Radiology is a medical discipline, an area of transversal knowledge integrated into any clinical situation. The optimal training of learning knowledge, skills and aptitudes in Radiology in the Degree in Medicine requires the integration of any imaging modality in the different areas of knowledge; from the basic subjects to any clinical subject of the Degree. This article describes the integration of Radiology teaching into the curriculum throughout the Medicine Degree at the University of Girona (UdG), describing the different radiology teaching activities that are taught. The specific activities of the subject "Radiology" are detailed; through workshops, seminars, practices, interactive computer game; and describing the characteristics of the main teaching methodological activity of the UdG, Problem-Based Learning.
La Radiología es una disciplina médica, área de conocimiento transversal integrada en cualquier situación clínica. La formación óptima del aprendizaje del conocimiento, habilidades y aptitudes en Radiología en el Grado en Medicina require la integración de cualquier modalidad de imagen en las distintas áreas del conocimiento; desde las asignaturas básicas hasta cualquier asignatura clínica del Grado. El presente artículo describe la integración de la docencia en Radiología del plan de estudios en todo el Grado de Medicina de la Universidad de Girona (UdG), describiendo las distintas actividades docentes de radiología que se imparten en las distintas asignaturas; desde primero a sexto curso. Se detallan las actividades específicas de la asignatura de "Radiología"; incluyendo talleres, seminarios, prácticas, juego de ordenador interactivo; y describiendo las características de la actividad metodológica docente principal de la UdG, el Aprendizaje Basado en Problemas.
Radiology training at undergraduate level varies widely between medical schools in Spain. Radiology has generally been a minor subject; this is reflected in the varied role it is assigned across different syllabuses particularly in the second half of the degree, according to the SERAM training commission report1 (although it should be noted that this report refers to the Spanish licenciatura syllabuses in place prior to the current Bologna-aligned undergraduate degree syllabuses). One of the objectives of the Bologna Process was precisely to standardise higher education throughout Europe.2 In this regard, the European Society of Radiology (ESR) produced a white paper in 20113 to serve as a baseline for radiology training curricula in medical schools across Europe, with the aim of addressing variations between different countries in undergraduate radiology education.4
The term ‘radiology’ includes all areas of knowledge related to medical imaging, diagnostic radiology, diagnostic imaging, radiotherapy, nuclear medicine and medical physics. The role of radiology, or medical imaging, in clinical practice has evolved in recent years to occupy an increasingly influential role in diagnostic and therapeutic decision-making. It is estimated that approximately 80% of medical decisions are made on the basis of radiological evidence.5 Today, radiology is a medical discipline in its own right, a cross-disciplinary area of knowledge that is integral to all types of clinical situations where it provides patient imaging data to facilitate the resolution of clinical problems.6 The great evolution seen in radiology as a specialty is yet to be reflected in many medical school syllabuses.7 On a positive note, according to a recent ESR publication, undergraduate radiology education has improved in the last decade.8
Undergraduate medical teaching began at the University of Girona (UdG) in 2008. The educational programme emphasises self-directed learning in the form of problem-based learning (PBL), considered essential to ensure students take an active, autonomous and committed approach to their own learning. All subjects had to include the main teaching method, PBL, in their syllabus. The PBL methodology has been integrated as a common objective at all levels of radiology teaching across the different areas of knowledge,9 from core subjects such as anatomy to the different areas of clinical teaching delivered over the six-year undergraduate degree,10 with a particular emphasis on the radiology-specific module in the second year. The aim is that students in the medical undergraduate degree gain a solid grounding in radiology knowledge, skills and aptitudes11 by integrating the different imaging modalities into the different areas of medical knowledge.5 This article describes the way radiology teaching has been integrated into the UdG medical undergraduate degree programme syllabus. The article is divided into two sections: the first describes the integration of radiology into the different modules throughout the degree, and the second specifically describes the way the radiology module is taught in the second year of the degree.
