Parkinson’s disease (PD) is catastrophic, chronic, and neurodegenerative. In advanced stage requires a permanent informal caregiver. The adaptation of the caregiver to their role is unknown, a fundamental aspect to guarantee the quality of care.
ObjectivePrepare a healthcare proposal with standardized language to promote the adaptation of informal caregivers of Parkinson’s patients to their social role.
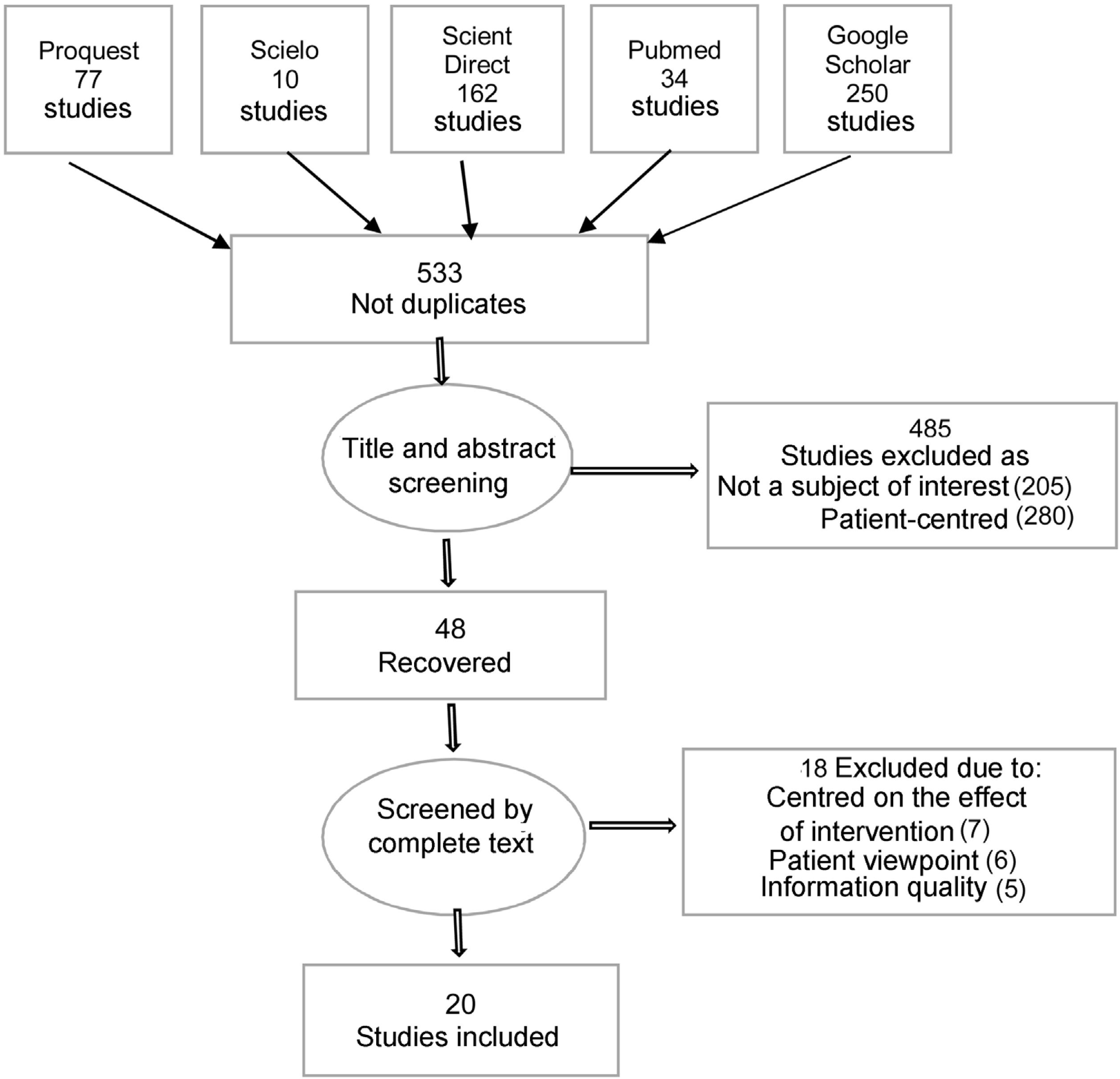
