The COVID-19 pandemic and the consequent declaration of a state of alarm have required changes throughout the entire health system and diagnostic imaging departments are no exception.
In our department, these circumstances led to an immediate restructuring of the working dynamics of our group of imaging technologists that had an important role in the front lines of the battle. To ensure that these new needs were met, the staff had to be trained and distributed into different areas and working groups; moreover, new protective measures and protocols had to be adopted in the working environment. We also defined different care circuits for patients with COVID-19 and those without COVID-19, incorporating new technologies, adapting existing resources to the new scenario, and creating a circuit for the rapid diagnosis of COVID-19. This paper also provides detailed recommendations for organizing radiology departments in the case of new outbreaks of COVID-19.
La pandemia de COVID-19 y la consecuente declaración del estado de alarma crearon una obligada modificación dentro del ámbito de la sanidad en su totalidad y los servicios de radiodiagnóstico no quedaron exentos.
En nuestro servicio conllevó una reestructuración inmediata de la dinámica de trabajo del colectivo de técnicos superiores en imagen para el diagnóstico (TSID), que tuvo un papel destacado en la primera línea de batalla. Para lograr satisfacer las nuevas necesidades, se tuvo que formar al personal, distribuirlo en diferentes áreas y grupos de trabajo y adoptar nuevas medidas de protección y cuidado en el ámbito laboral. También se adecuaron los diferentes circuitos de atención asistencial (COVID-19 vs. NO COVID-19), incorporando tecnología, adaptando los recursos existentes al nuevo escenario y creando un circuito rápido de diagnóstico COVID-19. Así mismo, se detallan las recomendaciones que se han de tener en cuenta sobre la estrategia organizativa dentro del servicio de radiología ante un posible rebrote de la pandemia.
Radiology plays a prominent role in the multidisciplinary management of COVID-19.1 Although reverse transcription-polymerase chain reaction (RT-PCR) in nasal and pharyngeal secretion samples is considered the test of choice for diagnosis,2 radiological tests, especially chest X-ray and computed tomography (CT), are vitally important tools for the diagnosis, prognosis and monitoring of patients with COVID-19.3–5 This demonstrates the validity and enormous usefulness of these techniques in the face of new diagnostic challenges.
The rapid spread of the pandemic, combined with a lack of foresight on the part of government authorities, resulted in a health crisis scenario.6 The collateral effects of the pandemic must also be taken into account. The increase in deaths secondary to preventable and treatable diseases is among them. The rapid increase in demand has overloaded the healthcare system, leaving gaps in other important areas. It is vital to maintain essential services so as not to deepen the damage to society.
Like the rest of the health system, radiology departments had to adapt to the pandemic7, which required hasty decision-making (often improvised) and the preparation of dynamic contingency plans. In this exceptional situation, exceptional measures had to be taken and implemented quickly, in order to cope with the substantial demand generated by COVID-19.
Within radiology departments, the fight against COVID-19 was primarily fought on the front lines, with senior diagnostic imaging technicians (SDITs) acting as the main agents on the battlefront.8 They certainly rose to the occasion, thanks to their professionalism, determination and commitment. Organising SDIT staff was (and still is) a challenge during the pandemic. The imperative to meet new healthcare demands without neglecting essential basic radiological care forced us to push our team to its limits, with a fundamental reliance on strict personal care and efficient teamwork.
Our centre is a university hospital, with a capacity of 697 beds, and covers a demographic area of 493,382 inhabitants (2019). The Diagnostic Imaging Department is made up of 42 adjunct specialists and 12 resident physicians in training, organised by subspecialisation, and has 86 SDITs.
The objective of this article is to describe, detail and illustrate the different changes and decision-making processes carried out among the SDIT staff of the Diagnostic Imaging Department at our institution due to the COVID-19 pandemic, as an example of organisation and coordination in a health crisis situation.
