Pioneer publications discourage the use of ulnar access after failed attempt to obtain ipsilateral radial access.
MethodsProspective efficacy and safety registry comparing the incidence of bleeding and vascular complications in patients with an initial intention to use ulnar access and those who used this access after a failed attempt to cannulate the ipsilateral radial artery.
ResultsBetween May 2007 and December 2013, 11,825 invasive coronary procedures were performed at a single center, 473 (4%) of them by ulnar access. In 65 cases, the ulnar artery cannulation was preceded by a failed attempt to obtain the ipsilateral radial access. The technical success rate was higher than 98%, with low complication rates, mostly due to superficial hematomas, with no differences between groups. There were no cases of major bleeding related to the access site, pseudoaneurysm, arteriovenous fistula or injury to the adjacent ulnar nerve.
ConclusionsThe ulnar access is a safe and effective alternative to perform selected invasive coronary procedures, despite previous attempts to obtain the ipsilateral radial access.
Segurança e Factibilidade do Acesso Ulnar Após Falha do Acesso Radial Ipsilateral
IntroduçãoPublicações pioneiras desencorajam o uso do acesso ulnar após falha na tentativa de obtenção do acesso radial ipsilateral.
MétodosRegistro prospectivo de eficácia e segurança comparando a ocorrência de sangramento e complicações vasculares entre casos com intenção inicial de utilizar o acesso ulnar e aqueles cujo emprego desse acesso se deu após falha na canulação da artéria radial ipsilateral.
ResultadosEntre maio de 2007 e dezembro de 2013, foram realizados 11.825 procedimentos coronários invasivos em um único centro, 473 (4%) deles pelo acesso ulnar. Em 65 casos, a canulação da artéria ulnar foi precedida por falha na obtenção do acesso radial ipsilateral. A taxa de sucesso da técnica foi superior a 98%, sendo baixo o número de complicações, em sua maioria decorrente de hematomas superficiais, sem diferença entre os grupos. Não houve casos de sangramento grave relacionado à via de acesso, pseudoaneurisma, fístula arteriovenosa ou lesão do nervo ulnar adjacente.
ConclusõesO acesso ulnar representa uma alternativa segura e eficaz para a realização de procedimentos coronários invasivos selecionados, a despeito de tentativa prévia de obtenção do acesso radial ipsilateral.
The choice of access route for the performance of invasive coronary procedures constitutes an important step in an approach involving the reduction of vascular complications and severe bleeding. Although the femoral technique remains predominant, there is a consistent increase in the adoption of transradial approach, which is known to promote greater comfort and safety for the patient. 1,2
Spasm, anatomical variations and lower pulse amplitude subsequent to the reuse of the route are mechanisms of failure in obtaining the radial access.3 In this context, the ulnar artery is a viable alternative, capable of offering benefits similar to those arising from the radial technique, as demonstrated in previous studies.4,5 However, pioneer papers on this topic discourage the use of ulnar access after a failed cannulation of the ipsilateral radial artery.6,7
The objective of this analysis was to evaluate the feasibility and safety of performing coronary interventions through ulnar artery in situations of failed attempt to use the ipsilateral radial artery.
METHODSConsecutive patients referred to the performance of invasive coronary procedures by the ulnar route were included in a prospective registry of safety and efficacy. The primary objective of the study was to compare clinical characteristics, procedure-related characteristics, and occurrence of bleeding and vascular complications among patients with an original intent of puncturing the ulnar artery (Group 1) and those whose use occurred after failure to obtain the ipsilateral radial access (Group 2).
DefinitionsIn accordance with the classification of the Bleeding Academic Research Consortium (BARC), 8 severe bleeding was defined as type 3 – (3a) bleeding with hemoglobin decrease≥3 and < 5g/dL or red blood cells transfusion; (3b) bleeding with hemoglobin decrease≥5g/dL, or cardiac tamponade, or bleeding requiring surgical intervention, or bleeding requiring intravenous vasoactive drug use; (3c) intracranial hemorrhage, or subcategories confirmed by autopsy, imaging examination, or lumbar puncture, or intraocular bleeding with vision impairment; or Type 5 – (5a) likely fatal bleeding; (5b) definitive fatal bleeding.