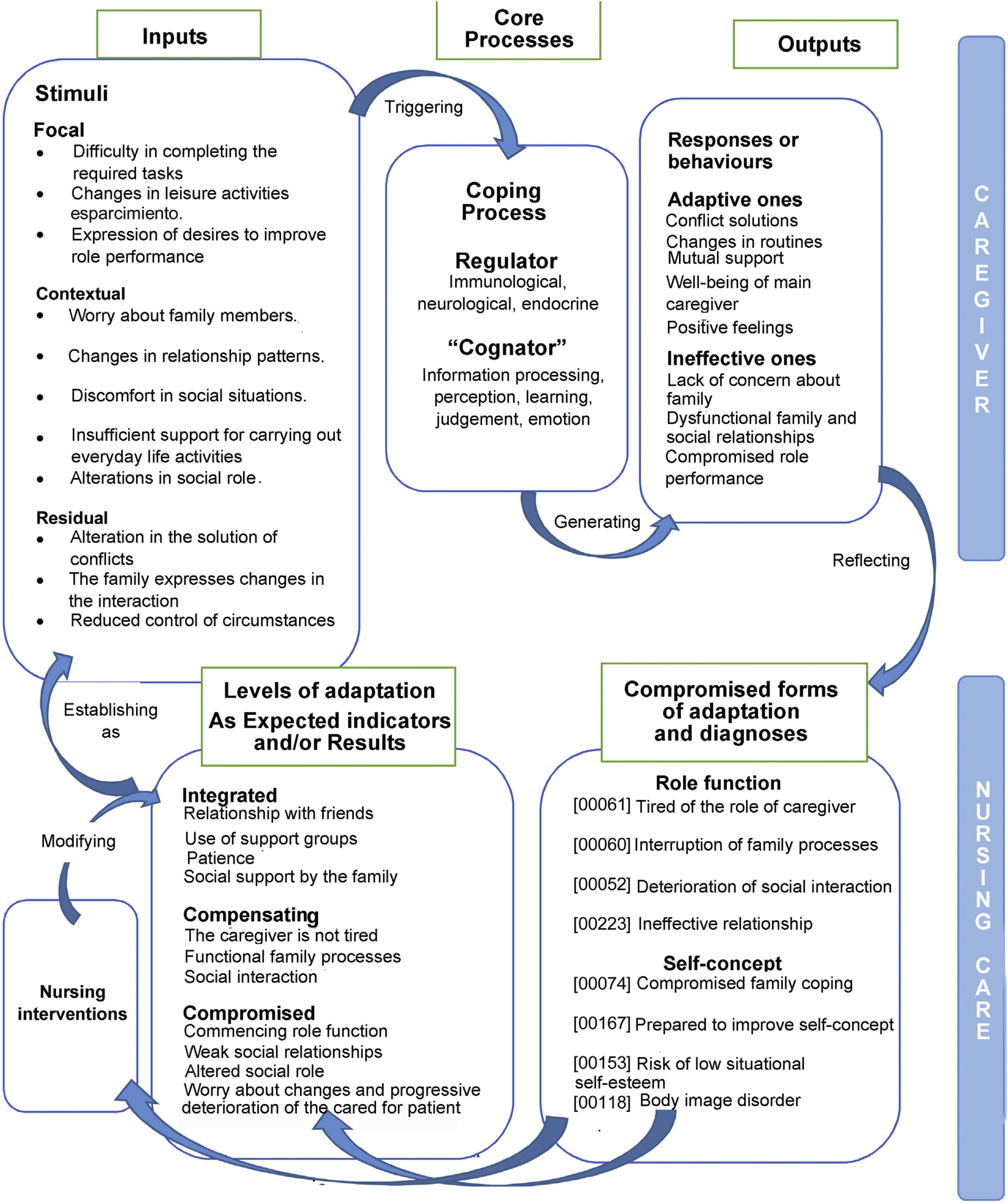
MethodsTwo-phase study: Literature review and preparation of a Care Proposal. Search in Proquest, Scielo, Scient Direct, Pubmed, and Google Scholar databases, in English, Spanish and Portuguese languages, for the last five years. Descriptors: Parkinson’s disease, Chronic disease, caregivers, adaptation, nursing process. The proposal articulates the Calixta Roy adaptation Model with the Nursing Process using NANDA-NOC-NIC taxonomy.
