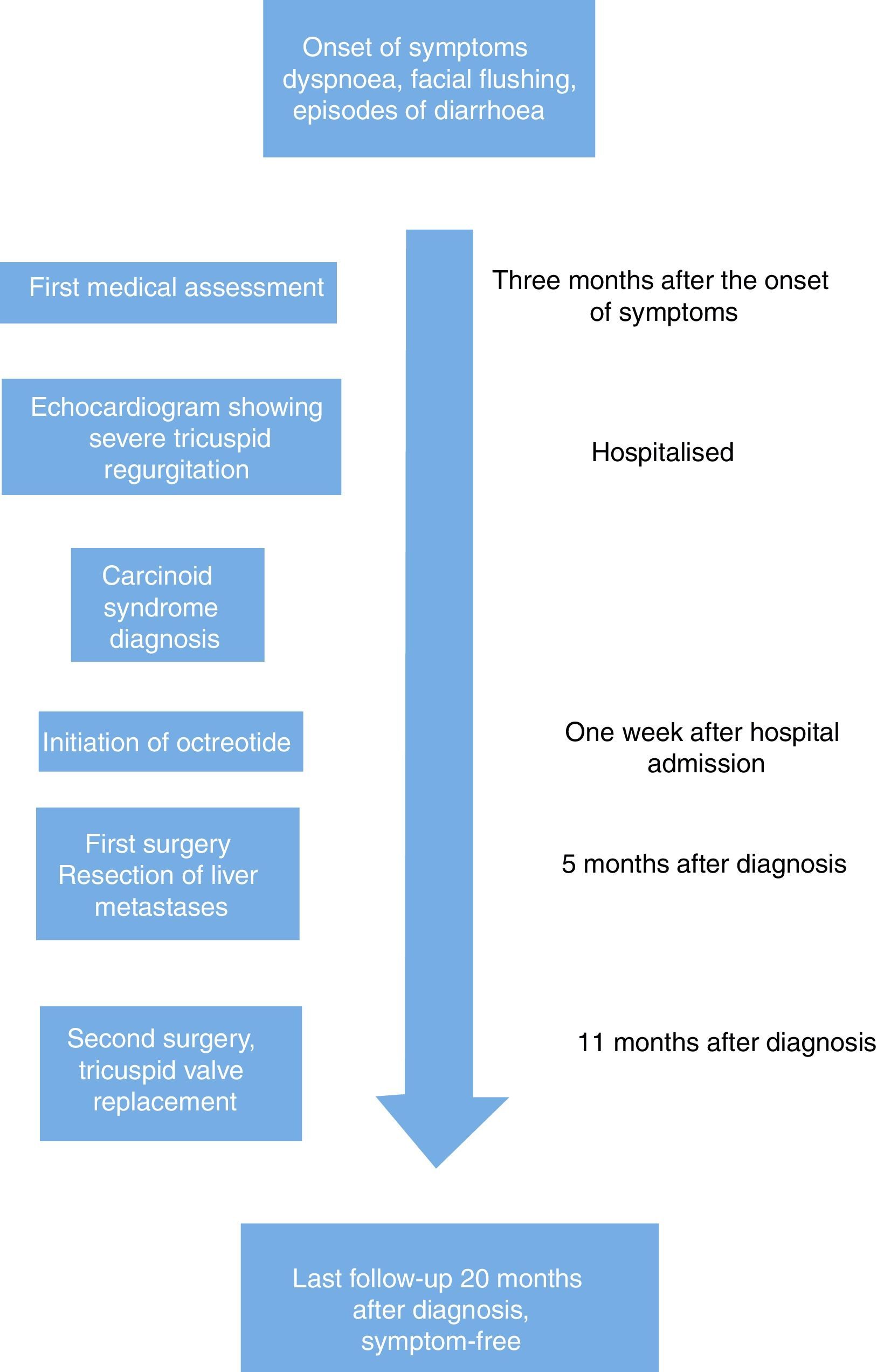
On the 12-month follow-up visit, the patient did not report cardiac or other symptoms associated with carcinoid syndrome and there were not detectable urinary levels of 5-HIAA on that date (Fig. 1).