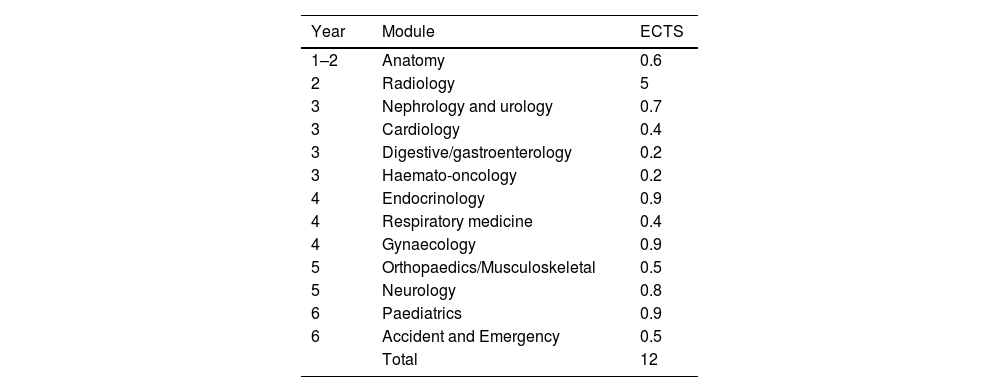
Integrating radiology into the UdG degree in medicineRadiology forms part of the area of knowledge relating to medical imaging, generically called ‘radiology’ in the UdG degree in medicine. It includes diagnostic radiology, nuclear medicine, radiotherapy and medical physics. The subject area ‘radiology’ makes up 12 (3.4%) of the 355 total ECTS (European Credit Transfer System) credits in the medical degree at UdG.
Table 1 illustrates how radiology ECTS credits are distributed across different modules of the degree course. Of these, the highest number of credits (5 ECTS) is awarded to the Radiology module. This is a second-year subject and is described in detail in the following section. The distribution of radiology credits throughout the degree given in Table 1 does not include the credits for the final dissertation project, which radiologists may supervise each year, should students choose a radiology-related issue to investigate. Our baseline credit distribution also does not include the two optional modules offered to students: ‘Anatomical recognition by ultrasound: musculoskeletal and locomotor system’, and ‘How medical imaging is improving modern medicine’.
Distribution of credits for the knowledge area of medical imaging, radiology, in the undergraduate degree in medicine at the University of Girona.
| Year | Module | ECTS |
|---|---|---|
| 1–2 | Anatomy | 0.6 |
| 2 | Radiology | 5 |
| 3 | Nephrology and urology | 0.7 |
| 3 | Cardiology | 0.4 |
| 3 | Digestive/gastroenterology | 0.2 |
| 3 | Haemato-oncology | 0.2 |
| 4 | Endocrinology | 0.9 |
| 4 | Respiratory medicine | 0.4 |
| 4 | Gynaecology | 0.9 |
| 5 | Orthopaedics/Musculoskeletal | 0.5 |
| 5 | Neurology | 0.8 |
| 6 | Paediatrics | 0.9 |
| 6 | Accident and Emergency | 0.5 |
| Total | 12 |
ECTS: European Credit Transfer System.
Radiology is first integrated into the degree in medicine in the first- and second-year anatomy modules through interactive workshops, which include a brief introduction to radiology imaging techniques, and anatomical recognition in the following imaging modalities: plain radiology, CT and MRI. These seminars are held in the computer room so that the images can be viewed directly using a DICOM viewer in groups of 20 students.
The radiology-specific module is taught in the second year of the degree. The aim of this subject in the second year is to cover the basics of radiological techniques, nuclear medicine, radiobiology and radiation protection. The following section will describe the teaching in the second-year radiology module.
In years three to six of the degree, radiology is integrated within different clinical modules (Table 1), as previously described. These modules cover all the radiological pathology training on the curriculum, which is taught by radiologists in each of the clinical subjects. In each clinical module, teaching is carried out through workshops or seminars in small or medium-sized groups, i.e. between 20 and 40 students, to facilitate interaction. Radiology teaching across the different clinical modules aims to integrate knowledge, skills and aptitude in interpreting radiological pathology and connecting it to clinical pathology, as well as discerning when to use different imaging techniques in each of the areas of medical knowledge covered by the degree.