Decision-making processes and management of SDIT staffTo cope with the difficulties caused by the pandemic, an Executive Crisis Committee was formed with the backing of the Hospital Executive Directorate. The committee was made up of: the Medical Directorate, the Research and Innovation Directorate, the Nursing Directorate and the Human Resources Directorate. It reported on decision-making to the Finance and Services Directorate. Within the Diagnostic Imaging Department, decision-making was a joint effort between the Department Directorate and the University Diploma in Nursing (UDN)/SDIT Staff Management and Administration Directorate, who reported weekly to the Executive Crisis Committee and conveyed the directives to the heads of the different radiology service areas (abdominal, neuroradiology, breast and gynaecologic, musculoskeletal, paediatric, thoracic, and vascular and interventional).
During the pandemic, staff were divided into two groups of 43 people, group A and group B. These groups carried out their work on-site on an every-other-week basis. Each group was divided into two teams: “COVID-19” (70%) and “Non−COVID-19” (30%), depending on the work sector to which the staff were assigned. In order to form these teams, the Occupational Health Department was contacted, and they, along with the UDN/SDIT Staff Management and Administration Directorate, segregated staff based on various risk factors.9 SDITs with potential risk factors for severe COVID-19 due to underlying diseases (e.g. chronic lung diseases, obesity, diabetes or cardiovascular disease) were assigned to performing tests in patients not suspected of having COVID-19 (“Non−COVID-19” team).
Due to the marked increase in demand for certain tests (e.g. chest X-rays) in the emergency setting, these areas had to be bolstered. To this end, SDIT staff from other specific radiological areas, which were closed or engaged in limited care provision, were made available. Before being placed in their target areas, staff went through a brief period of basic training in that area and did a refresher course on safety measures in relation to personal protective equipment (PPE). In this way, the different shifts were always made up of a professional with more experience (having worked in that area for a longer period of time) and a professional with less experience redirected from another area engaged in less care activity during the pandemic (e.g. vascular and interventional radiology, breast radiology, magnetic resonance imaging or ultrasound).
The areas with the highest care burden were also strengthened by relocating staff with dual SDIT and UDN qualifications. Professionals who normally worked as UDNs were placed as SDITs in areas of greatest need. In our case, there were seven of these: three UDNs from vascular and interventional radiology, two from magnetic resonance imaging, one from breast radiology and one from ultrasound.
Staff training and protectionAt the beginning of the pandemic, Europe reported high numbers of infections among health staff.10 This was attributed to different factors. Among them, the global problem of a shortage of protective equipment and a lack of awareness of transmission by asymptomatic cases in the initial phases of the pandemic might have led to infections in health staff who were not properly protected.11 In mid-May, in Spain, this percentage was as high as 24.1% of all infections in the general population.12
Among the functions of the Executive Crisis Committee, in line with the guidelines and protocols established by the health authorities, informing and training health staff were priorities.13,14
Bearing in mind that health workers are considered an at-risk population15, multiple information sessions were held for all staff (both in clinical care and in auxiliary fields) in which details about the virus SARS-CoV-2 and the disease COVID-19 were explained, emphasising routes of transmission and precautions to be taken by health staff.