Hematomata were graded according to the classification of Early Discharge After Transradial Stenting of Coronary Arteries (EASY) study: type I, ≤ 5cm in diameter; type II≤10cm in diameter; type III, > 10cm, without reaching the elbow; type IV, hematoma extending beyond the elbow; type V, any hematoma with ischemic hand injury. 9 Complications related to the puncture site, besides hematomata, included asymptomatic arterial occlusion, ulnar nerve lesion, acute ischemia, pseudoaneurysm, arteriovenous fistula, need for vascular repair, and surgical site infection.
The success of the technique was defined as the completion of the diagnostic or therapeutic procedure without switching to another access route. Asymptomatic artery occlusion was defined as the interruption of arterial blood flow with no manifestations of ischemic compromise of the limb. Ulnar nerve lesion was defined as the occurrence of motor and/or sensory disturbances in the limb where the procedure was performed, with persistent signs and/or symptoms for a period≥24 hours, as a result of direct injury by accidental puncture of the nerve or extrinsic compression by hematoma and/or pseudoaneurysm.
The duration of the procedure and the fluoroscopy time were obtained from the arterial puncture to sheath withdrawal.
Ulnar techniqueAfter wrist hyperextension and infiltration of 1 to 2mL of 2% lidocaine, the ulnar artery was punctured at a point 1 to 3cm proximal to the pisiform bone, using a needle with polyethylene catheter #20-22 with the Seldinger technique. After puncture, a 0.019” guidewire was introduced, followed by a small skin incision with scalpel blade #11 and insertion of a short 5 or 6F sheath. A solution containing 5000IU heparin sulfate and 10mg of isosorbide mononitrate was injected through the length of the sheath. At the end of the procedure, the sheath was immediately removed and hemostasis was obtained with a compressive dressing with porous adhesive elastic bandage in the diagnostic procedures, and with an adapted selective compressive bracelet in the therapeutic procedures. Clinical examination of the puncture site and an evaluation of ulnar pulse at discharge were performed, and the use of Doppler ultrasound was reserved for suspected complications.
Statistical analysisQualitative variables were summarized as absolute frequencies and percentages, and quantitative variables were described as means±standard deviations. To compare the groups, the chi-squared or Fisher exact test for qualitative variables was used; Student’s t test was used for quantitative variables. P values < 0.05 were considered significant.
RESULTSBetween May 2007 and December 2013, 11,825 invasive coronary procedures were carried out in a single center, of which 10,761 (91%) by radial access, 591 (5%) by femoral access and 473 (4%) by ulnar access – the latter group constitutes the analyzed sample.
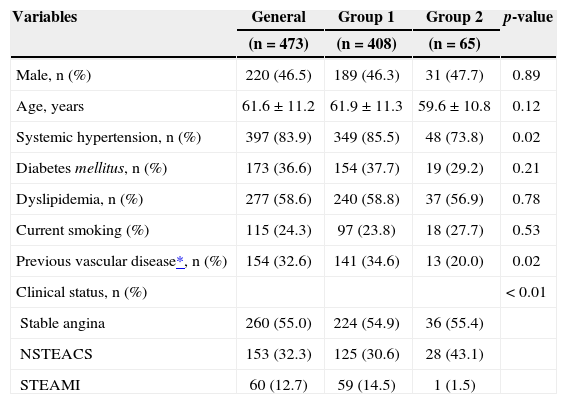
In both groups, there was a preponderance of female patients, mean age of 61±11.2years, and a high prevalence of diabetes. Overall, both groups showed similar characteristics, with the exception of previous hypertension and vascular disease, less frequent in patients with radial-to-ulnar switching. These patients also exhibited lower percentage of primary percutaneous coronary interventions (Table 1).