DiscussionCarcinoid tumours are slow-growing neuroendocrine tumours of low incidence in the general population and unpredictable clinical course. The incidence of these tumours has increased substantially over the past decade due to the availability of better and faster diagnostic tools.3
Liver metastases are present in 50–70% of cases, 20% of which will develop carcinoid syndrome and, among the patients with carcinoid syndrome, 50% will have cardiac manifestations.12 After liver involvement, the next step in the disease is right heart compromise. The mechanism by which fibrous plaques form in the right cardiac cavities, endocardium, valves and sub-valvular apparatus is not clearly understood, but it could be related to the influence of certain growth factors released by this type of tumour, favouring the development of fibrous tissue in the endocardium.5
There is right heart compromise in the vast majority of cases of carcinoid syndrome, the pulmonic and tricuspid valves being the most severely affected13 because of the deposition of fibrous tissue in the right endocardium. Although uncommon, left heart involvement may also be found in cases of carcinoid tumour of bronchogenic origin14 or in patients with patent foramen ovale.15 The interventricular septum may also be compromised as an unusual manifestation of this disease.16
The indications for surgical treatment of the cardiac disease produced by carcinoid syndrome are heart failure and/or severe tricuspid regurgitation. Patients with heart and liver involvement are usually taken first to tricuspid valve replacement in order to lower high pressures in the right ventricle and the inferior vena cava, reducing liver venous congestion and, consequently, also reducing the risk of difficult-to-control bleeding in case of partial hepatectomy.17 Elevated right heart pressures increase the risk of bleeding during hepatectomy, as reported by Dobson et al.18
In the case presented here, the patient was taken first to partial hepatectomy despite confirmation of increased pressures in the superior vena cava and the right ventricle during the initial catheterisation. This decision was made by a multidisciplinary team (cardiac surgeon, hepatobiliary surgeon, transplant anaesthetist, cardiovascular anaesthetist) based on the fear of the cardiovascular surgeons of worsening tricuspid valve compromise due to liver metastasis, and based also on the severe symptoms exhibited by the patient as a result of the carcinoid syndrome. Initial liver metastasis resection may help lower the levels of hormones and vasoactive substances, leading to a reduction or even resolution of symptoms associated with the carcinoid tumour and, consequently, to a peri-operative management less prone to complications like the onset of a carcinoid crisis during the second intervention.
The use of veno-venous bypass has been previously described in this type of surgery as well as in liver transplant.11,19 Difficult-to-control bleeding during hepatectomy may be managed successfully with the use of this type of venous blood flow diversion technique. The goal of veno-venous bypass is to divert flow to the right atrium and improve venous return. In this case, it was used because the patient did not tolerate temporary IVC clamping and showed marked haemodynamic instability. The flow rate maintained during veno-venous bypass ranged between 0.5 and 2.3, and this large variation may be attributed to intra-operative bleeding and subsequent hypovolemia. Flow data were taken from the perfusion form. Flow rate variations may be due to massive bleeding or to other factors not specified in this case. High right atrial pressures may also have influenced the occurrence of massive intra-operative bleeding.
The most important challenges during anaesthesia in carcinoid tumour surgery include the onset of a carcinoid crisis and the development of right heart failure during the procedure.20 Carcinoid crisis manifests as arterial hypotension, generalised flushing and increased airway pressures. The first step in treatment is to avoid the use of drugs that may induce histamine release such as long-acting opioids (morphine and meperidine) or muscle relaxants (rocuronium, vecuronium). Arterial hypotension must be treated with volume replenishment ideally guided by dynamic indicators, and the use of inotropes or vasopressors such as phenylephrine and noradrenaline, which are indicated for maintaining adequate perfusion pressure for vital organs and counteracting the vasodilation induced by most of the peptides secreted by this type of tumour. Octreotide is the best option currently available for the prevention and treatment of crises associated with a carcinoid tumour and it needs to be used as part of this intervention, sometimes in high doses.
ConclusionCarcinoid syndrome is an uncommon disease that involves the heart in some cases, mainly right heart valves. It gives rise to significant pathophysiological changes that may pose a challenge for anaesthetic management during liver as well as cardiac surgery. The anaesthetist must be aware and prepared for managing these cases with the use of drugs such as octreotide, vasopressors and inotropes.
Defining the severity of the disease and the degree of liver involvement, as well as the presence and grade of cardiac valve compromise and ventricular function are very important steps in planning and preparation. Also very important is the use of bypass circulation tools and veno-venous bypass which may be very useful for perioperative management of this infrequent but highly complex disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe authors declare not having received funding for the preparation of this article.
Conflict of interestThe authors declare having no conflict of interest.
Please cite this article as: Giraldo M, Harle C, Lopera-Velásquez LM, Dobkowsky W. Tratamiento quirúrgico de la enfermedad metastásica del síndrome carcinoide: hepatectomía parcial usando un bypass veno-venoso y posterior cambio valvular tricúspide. Reporte de caso. Rev Colomb Anestesiol. 2017;45:344–348.