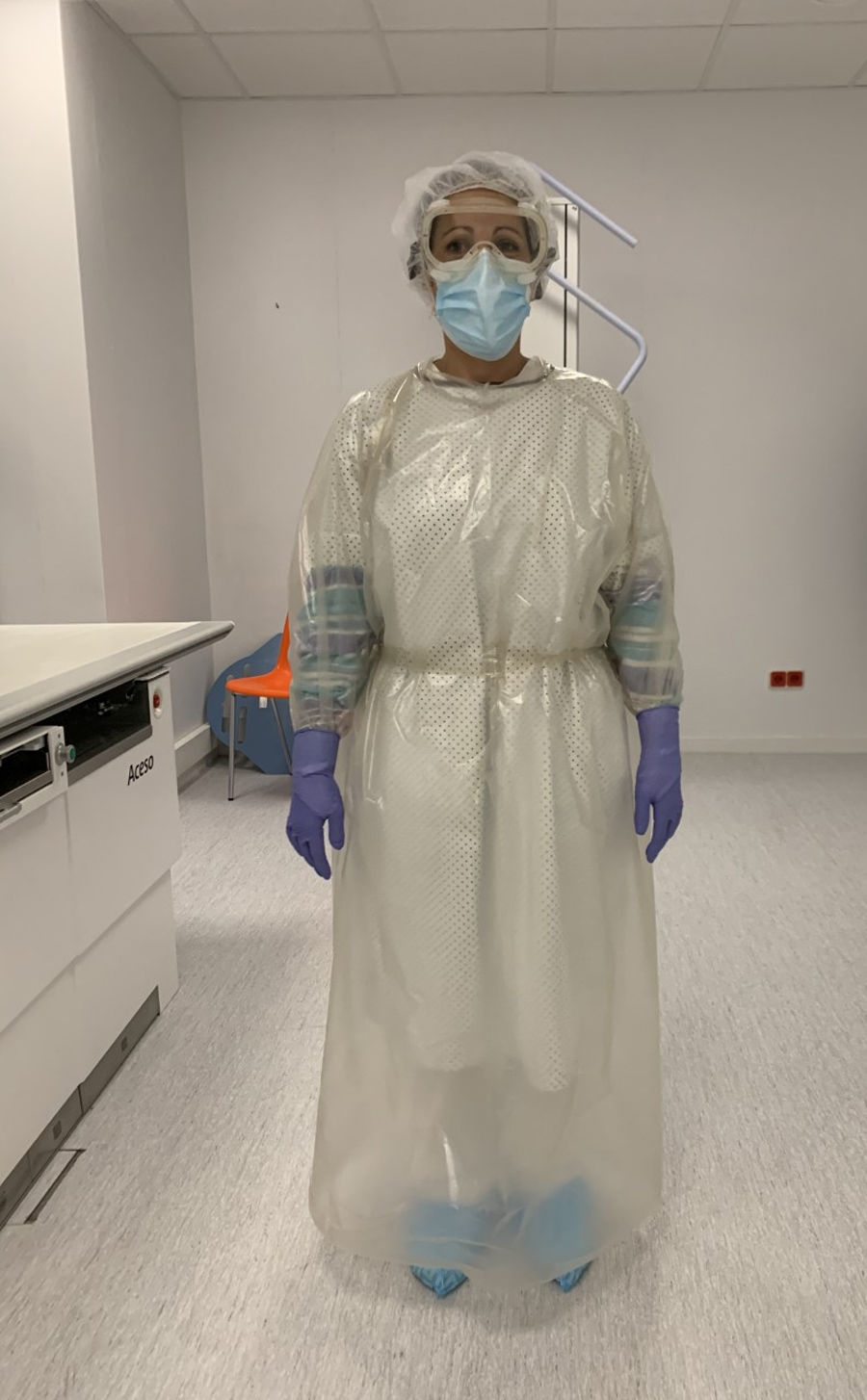
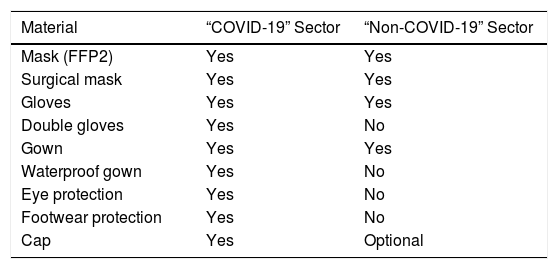
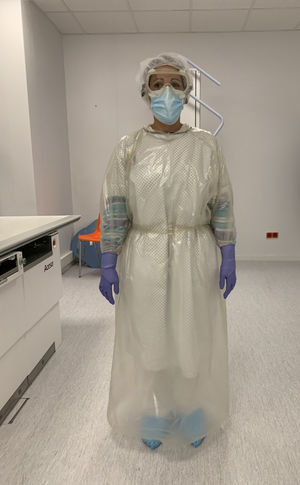
In the Diagnostic Imaging Department, protective protocols were implemented with the adaptation and provision of PPE (Fig. 1). These protocols were conveyed to and duly followed by staff members. In this way, standardisation of care practices among SDIT staff, regardless of their position or work shift, was achieved. Table 1 lists the PPE used by each healthcare circuit.