Baseline clinical characteristics
| Variables | General | Group 1 | Group 2 | p-value |
|---|---|---|---|---|
| (n=473) | (n=408) | (n=65) | ||
| Male, n (%) | 220 (46.5) | 189 (46.3) | 31 (47.7) | 0.89 |
| Age, years | 61.6±11.2 | 61.9±11.3 | 59.6±10.8 | 0.12 |
| Systemic hypertension, n (%) | 397 (83.9) | 349 (85.5) | 48 (73.8) | 0.02 |
| Diabetes mellitus, n (%) | 173 (36.6) | 154 (37.7) | 19 (29.2) | 0.21 |
| Dyslipidemia, n (%) | 277 (58.6) | 240 (58.8) | 37 (56.9) | 0.78 |
| Current smoking (%) | 115 (24.3) | 97 (23.8) | 18 (27.7) | 0.53 |
| Previous vascular disease*, n (%) | 154 (32.6) | 141 (34.6) | 13 (20.0) | 0.02 |
| Clinical status, n (%) | < 0.01 | |||
| Stable angina | 260 (55.0) | 224 (54.9) | 36 (55.4) | |
| NSTEACS | 153 (32.3) | 125 (30.6) | 28 (43.1) | |
| STEAMI | 60 (12.7) | 59 (14.5) | 1 (1.5) |
NSTEACS: acute coronary syndrome without ST-segment elevation; STEAMI: acute myocardial infarction with ST-segment elevation.
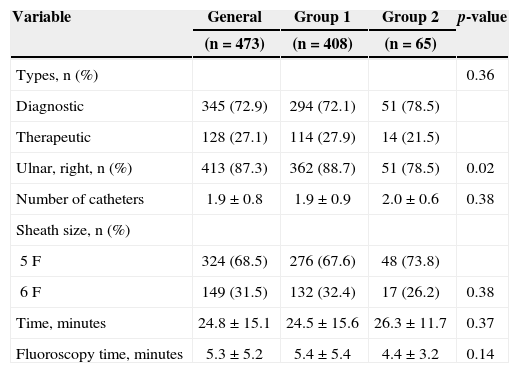
Diagnostic procedures accounted for 73% of cases, and the right ulnar approach was used in four of each five patients, but it was less frequently used after radialto-ulnar access switching (88.7% vs. 78.5%; p=0.02). The number of catheters used in the procedures was similar, and the 5F sheath was used in at least twothirds of the interventions. Procedure and fluoroscopy times did not differ between groups (Table 2).
Characteristics of procedures
| Variable | General | Group 1 | Group 2 | p-value |
|---|---|---|---|---|
| (n=473) | (n=408) | (n=65) | ||
| Types, n (%) | 0.36 | |||
| Diagnostic | 345 (72.9) | 294 (72.1) | 51 (78.5) | |
| Therapeutic | 128 (27.1) | 114 (27.9) | 14 (21.5) | |
| Ulnar, right, n (%) | 413 (87.3) | 362 (88.7) | 51 (78.5) | 0.02 |
| Number of catheters | 1.9±0.8 | 1.9±0.9 | 2.0±0.6 | 0.38 |
| Sheath size, n (%) | ||||
| 5F | 324 (68.5) | 276 (67.6) | 48 (73.8) | |
| 6F | 149 (31.5) | 132 (32.4) | 17 (26.2) | 0.38 |
| Time, minutes | 24.8±15.1 | 24.5±15.6 | 26.3±11.7 | 0.37 |
| Fluoroscopy time, minutes | 5.3±5.2 | 5.4±5.4 | 4.4±3.2 | 0.14 |
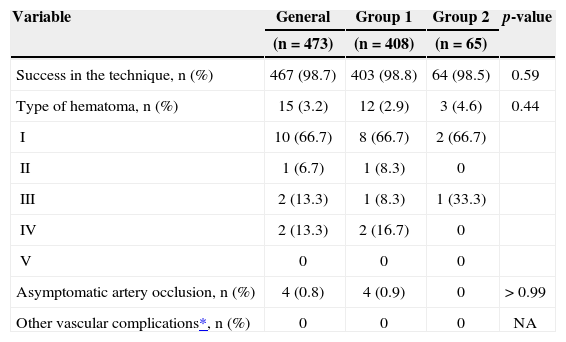
The success rate for the technique was above 98%, with low complication rates, mostly due to superficial hematomata, without ischemic hand injury. There were no cases of severe bleeding related to the access route, pseudoaneurysm, arteriovenous fistula, nor adjacent ulnar nerve lesion (Table 3).
