Congenital anomalies of the central nervous system comprise a wide spectrum of malformations associated with a wide variety of genetic syndromes and chromosomal anomalies, and they are among the principal causes of morbidity and mortality in infants. Among these anomalies, holoprosencephaly arises from the complete or partial failure of the brain to divide into the cerebral hemispheres. Imaging tests are fundamental for the prenatal diagnosis of holoprosencephaly; the diagnostic process usually starts with sonography and then the findings are refined with fetal MRI. Radiologists need to be familiar with the possible findings because the prognosis varies.
Las anomalías congénitas del sistema nervioso central constituyen un amplio grupo de malformaciones asociadas a una gran variedad de síndromes genéticos y anomalías cromosómicas, y una de las principales causas de morbimortalidad infantil. Dentro de ellas, la holoprosencefalia conlleva un trastorno de la diferenciación del prosencéfalo, con una falta completa o parcial de división entre los hemisferios cerebrales. Para su diagnóstico prenatal es fundamental la realización de pruebas de imagen y el conocimiento de los posibles hallazgos, debido a que su pronóstico es variable, comenzando normalmente con la ecografía y confirmando lo visualizado con la resonancia magnética.
Abnormalities of the central nervous system (CNS) are, in general, a common group of congenital malformations, which can occur in one in 100 deliveries1, and are one of the main causes of infant morbidity and mortality. The prevalence varies between developed and non-developed countries, being lower in the former than in the latter, where figures are recorded from 10.6 to 167.0 per 1000 live births2,3.