Personal protective equipment. Senior diagnostic imaging technician showing the protective equipment worn in the “COVID-19” sector. See Table 1.
Personal protective equipment used by SDIT staff by care activity sector.
| Material | “COVID-19” Sector | “Non-COVID-19” Sector |
|---|---|---|
| Mask (FFP2) | Yes | Yes |
| Surgical mask | Yes | Yes |
| Gloves | Yes | Yes |
| Double gloves | Yes | No |
| Gown | Yes | Yes |
| Waterproof gown | Yes | No |
| Eye protection | Yes | No |
| Footwear protection | Yes | No |
| Cap | Yes | Optional |
Spatial and temporal social distancing measures were also created to prevent staff contact, mainly during shift changes. Communication between the different work teams was carried out via institutional email. The rate of infections among SDIT staff in our department was 1.16% (1/86); this rate was considerably lower than that presented by the UDN and nursing assistant staff of the Emergency Department (27.6%; 31/112).
Healthcare action circuitsAt the height of healthcare activity during the pandemic, our hospital reached an overall capacity of 954 beds: 578 COVID-19 (60.5%) and 376 non−COVID-19 (39.5%). The intensive care unit (ICU) had 76 beds (65 COVID-19; 11 non−COVID-19) and 14 additional COVID-19 beds in the semi-critical area for patients with non-invasive ventilation.
As a result of the increase in specific demand and the resulting forced redistribution of the healthcare burden within the radiodiagnosis department, a reorganisation of technical resources and staff was needed. The prominent role of radiological tests in the diagnosis and follow-up of pneumonia3–5 required a change in structure and work dynamics in which support for the Emergency Department, ICU and different wards admitting COVID-19 patients was prioritised. This led to the cancellation of tests considered non-essential in times of crisis (such as population-based breast cancer screening). In addition, some diagnostic tests were performed less due to a decrease in certain pathologies during the pandemic (e.g. reduction in polytrauma due to the lockdown).