Comparisons between procedures performed by ulnar access as the initial option and after failure of the ipsilateral radial approach (outcomes of efficacy/safety)
| Variable | General | Group 1 | Group 2 | p-value |
|---|---|---|---|---|
| (n=473) | (n=408) | (n=65) | ||
| Success in the technique, n (%) | 467 (98.7) | 403 (98.8) | 64 (98.5) | 0.59 |
| Type of hematoma, n (%) | 15 (3.2) | 12 (2.9) | 3 (4.6) | 0.44 |
| I | 10 (66.7) | 8 (66.7) | 2 (66.7) | |
| II | 1 (6.7) | 1 (8.3) | 0 | |
| III | 2 (13.3) | 1 (8.3) | 1 (33.3) | |
| IV | 2 (13.3) | 2 (16.7) | 0 | |
| V | 0 | 0 | 0 | |
| Asymptomatic artery occlusion, n (%) | 4 (0.8) | 4 (0.9) | 0 | > 0.99 |
| Other vascular complications*, n (%) | 0 | 0 | 0 | NA |
Pioneer reports on the use of ulnar artery as a new option for vascular access in invasive procedures are characterized by the small number of patients and by warnings about this choice in situations of failure to obtain the ipsilateral radial access, prior cannulation of the same route in the past and a mandatory evaluation of palmar arch permeability by Allen test or plethysmography. 6,10,11 With the greater experience obtained primarily by groups that favor and adopt the radial technique as their first choice, and which consequently migrated to the ulnar technique when faced with the need for an alternative route, its safety and efficacy were demonstrated, even in borderline situations. 12−14
A prospective registry recently published evaluated 240 patients undergoing diagnostic and therapeutic vascular procedures by ulnar access, all with previous documentation of ipsilateral radial access occlusion. 15 The authors reported a success rate of 97%, requiring switching to femoral access in 3% of cases. Despite the occurrence of spasms in 8% of patients and of a rate of asymptomatic occlusion of the ulnar artery in 3%, there was no report of hand ischemia after 30 days of follow-up. Indeed, the presence of the deep palmar arch in more than 95% of anatomical studies and the vascular reserve capacity of the circulation in the hand, demonstrated by collaterals’ recruitment in laboratory models, would justify the absence of ischemic complications after the procedure.16
In this series, whose main results were previously published, 4 it was demonstrated that, despite the spasm of the radial artery in 80% of cases of failure and of subsequent switching to the ipsilateral ulnar artery, this route was used without negative implications for patients, especially regarding the risk of ischemic injury to the hand. The possibility of carrying out more quickly this procedure in emergency situations, for example, primary percutaneous coronary intervention, in which the need to prepare the contralateral upper limb or a lower limb would cause additional delay for the initiation of the procedure; the use of the same materials previously employed in the attempted radial artery puncture; and the greater comfort, both for the patient and for the surgeon, would justify the option by the ulnar route.
Similar results were reported in a series of 12 patients undergoing systematic palmar arch angiography at the end of invasive procedures by ipsilateral ulnar access, after failure of an attempted radial access procedure. 13 In seven cases, the radial artery was patent, indicating a temporary spasm. One patient exhibited chronic occlusion of the radial artery, with collateral branches from both arteries. In the remaining four cases, there was an acute radial occlusion, possibly caused by dissection, but with clear demonstration of collateral circulation to the palmar arch, without clinical evidence of ischemia.
In our daily practice, in face of the inability to use the radial approach, we advocate the use of the ulnar access regardless of the finding of occlusion or of failed cannulation of the ipsilateral radial artery; the only requirement is the presence of a large and easily identifiable pulse, which represents less than 5% of our total procedures. Without a previous evaluation of the anatomy and of the wrist, the choice in favor of the ulnar technique will result in a greater number of attempts at punctioning, more time spent in gaining access, an excessive duration of the examination and a failure rate close to 45%.17,18
Among the limitations of our study, we emphasize its non-random nature, the sample size and, above all, that our cases come from a single center, by surgeons acquainted with the ulnar and radial accesses, used in 95% of procedures, as well as the availability of materials dedicated to these routes, such as hydrophilic catheters and sheaths, and with an experienced multidisciplinary team, trained in the handling of hemostasis.
CONCLUSIONSThe ulnar access represented a safe and effective alternative to performing invasive coronary procedures in selected cases, even after failed attempts to reach the ipsilateral radial access.
CONFLICTS OF INTERESTThe authors declare no conflicts of interest.
SOURCE OF FINANCINGNone.