They are associated with a wide variety of genetic syndromes and chromosomal abnormalities, and imaging is fundamental for diagnosis.
Case reportWe present the case of a 32-week pregnant woman diagnosed with holoprosencephaly on screening ultrasound (Fig. 1), with a positive genetic analysis for the c.2244_2245delAA variant (reported as pathogenic in the CSPP1 gene). Neither parent had any relevant previous medical history, except for consanguinity due to being first cousins. The mother was referred for foetal magnetic resonance imaging (MRI) for confirmation and anatomical assessment.
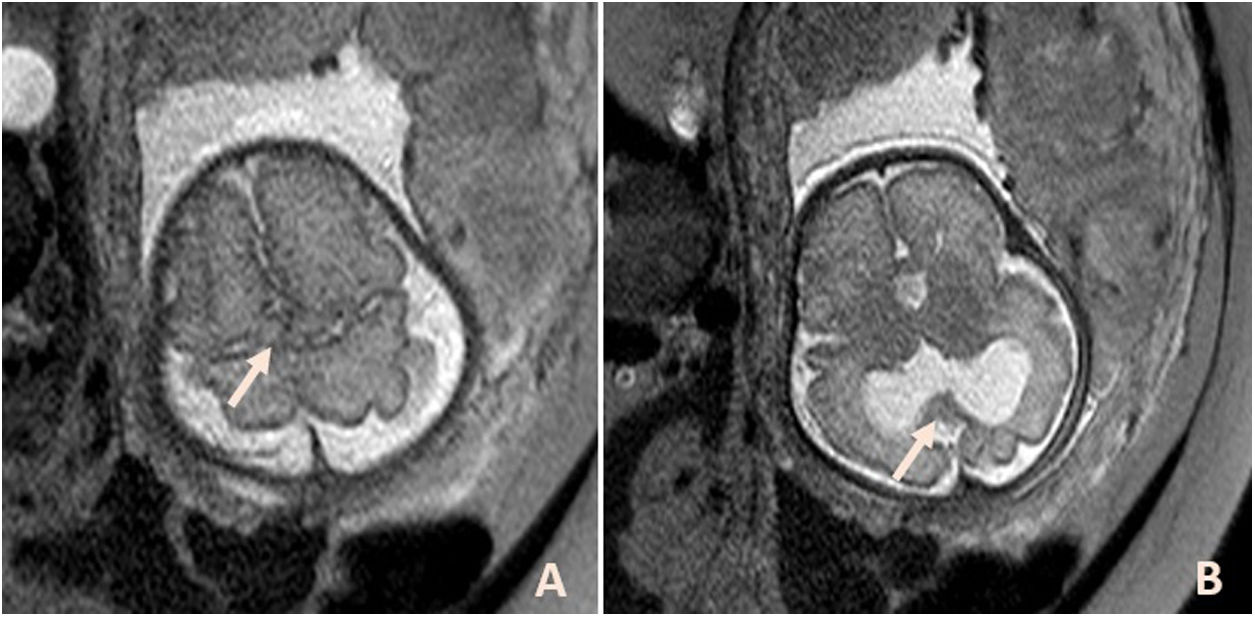
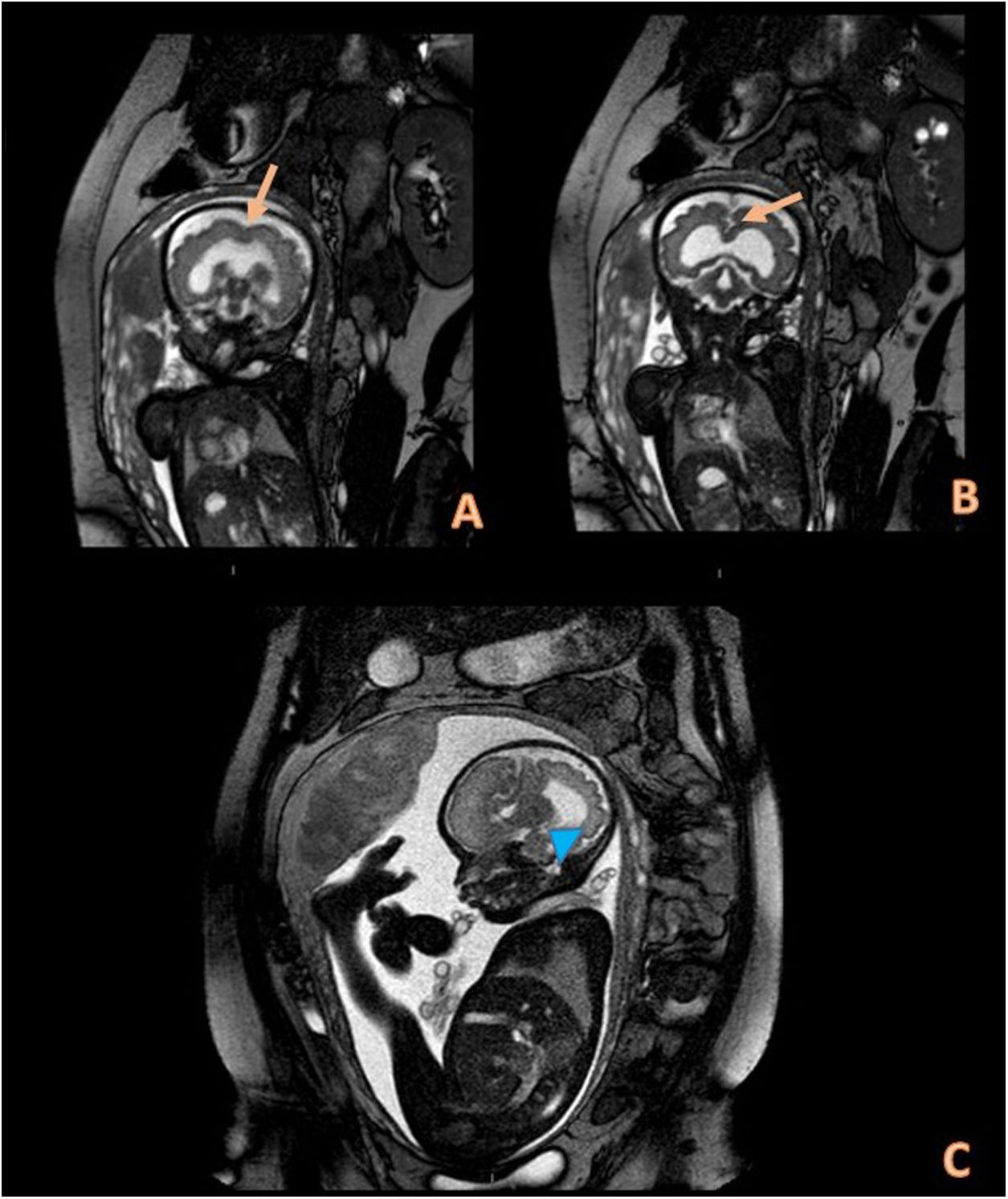
Foetal MRI confirmed the ultrasound findings. There was midline continuity of the posterior frontal and parietal cortex with fusion of the dorsal medial hemispheric cortex and normal separation of the frontal and occipital poles (Fig. 2A). This abnormality was associated with a single ventricular cavity (Figs. 3A and B), a single abnormal Sylvian fissure that covered the dorsal area of both hemispheres (Figs. 2B and 3 C) and absence of the cavum of the septum pellucidum, with dysgenesis of the corpus callosum (Fig. 2B). These abnormalities correspond to syntelencephaly (middle interhemispheric variant of holoprosencephaly).
The patient is currently continuing to have her pregnancy monitored until delivery.