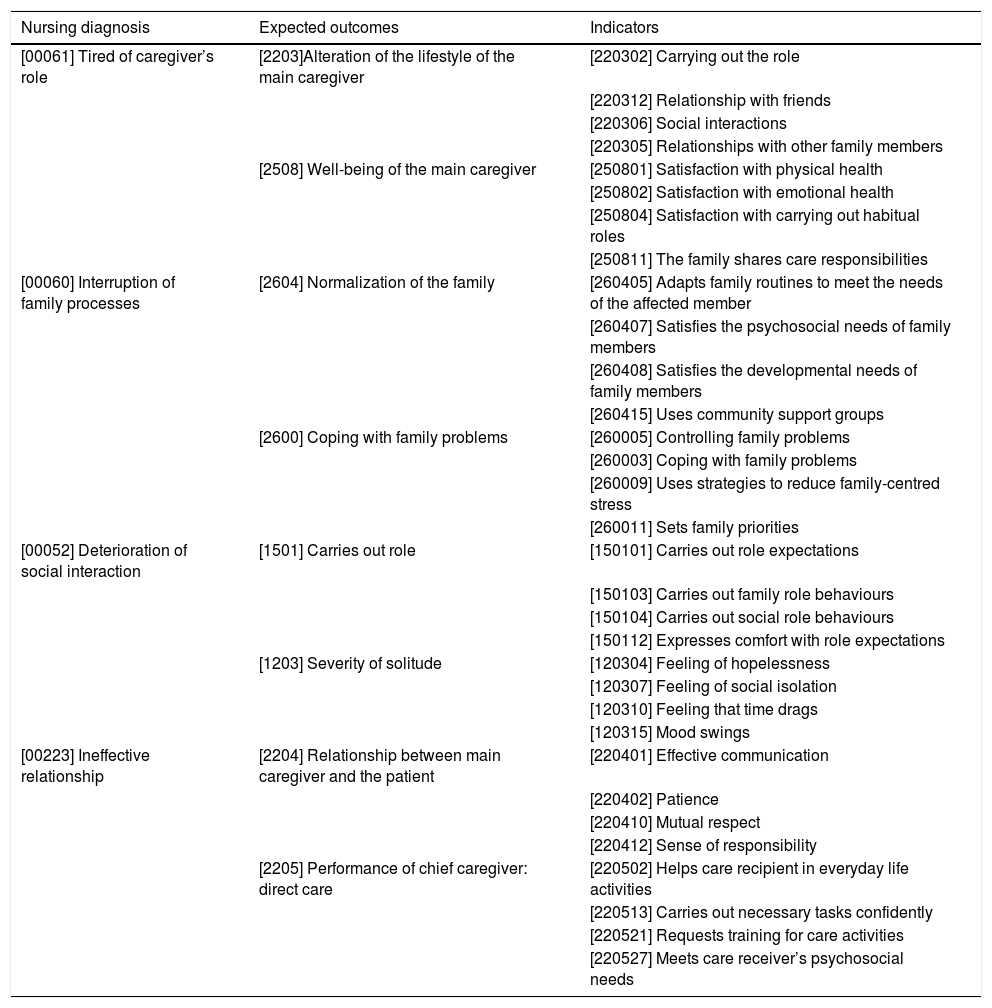
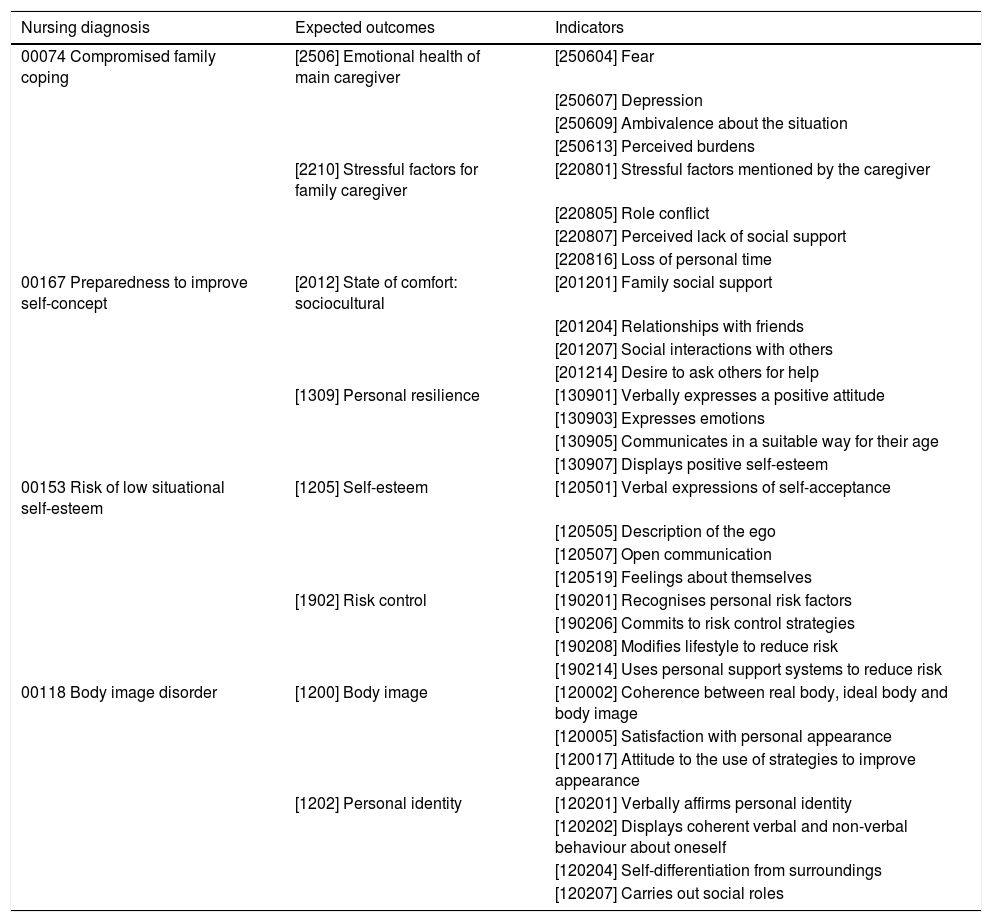
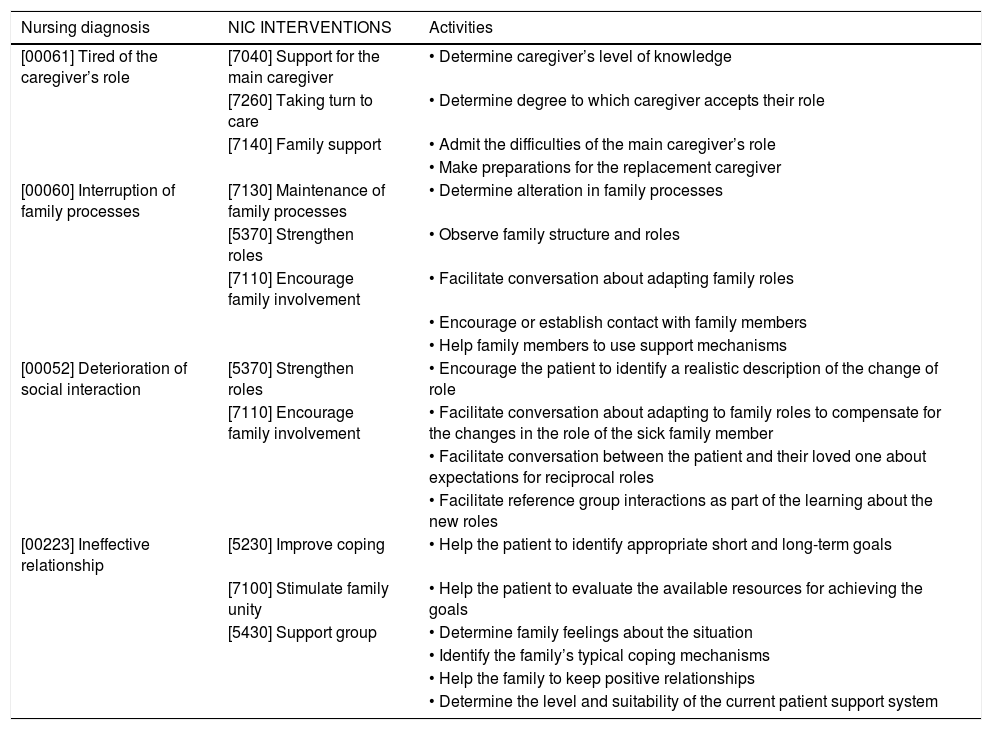
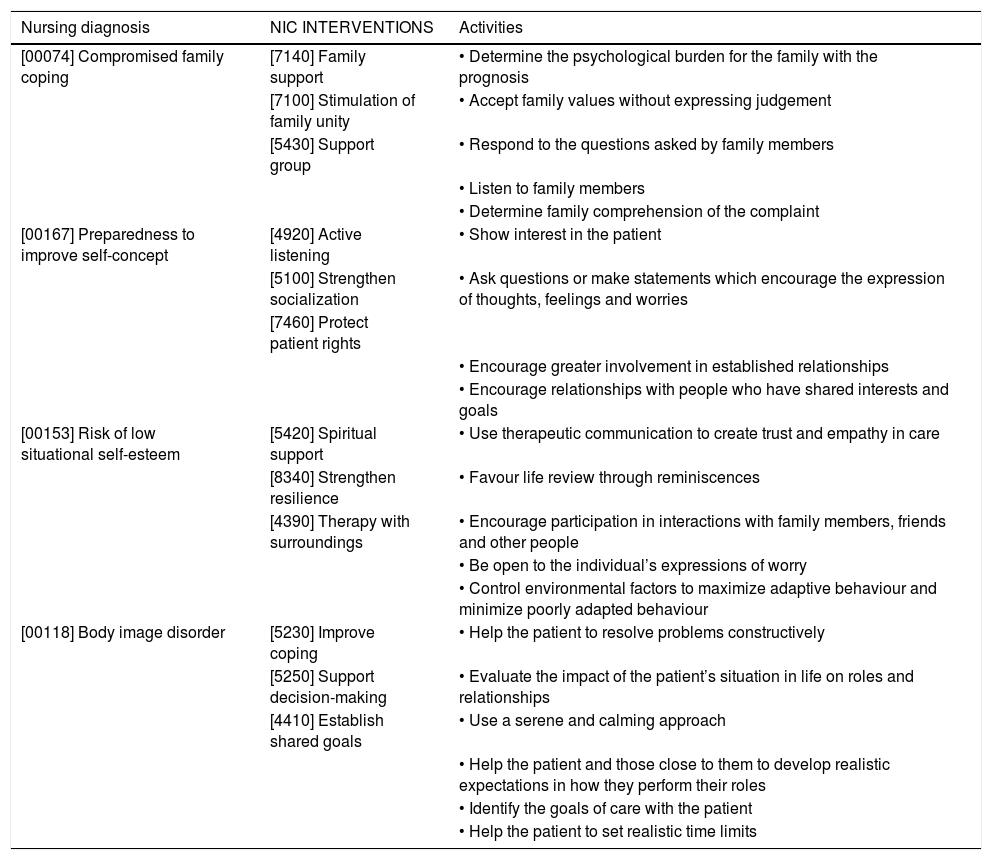
ResultsFew publications on coping and adaptation of caregivers and on the Nursing Process to caregivers using standardized language. Committed adaptation modes: Role function and Self-concept. Relevant nursing diagnoses: Tiredness of the caregiver role, Interruption of family processes, Impairment of social interaction, Ineffective relationship, Compromised family coping, Willingness to improve self-concept, Risk of low situational self-esteem, and Body image disorder. Two NOC outcomes and three NIC interventions were linked for each diagnosis.
ConclusionsThe articulation of the Calixta Roy Adaptation Model with the standardized language NANDA-NOC-NIC is an innovative contribution to the disciplinary and professional development of Neurological and Community Nursing. The proposal makes it possible to monitor the levels of adaptation of the informal caregiver and intervene in a timely manner.