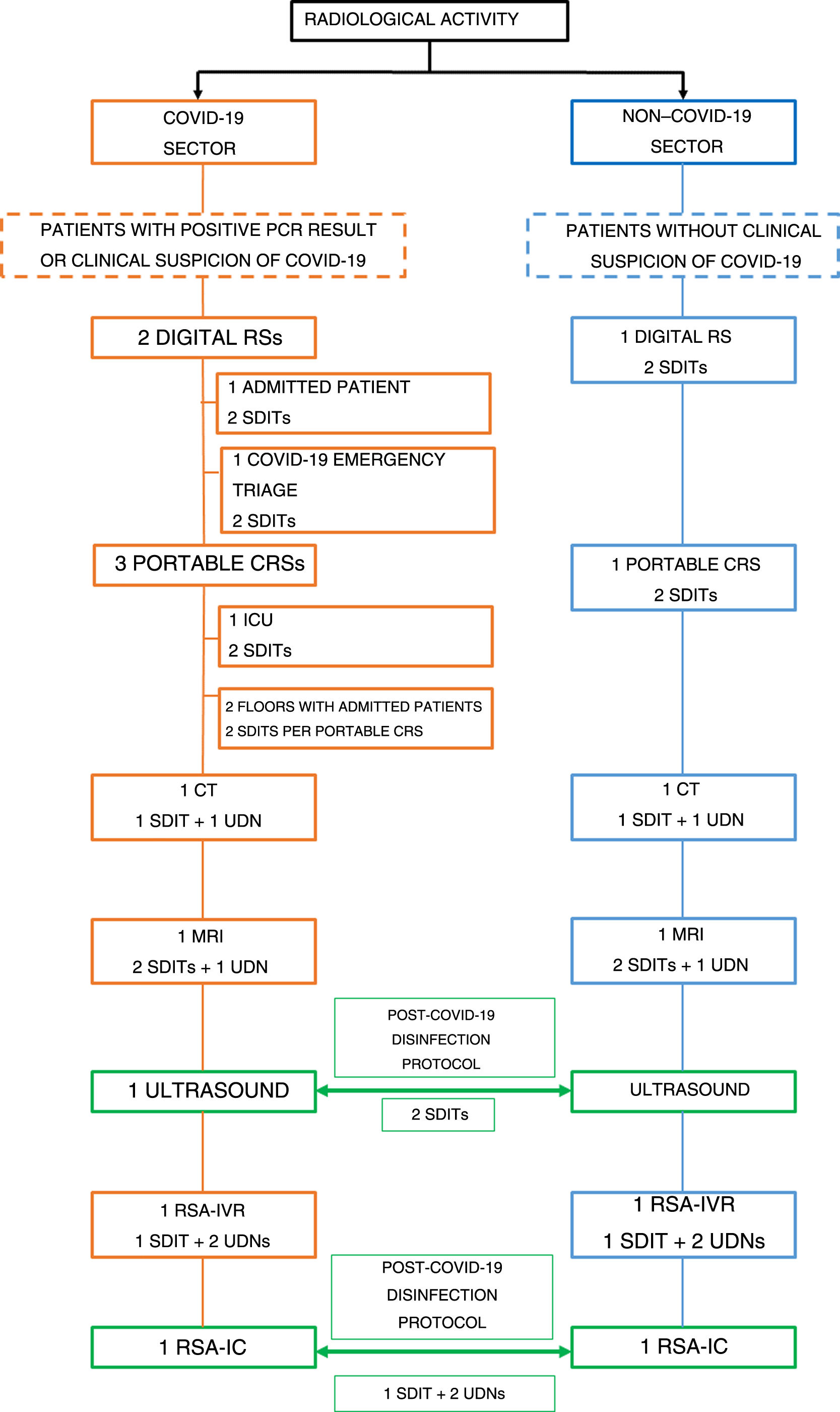
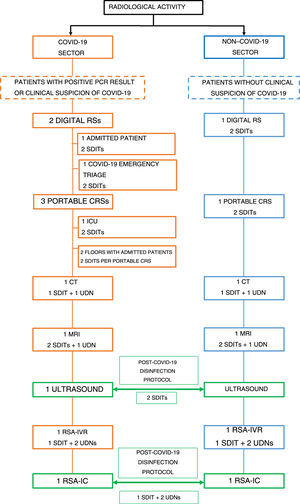
In line with other specialisations, our organisation and work dynamics were as follows: two sectors for radiological care activity were established. One was the “COVID-19” sector, where patients with a diagnosis confirmed by positive RT-PCR results, or with clinically suspected infection, received care. The other was the “Non−COVID-19” sector for patients without clinically suspected infection. The different imaging techniques were divided between these two sectors. COVID-19 activity was prioritised and all other essential healthcare activity was maintained. Both sectors had their own digital X-ray system, portable conventional X-ray system, CT scanner, magnetic resonance imaging system and C-arm for interventional vascular radiology. Due to low demand and our department's logistics, a decision was made to share the emergency ultrasound system and C-arc with the interventional cardiology department. This means that these two radiology techniques were used interchangeably by the two sectors, with adherence to a protocol for work room disinfection. Waiting rooms were closed at the height of the pandemic, but were subsequently partially reopened (with restricted capacity). As regards recovery rooms, these remained closed throughout the state of alarm. Fig. 2 shows a diagram of the technology and staff used during the COVID-19 pandemic.
Healthcare sectors. Diagram showing the different techniques and staff used in the different healthcare sectors (“COVID-19” and “Non−COVID-19”).
CRS: conventional radiology system; SCA-IC: surgical C-arm for interventional cardiology; SCA-IVR: surgical C-arm for interventional vascular radiology.