It should be noted that, besides the optional radiology credits for the final year dissertation and optional modules, as previously described, the objective structured clinical examination (OSCE) at the end of the degree also includes a specific section to assess competence in radiology. Radiology lecturers who teach the different seminars/workshops within each clinical module provide exam questions to the module coordinator for the corresponding assessments.
At present, there are a total of ten radiologists teaching radiology throughout the UdG degree programme, not including a nuclear medicine doctor, a medical physicist and a radiation oncologist.
Radiology-specific teaching activitiesThe Radiology module in the second year of the degree consists of different teaching activities, the main one being PBL sessions. PBL is self-directed learning, in which the student takes an active and autonomous role in their own learning. The other activities include: workshops, seminars, masterclasses, hospital placements and interactive games (Medgame).
The subject covers these general learning objectives:
- •
Fundamentals of radiology, radiation sources, imaging techniques and treatments/therapies. Radiobiology, radiation protection.
- •
Indications, contraindications of imaging techniques; contrasts, radioisotopes for imaging tests.
- •
Basic imaging/report interpretation and basic imaging features.
Each general objective contains specific objectives, which the student must achieve by the end of the course. For example, the specific objectives within the wider learning objective (LO), ‘Radiation interaction mechanisms when forming images’, are:
- 1
Explain conventional diagnostic radiology techniques: analogue versus digital.
- 2
Understand the concept of spatial and contrast resolution.
- 3
Define techniques specific to conventional diagnostic radiology: contrast, dental radiography, mammography, fluoroscopy, digital angiography, PACS.
- 4
Explain computed tomography: characteristics of the equipment and data collection.
- 5
Explain ultrasound: transducers, artifacts, Doppler effect.
- 6
Explain MRI: image acquisition mechanism. Sequences, antennas.
- 7
Describe the instrumentation used in nuclear medicine.
- 8
Be familiar with gamma camera planar imaging and tomographic equipment.
- 9
Define scintigraphy and its modalities.
- 10
Explain densitometry.
PBL is the main teaching methodology applied throughout this module. It consists of self-directed learning, in which the student takes an active and autonomous role in their own learning.12 The PBL methodology presents students with real clinical situations as problem scenarios. The student must use reasoning strategies to formulate hypotheses based on the data, as well as identify learning needs, propose and identify concepts to solve, prove or demonstrate the problem.13 The process of selecting the correct sources and their critical evaluation helps students to gain a deeper understanding of the problem by discussing, exchanging ideas and reflecting on how to resolve the scenario.14 The purpose of the activity lies primarily in identifying which learning needs must be met to achieve the learning objectives (LOs), rather than solving the problem itself.15
Three sessions are dedicated to each problem (PBL tutorials), with a tutor and a small group of students (maximum 10). The tutor's interventions are student-centred and their role is to facilitate student learning.16 PBL consists of three essential elements: learning objectives (LOs), problem scenarios and assessments (continuous assessment and PBL exam).
PBL sessions are set up in the same way for each of the three problem scenarios in the module:17 the group meets three times with the tutor for approximately two hours each time, on different days and, if possible, with a day off between each (Monday, Wednesday and Friday). To resolve the problem scenario, they follow these steps:
First dayPresent and analyse the problem.
- •
Brainstorming: possible explanations or hypotheses for the problem identified within the group (Fig. 1).
- •
List existing information/knowledge that might be relevant when analysing the problem.
- •
List points of interest related to the problem (what students do not know, do not understand or consider important or relevant).
- •
List what they need to know (learning needs) to understand/solve the problem. The tutor proposes an order of priority for the learning needs according to their relevance for the LOs.
- •
List tasks necessary to achieve the LOs. How to obtain the information (library, internet, consultation with teaching staff and experts…): PubMed, Google… But students are not given a list of books or a bibliography: they must perform their own search.
- •
The first session ends when the LOs have been set and a work/study/learning plan (which the whole group has agreed to) has been set out (Fig. 2). The tutor will help to clarify the LOs and how to achieve them. The members of the group choose what subjects they want to focus on. It is recommended the group identify and choose one or a maximum of two subjects of general interest or of key importance for all members of the group to work on. Other subjects can be investigated individually or in small groups. Students are always asked if they want to work on other LOs that have not been included in the work plan either individually or as a group.