La enfermedad de Parkinson (EP) es catastrófica, crónica y neurodegenerativa. En etapa avanzada requiere un cuidador informal permanente. Se desconoce la adaptación del cuidador a su rol, aspecto fundamental para garantizar la calidad asistencial.
ObjetivoElaborar una propuesta de cuidado con lenguaje estandarizado para fomentar la adaptación de cuidadores informales de pacientes con Parkinson a su rol social.
MétodosEstudio en dos fases: revisión de la literatura y elaboración de una propuesta de cuidados. Búsqueda en las bases de datos Proquest, Scielo, Scient Direct, Pubmed y Google Scholar, en idiomas inglés, español y portugués, últimos cinco años. Descriptores: Enfermedad de Parkinson, Enfermedad crónica, cuidadores, adaptación, proceso de enfermería. La propuesta articula el Modelo de adaptación de Calixta Roy con el Proceso de Enfermería utilizando taxonomía NANDA-NOC-NIC.
ResultadosEscasas publicaciones sobre afrontamiento y adaptación de cuidadores y sobre Proceso de Enfermería a cuidadores utilizando lenguaje estandarizado. Modos de adaptación comprometidos: Función de rol y Autoconcepto. Diagnósticos de enfermería relevantes: Cansancio del rol de cuidador, Interrupción de procesos familiares, Deterioro de la interacción social, Relación ineficaz, Afrontamiento familiar comprometido, Voluntad de mejorar el autoconcepto, Riesgo de baja autoestima situacional y Trastorno de la imagen corporal. Se vincularon dos resultados NOC y tres intervenciones NIC para cada diagnóstico.
ConclusionesLa articulación del Modelo de Adaptación de Calixta Roy con el lenguaje estandarizado NANDA-NOC-NIC es aporte innovador al desarrollo disciplinar y profesional de la Enfermería Neurológica y Comunitaria. La propuesta permite monitorear los niveles de adaptación del cuidador informal e intervenir de manera oportuna.