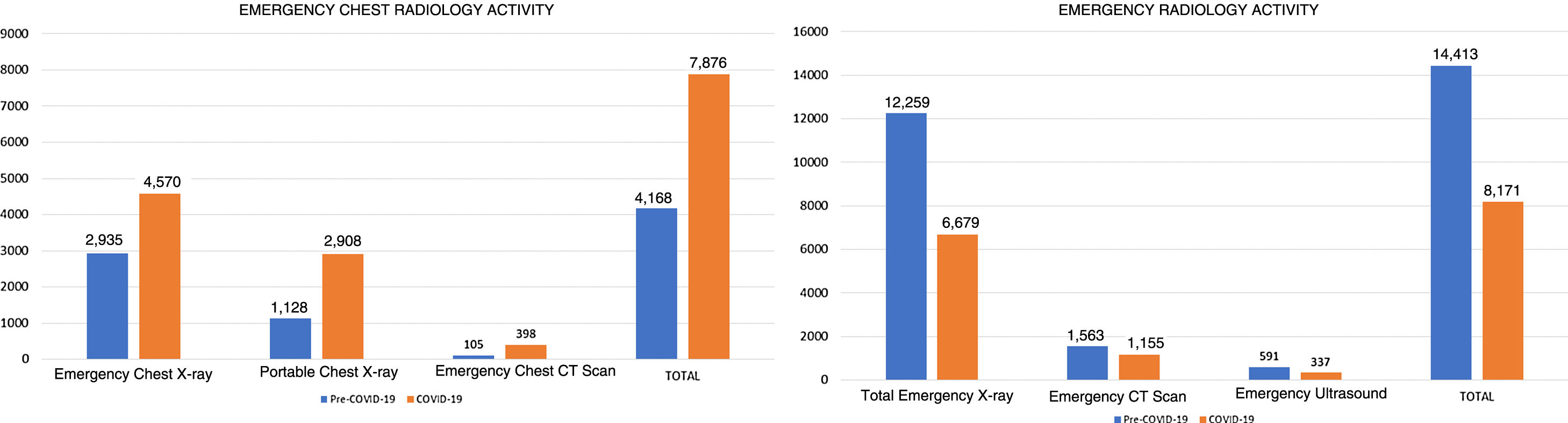
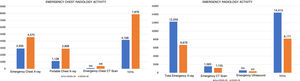
Analysis of the number of emergency examinations performed between March and April 2020 compared to the same period in 2019 reveals that there was an 88.9% increase in the activity of the Thoracic Radiology Area, secondary to a marked increase in X-rays and CT scans of the chest, though the total number of emergency radiological examinations decreased by 43.3%. Emergency radiological activity details are shown in Fig. 3.
In addition to performing diagnostic tests, SDIT staff played a leading role in the COVID-19 diagnosis circuit. With the implementation of teleworking as the main way of working, a protocol for action was established in which, in the event of a radiological finding raising suspicion of COVID-19 in a planned outpatient CT scan of the chest or abdomen (asymptomatic patients), the SDIT had to inform the radiologist responsible for the study by telephone to initiate the rapid COVID-19 diagnosis circuit through the Emergency Department. The SDIT also sent an e-mail to the UDN/SDIT Staff Management and Administration Directorate.
Shortcomings and obstaclesWe must not limit ourselves to describing only the strong points of the organisation of SDIT staff in times of crisis. It is also important, and indeed our duty, to describe the obstacles, errors and shortcomings that we faced during the pandemic.
Undoubtedly, a lack of experience with similar situations was, to our understanding, the most significant shortcoming. This generated a constant need to adapt to the different situations that arose day after day. Nobody was prepared to face such a situation, and the containment plans needed to cope with this new reality were not in place. The continuous improvisation led to a stressful work environment that affected all staff at all levels.
The sharp cuts made to the Spanish health budget as a result of the 2010–2012 economic crisis16 resulted in significantly outdated technology and a substantial lack of maintenance across all diagnostic imaging departments in Spain, representing another obstacle to be overcome. We were forced to cope with a significant increase in demand with old, frankly obsolete, equipment. Predictably, some equipment broke down. In our case, two portable conventional X-ray systems failed, representing a blow to our productivity at the time of greatest need.
The shortage of PPE was another shortcoming in the early stages of the pandemic. As a result, in some cases, we had to prolong PPE usage times or reuse certain materials (following sterilisation).