Each student should contribute the following in relation to the LO they have worked on:
- •
A summary of the information found. This should not take the form of individual ‘presentations’. It should be a brief (5 min) explanation to present the key points from the information found. At the end of each explanation the tutor will ask: ‘Does anyone have anything relevant to add?’.
- •
The source of the information: what was the most effective source of information, what level of evidence does the information provide (is it an opinion piece, a meta-analysis, original research…); review articles are very helpful if up-to-date.
- •
The difficulties faced when searching for information. For example, difficulties in accessing sources.
- •
The group will critically evaluate the information collected. For example, reputation of the authors, search and statistical methods employed.
- •
Assess the work plan hypotheses and then reconstruct and interpret the acquired knowledge.
- •
Reevaluate the problem in light of the acquired knowledge. It is worth rereading the scenario with the newly acquired information, to see if any LOs were missed before, if any hypotheses should be changed, etc. Review the learning plan after reevaluating the problem.
- •
At the end of the day, students leave with the LOs for the problem scenario to serve as a guide for redesigning the learning plan and for students to prepare any remaining learning needs for the third day.
- •
The tutor/facilitator has a key role in the student’s learning and in the subsequent assessment of their competencies. The tutor should facilitate and incentivise participation of all students throughout the learning process. Limiting PBL groups to a maximum of 10 students allows for improved individual participation in PBL sessions. Larger groups complicate individual participation.
Coming to an agreement: all collated information is discussed and compared.
- •
Identify disagreements and differences of opinion.
- •
Develop final hypotheses that would explain the problem scenario and read the final conclusions sheet (this is not essential, the learning objectives are key here).
- •
Identify relevant principles and concepts from the knowledge acquired that can be applied to other problems/situations.
- •
Perform post-analysis reflection (students answer the following for themselves):
- -
What new topics, principles and concepts have we worked on and discussed?
- -
How can we link what we have learned is linked to the LOs? From what we have learned, what will help us in terms of understanding different problems in the future (analogies)?
- -
What LOs have been identified but not explored? Will these remain as personal learning objectives? If any essential LOs have not been worked on, these should become additional objectives to achieve.
- -
Three clinical scenarios are tackled in PBL sessions. These three scenarios have been developed and drafted to include the learning objectives the student should achieve. The scenarios are chosen because they present characteristics and context of the problem incorporate the relevant LOs.18 The three problem scenarios incorporate the following learning objectives: the foundations of radiology, sources of radiation, imaging or therapeutic techniques; radiobiology, radiation protection. The first scenario deals with radiation and radiation protection, the second nuclear medicine and CT techniques and the third scenario focuses on ultrasound and magnetic resonance. The remaining LOs for the subject are acquired through the other activities, which will be described in the following subsections. The LOs covered by the remaining teaching activities are: indications and contraindications of imaging techniques; contrasts and radioisotopes in imaging tests; basic interpretation of images/reports and basic imaging features.
The PBL methodology enables students to learn from real-life clinical scenarios, integrating and promoting skills development, positive attitudes to participation, critical analysis and resource finding skills. It promotes comprehensive learning and the building of integrated medical knowledge in a stimulating way.15
Workshops/seminarsThree practical workshop sessions are held in the IT suite to learn to read radiological images systematically. Chest, abdomen and spine radiographs are analysed, as well as images originating from CT, MRI and nuclear medicine techniques. The course also includes learning to interpret standard reports for the most common imaging tests, learning the most common radiological terminology and specifically discussing the contraindications of tests that use ionising radiation, MRI, iodised contrasts and gadolinium contrast.
A set of images are made available on the module’s web platform (Moodle environment), alongside typical questions about the images and a list of standard reports, for students to analyse prior to the workshop. On the day of the workshop, the questions on the different images are answered interactively with the participation of all students. The workshops are held in groups of 20 students.
MasterclassesMasterclasses are stimulating sessions based on areas of conceptual complexity from a number of sources, including drawing on the specific expertise of teaching staff. The masterclasses taught are: radiation and radiation protection, CT, MRI, ultrasound, interventional radiology, radiotherapy and nuclear medicine.
