To improve language in aphasic patients after a recent ischaemic stroke using computer applications for mobile devices (tablet) for 30 days and to establish whether length of use influences this improvement.
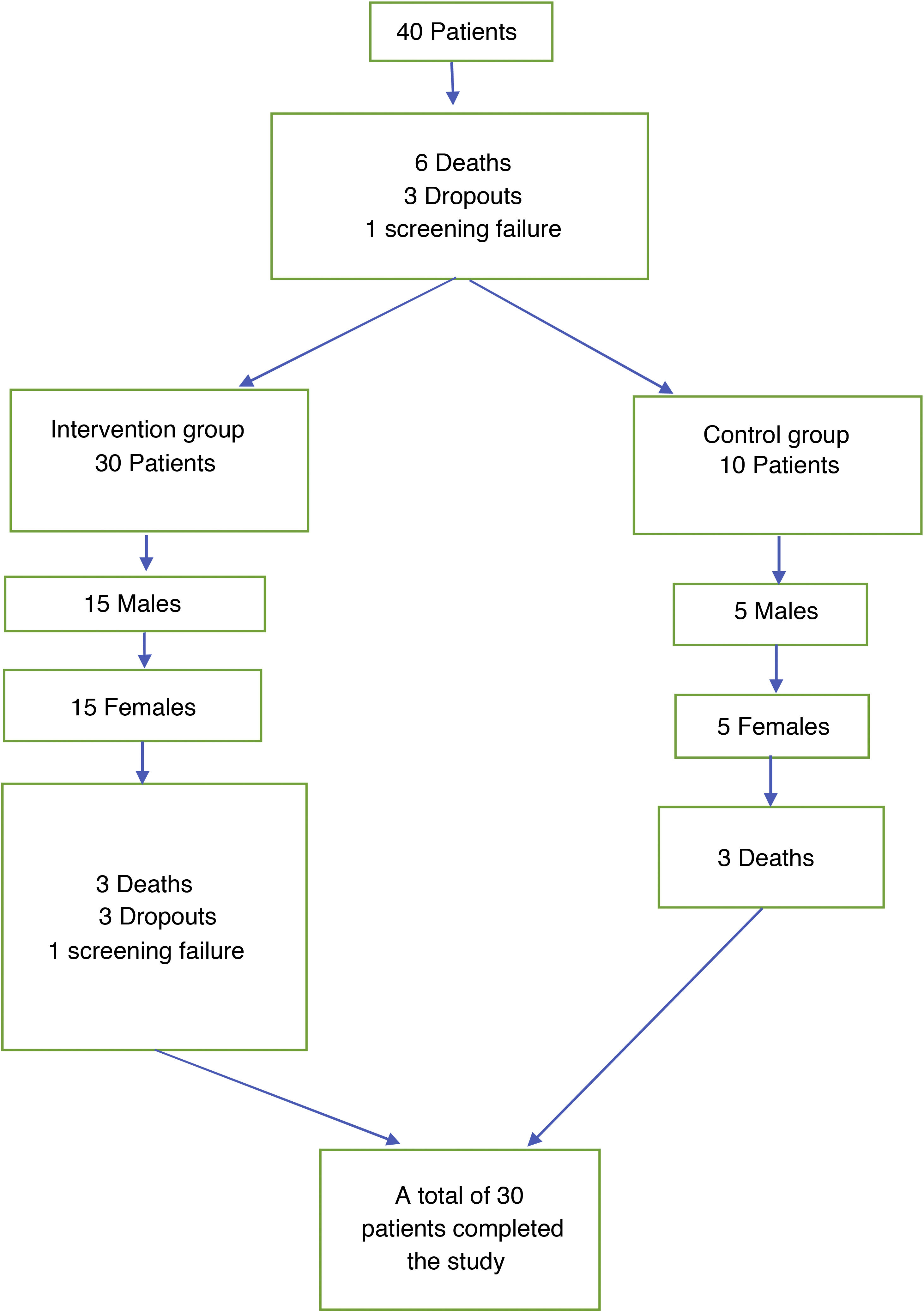
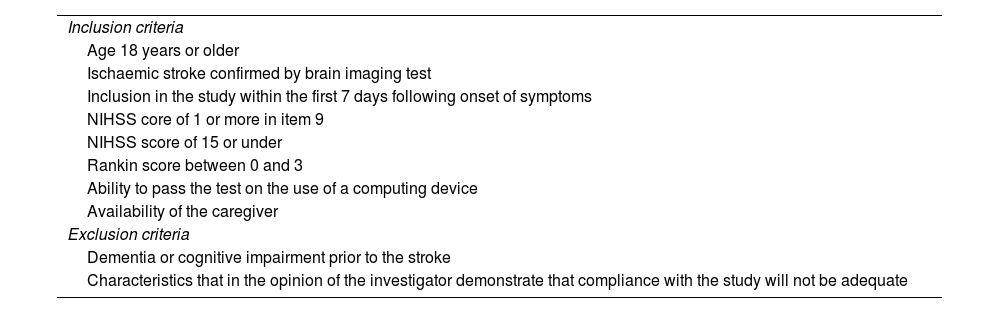
MethodRandomised, prospective, single-centre clinical trial with two intervention groups, one of which was a control group. Aphasic patients were included within a maximum of 7 days after an ischaemic stroke. The intervention group used tablet-specific software for 30 days. Language improvement was assessed using the Mississippi Aphasia Screening Test (MAST).