DiscussionOf the different CNS malformations, holoprosencephaly is considered the most common. The prevalence is one per 250 pregnancies, less than one per 10,000 live births and stillbirths, and up to 50 per 10,000 in aborted embryos4. The aetiology is multifactorial, but the main causes are genetic and chromosomal abnormalities (classically trisomy 13, with 24–45% of cases of holoprosencephaly)5, teratogenic exposure and in association with syndromes. In this case, there was an abnormality in the CSPP1 gene, which is involved in the function of primary cilia, fundamental structures in the Sonic Hedgehog (SHH) signalling pathway, which in turn regulates part of the development of the forebrain-centralisation.
Holoprosencephaly is a diverticulation disorder that occurs in the differentiation process of the cerebral vesicles, specifically of the forebrain, with a complete or partial lack of division between the cerebral hemispheres.
It is classified into alobar, semilobar and lobar holoprosencephaly, in addition to the mid-interhemispheric variant (also known as syntelencephaly). These subtypes are briefly described below4.
Lobar holoprosencephaly is the mildest form, in which the falx cerebri and the interhemispheric fissure are absent in the rostral and ventral region of the frontal lobes, in association with dysplasia of the corpus callosum and absence of the septum pellucidum. In semilobar holoprosencephaly, the frontal lobes are united anteriorly due to the absence of the interhemispheric fissure and the falx cerebri, added to the absence of the septum pellucidum and the fact that the hippocampi are rudimentary. The most severe form is alobar holoprosencephaly, in which there is no division between the cerebral hemispheres, with a single ventricular cavity, absence of the corpus callosum and septum pellucidum, plus abnormal cerebral convolutions. Occasionally, a dorsal cyst is also observed, much more common (92%) in this subtype than in the others6.
Lastly, there is a variant known as the "middle interhemispheric variant" or syntelencephaly, which is what we have described in this case report. It consists of the absence of separation of the parietal and posterior frontal lobes. This is imaged as a fusion of the midline in the frontal posterior and parietal areas, while the polar areas of the brain are split normally. The corpus callosum may be absent, malformed or dysgenetic, the Sylvian fissures are vertically aligned and connect through the midline with the cerebral vertex. It has also been found that two thirds of these patients have cortical dysplasia or subcortical heterotopia7.
The facial malformations associated with these abnormalities are extensive, from cyclopia to ethmocephaly and cleft lip, all highly correlated with brain malformations. It should be noted that in syntelencephaly there are usually no midline craniofacial abnormalities, unlike in the other variants, in which they are more common.
The imaging test with which the study is usually started is the second-trimester ultrasound, which has a sensitivity of approximately 80%1. Because it is examiner-dependent and has other technical limitations, foetal MRI has been chosen as a supplementary test, as studies have shown it can detect abnormalities which are ultrasound-occult in up to 50% of cases8. Other studies have analysed the diagnosis of CNS abnormalities with both imaging tests. Although the series is small and should be interpreted with caution, the mean correlation between ultrasound and MRI findings in CNS malformations is 64%. MRI changed the diagnosis in 27% and provided additional data in 39%1.
As for the prognosis, holoprosencephaly is not as lethal as thought. Survival depends on the severity of a set of items: brain and facial malformations; the presence of chromosomal abnormalities; the involvement of other organs; and presence of multiple associated syndromes. Among euploid patients with holoprosencephaly, an inverse relationship has been found between the severity of the facial phenotype and survival4. Approximately 50% of children with the alobar holoprosencephaly subtype die within five months, but up to 30% live beyond a year. More than 50% of children with the semilobar or lobar subtype were alive at one year of age, and of those with lobar holoprosencephaly, about 50% can walk (some require assistance), have normal to mildly impaired hand function, and speak single words (some speak in multiple word sentences)9,10. Syntelencephaly is one of the variants with the best prognosis.
In conclusion, holoprosencephaly represents a wide variety of cerebral and facial malformations, most of them also associated with genetic disorders, with a variable prognosis depending on the subtype. It should be diagnosed prenatally by ultrasound and with a supplementary foetal MRI scan, as MR is less examiner-dependent and more conclusive in terms of assessing the findings.
Authorship- 1
Person responsible for the integrity of the study: IGM
- 2
Study concept: IGM and EMS
- 3
Study design: IGM and LFN
- 4
Data collection: EMS
- 5
Data analysis and interpretation: IGM and LFN
- 6
Statistical processing: LFN
- 7
Literature search: LFN
- 8
Drafting of the article: IGM
- 9
Critical review of the manuscript with intellectually significant contributions: EMS
- 10
Approval of the final version: IGM, LFN and EMS
The authors declare that they have no conflicts of interest.
Please cite this article as: Garrido Márquez I, Fernández Navarro L, Moya Sánchez E. Variante interhemisférica media de holoprosencefalia: diagnóstico medianteresonancia magnética fetal. Radiología. 2022;64:375–378.