Hospital placementsA one-day clinical placement is carried out in the hospital’s radiology department, with students divided into groups of two or three so they rotate through all the department’s rooms. The objective is to gain practical knowledge of how each technique works, and how a radiology department operates. Students see the request for an imaging test, then observe the methodology used to carry out the test and finally, in the report room, the procedure for analysing and writing a radiological report. Students will also have the opportunity to observe interventional procedures during the visit. In addition, the department offers voluntary clinical placements during the summer period.
Interactive game - MedgameIn 2012, the Research and Education Foundation of the Radiological Society of North America (RSNA) awarded a grant to ‘Developing a computer game for problem-based learning (PBL) of radiology for undergraduate medical education (MEDGAME)’.19 The grant enabled the funding and development of an educational computer game to help medical students learn the contraindication criteria of radiological methods and the basic principles of their interpretation. The game was designed to simulate a real radiology department in 3D. Students are presented with four realistic challenges in this scenario (Fig. 3) showing patients who present with real-life clinical situations in which the student takes on the role of an accident and emergency physician who interacts dynamically with a radiologist exchanging questions and answers. The four challenges are based on questions relating to the following four imaging modalities: plain radiology, ultrasound, CT and MRI (Fig. 4). The student answers the questions and is told whether the answers are correct or incorrect (with explanations for any errors). They are awarded a score at the end of the test. The Medgame session takes place in the IT suite in groups of 20 students (Fig. 5).
One of the key steps in any learning process is student assessment. The PBL system is based on evaluating a student’s appropriate use of the method and then the level to which they have acquired the desired knowledge.
The evaluation consists of three parts: continuous assessment throughout the PBL sessions (40% of the final mark), PBL exam (30% of the mark) and practical exam (30% of the mark).
Continuous assessment throughout PBL sessions evaluates the following skills: learning, communication, sense of responsibility and interpersonal relationships. In this way the assessment goes beyond simply evaluating knowledge acquisition to also consider skills, attitudes and professional values (teamwork, continuous learning, communication, commitment, responsibility).
The PBL exam is comprised of two parts. The first part is based on a clinical problem. Students must create a hypothesis for the scenario, define the objectives and justify them correctly, demonstrating understanding of basic concepts in the areas of medical physics, diagnostic radiology, nuclear medicine and radiotherapy that underlie the scenario. Students should solve the problem following the same process as in the tutorial sessions, but individually. The second part of the PBL exam consists of short questions on relevant theories, concepts and that pertain to the subject’s learning objectives.
The practical exam includes short questions linked to images/reports on the different techniques to assess the student’s skills at interpretating any of the procedures studied during the practical workshops and in Medgame.
The PBL methodology was implemented 14 years ago as part of the new degree in medicine at the University of Girona in 2008. Over this time the results have shown it to be effective and student surveys reveal high levels of satisfaction. Examination results demonstrate high levels of competence, in accordance with the previously defined learning objectives.10 Existing studies that compare the PBL methodology with conventional teaching demonstrate that PBL is coupled with improvements in students’ learning, problem-solving skills and learner satisfaction.20
ConclusionRadiology is a cross-disciplinary medical discipline integral to all types of clinical situations. To gain the appropriate knowledge, skills and aptitudes in radiology, undergraduate medical training should integrate the relevant imaging modalities into different areas of medical knowledge. Radiology training should be integrated into all modules on the curriculum, from core subjects to any clinical subject throughout the whole degree for students to gain a good level of competence, in accordance with their learning objectives. This integration requires teaching activities be carried out in different subjects of the degree, using problem-based learning as the central underlying methodology.
FundingThis article has not been funded.
Author contributions- 1
Research coordinators: J.C.V.
- 2
Development of study concept: J.C.V.
- 3
Study design: J.C.V.
- 4
Data collection:
- 5
Data analysis and interpretation:
- 6
Statistical analysis:
- 7
Literature search: J.C.V.
- 8
Writing of article: J.C.V.
- 9
Critical review of the manuscript with intellectually relevant contributions: J.C.V.
- 10
Approval of the final version: J.C.V.
There is no conflict of interests.