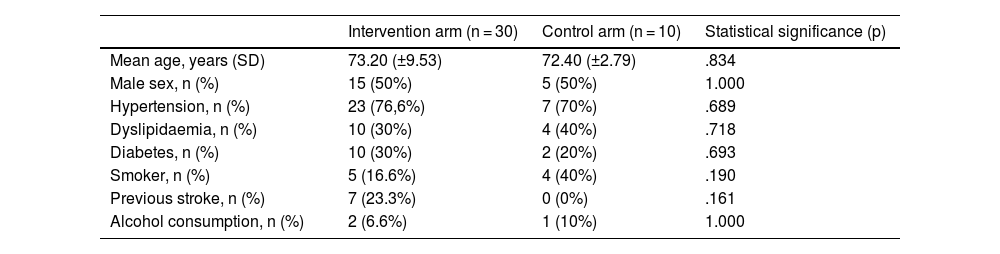
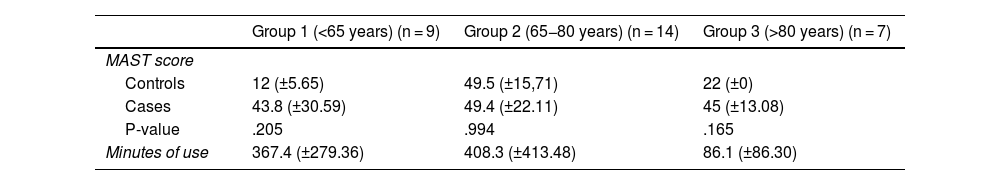
ResultsThe sample was 40 patients, mean age 73 years (± 10.2). Fifty percent were women. Patients were equally divided between the 2 groups. Mean device use was 311.8 (±334.6) minutes after the end of 30 days, with a final mean improvement in MAST of 46.5 (±22.3) points in the intervention group and 34.8 (±21.7) in the control group (p = .233). Adjusting for age, the results indicate that the patients who tend to improve the most are those under 65 years of age (43.8 (±30.5) points, p = .205). We were unable to demonstrate significant differences between the two groups.
Discussion and/or conclusionsThe results obtained in the study suggest that new technologies can be an effective tool for language recovery, especially in young patients. Multicentre studies with a larger sample size and younger patients may be able to demonstrate the usefulness of this new tool.
Establecer la mejoría del lenguaje en pacientes afásicos tras un ictus isquémico reciente, usando aplicaciones informáticas para dispositivos móviles (tablet) durante 30 días y establecer si el tiempo de uso influye en dicha mejoría.
MétodoEnsayo clínico aleatorizado, prospectivo, unicéntrico con dos grupos de intervención, uno de ellos control. Se incluyeron pacientes afásicos en un plazo máximo de 7 días tras un ictus isquémico. El grupo de intervención utilizó un software específico para tablet durante 30 días. La mejoría del lenguaje se evaluó mediante el Mississipi Aphasia Screening Test (MAST).
ResultadosLa muestra fue de 40 pacientes, edad media 73 años (±102). El 50% eran mujeres. Los pacientes se repartieron de forma equitativa entre los 2 grupos. El uso medio de los dispositivos fue de 311,8 (±334,6) minutos tras finalizar los 30 días, con una mejoría media final en el MAST de 46,5 (±22,3) puntos en el grupo de intervención y de 34,8 (±21,7) en el grupo control (p = 0,233). Al ajustar por edad, los resultados indican que los pacientes que más tienden a mejorar son los menores de 65 años (43,8 (±30,5) puntos, p = 0,205). No conseguimos demostrar diferencias significativas entre ambos grupos.
Discusión y/o conclusionesLos resultados obtenidos en el estudio sugieren que las nuevas tecnologías pueden ser una herramienta eficaz para la recuperación del lenguaje sobre todo en pacientes jóvenes. La realización de estudios multicéntricos con un mayor tamaño muestral y pacientes más jóvenes tal vez podrían conseguir demostrar la utilidad de esta nueva herramienta.
Article
Diríjase al área privada de socios de la web de la SEDENE, (https://sedene.com/revista-de-sedene/ ) y autentifíquese.