Among the public health measures put in place by governments during the COVID-19 pandemic, confinement proved to be the most important.17 Confinement saves lives. Of this there is no doubt. However, this unprecedented measure is not without consequences. On the contrary, many changes and new needs have surfaced in this scenario. In our department, it caused an increase in occupational leave related to lack of availability due to having to care for a child. Certain staff capable of working during the crisis were forced to take time off for such family responsibilities. In our case, it represented 8.1% (7/86) of the total TSID staff.
De-escalationThe de-escalation process carries several different challenges. The first consists of adapting to a "new normal", taking into account post-pandemic safety measures.18 The second consists of planning a new workflow to deal with the large numbers of pending examinations that were postponed during the pandemic. Finally, staff must be relocated to their usual work areas.
As an initial measure, in accordance with the protocols established by the health authorities, the capacity of the hospital centre was limited; companions were restricted and waiting rooms were restructured in order to maintain safe distancing. Planned examinations were also spaced out across all radiology settings. At the start of de-escalation, a 50% schedule was established, with capacity gradually increased as the weeks went by.
Regarding the scheduling of pending examinations, indications for performing, postponing or cancelling these was reassessed jointly with other specialisations.19
What about the future?Epidemiologists know that the current pandemic will not be the last and it is only a matter of time before the next one strikes.20
In order to function better in a crisis situation, all members of different care groups must receive more and better information. We believe it is essential to establish protocols for action in the event of a crisis and to incorporate them into each health worker's training. In addition, solid prevention programmes must be developed in the face of new crises and frameworks must be created to facilitate decision-making.
This pandemic has taught us that healthcare cuts are dangerous, and that equipping healthcare centres with the necessary staff and implementing suitable technological upgrades are matters of the utmost importance.
With regard to work dynamics, we are convinced that teleradiology will become even more widely used. With this in mind, new tools, skills and communication channels must be developed, especially for purposes of proper coordination between radiologists and SDITs.
We are aware of the limitations of this article. Our study reflects only the experience of a single diagnostic imaging department and the perspective of the authors. Future multicentre studies that incorporate and analyse survey data can improve understanding of how best to organise SDIT staff in the event of a pandemic.
ConclusionDiagnostic imaging departments, like all other areas of the health system, were affected by and forced to adapt to the crisis caused by COVID-19. We believe it is essential to recognise the role played by SDIT staff in the pandemic. This group, often not recognised by the system, have shown their professionalism and dedication in the fight against COVID-19. SDITs were one of the main frontline health workers, not only enduring gruelling working hours with changing guidelines, but also withstanding the stress and emotional pressure imposed by this critical situation. Furthermore, they had a proactive attitude as part of the rapid COVID-19 diagnosis circuit, thus contributing a significant added value to their healthcare role. Thanks to the measures implemented and the development of new work dynamics, we were able to face the obstacles and shortcomings presented by the system. Now, the most important task is to learn from this experience and prepare for the future.
AuthorshipResponsible for the integrity of the study: DR, JD, JP.
Study conception: DR.
Study design: JD, DR.
Data acquisition: DR, JD.
Data analysis and interpretation: DR, JD.
Statistical processing: N/A.
Literature search: DR, JD.
Drafting of the manuscript: JD, DR.
Critical review of the manuscript with intellectually significant contributions: DR, JD, JP.
Approval of the final version: DR, JD, JP.
Conflicts of interestThe sponsor and first author, as well as all other contributing authors, declare that there was no economic funding or any conflict of interest in the conduct of this study.
We would like to thank Dr Eva Castañer for making an invaluable contribution to the final manuscript and Dr Jaume Mesquida for providing relevant data. We would also like to extend our special thanks to all the staff of the Diagnostic Imaging Department at our institution for their professionalism, determination and commitment during the COVID-19 pandemic.
Please cite this article as: Ribas D, del Riego J, Perendreu J. Papel del personal técnico superior en imagen para el diagnóstico durante la pandemia COVID-19: importancia de la organización y planificación en la primera línea. Radiología. 2021;63:50–55.