Suplement “"Advances in Thoracic Radiology”
More infoWe present an uncommon case of a solitary fibrous tumor of the pleura with the appearance of an air-containing cystic mass. We discuss the differential diagnosis through the imaging findings, the hypothetical origins of the air component, and the possible relationship between the air component and the aggressivity of the tumor.
Presentamos un caso inusual de tumor fibroso pleural solitario con componente quístico aéreo. Se discute el diagnóstico diferencial a través de la imagen radiológica, así como la hipótesis de origen del componente aéreo y si existe relación entre este y la agresividad del tumor.
Solitary fibrous tumors of the pleura (SFTP) are a rare entity, accounting for less than 5% of all pleural tumors; fewer than 1000 cases have been published in the literature.1–3 It is even rarer for imaging to reveal air inside, and this has only been described in a few cases.2–6 We present a single case of a cystic SFTP containing air.
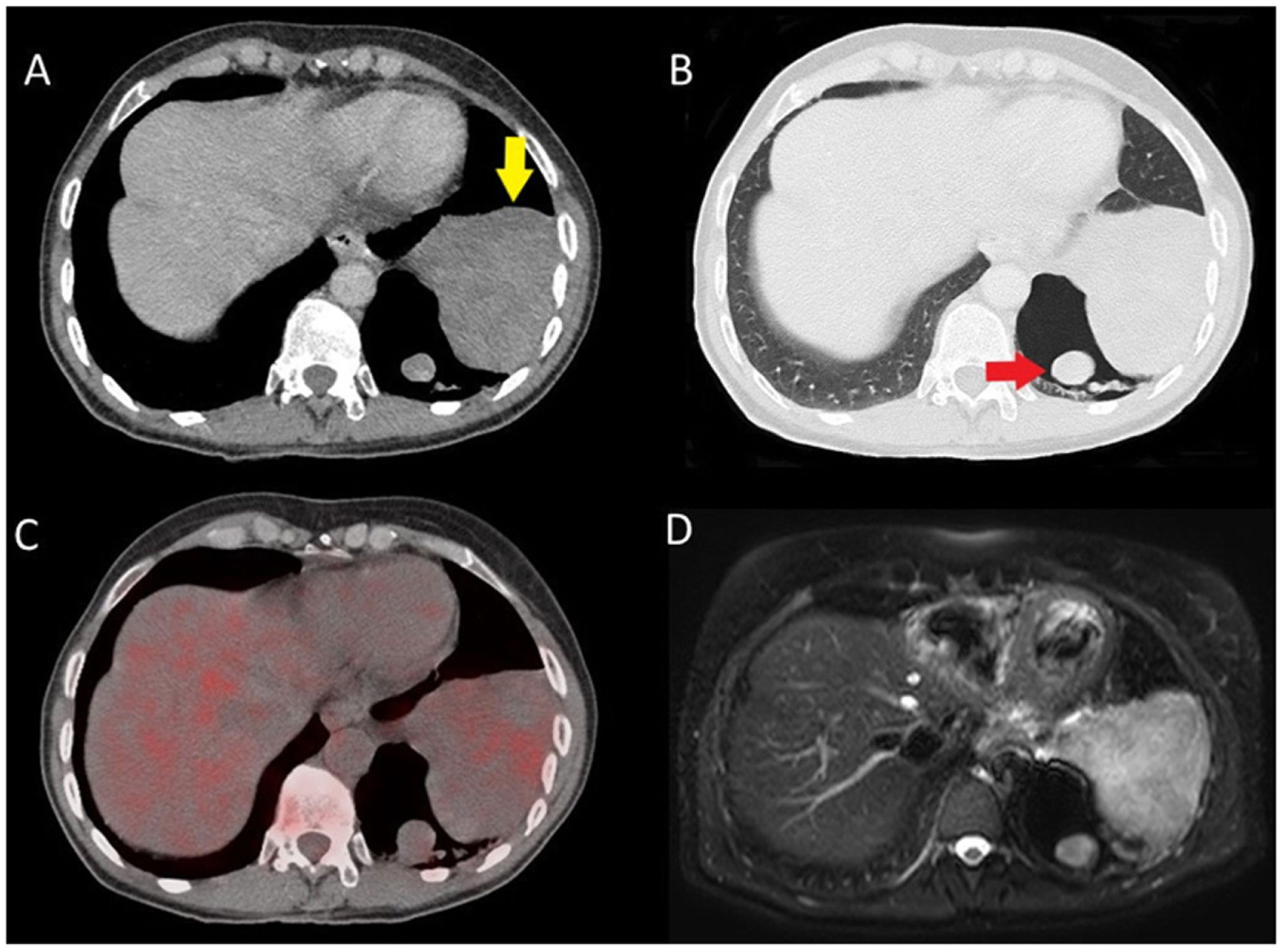
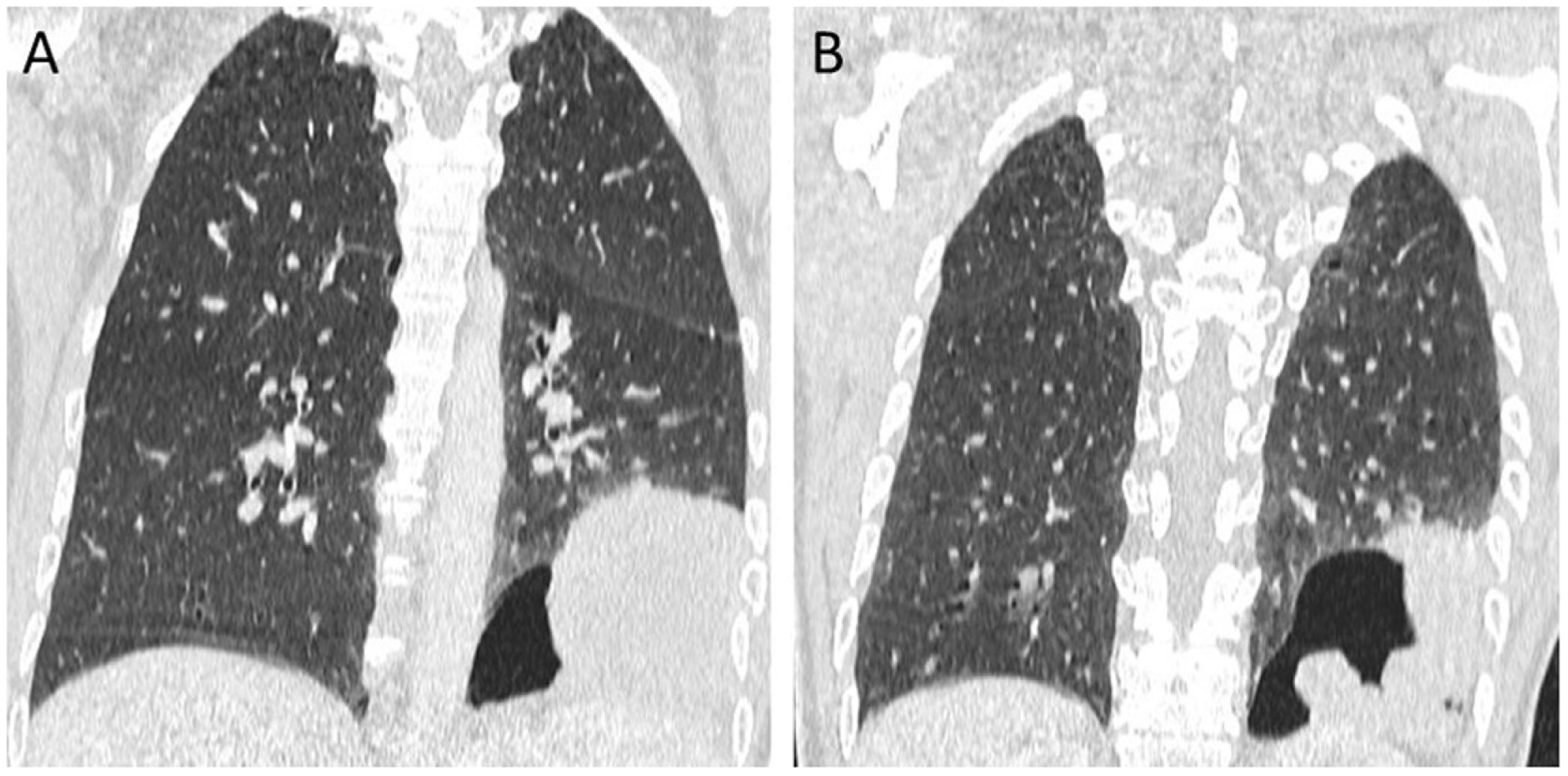
Case presentationA 57-year-old woman with no relevant medical history presented to the Emergency Department with subocclusive symptoms for which a computed tomography (CT) scan of the abdomen was performed. The slices corresponding to the lung bases revealed the incidental finding of a left intrathoracic mass which led to the decision to complement the study with a CT scan of the chest with intravenous contrast. The test showed a pleural lesion in the base with well-defined margins, homogeneous contrast uptake and an air-filled cavity with solid mural nodules inside (Figs. 1A and B, 2A and B). No previous studies were available, so it was initially suggested to be a congenital pulmonary airway malformation (CPAM) due to its air component. A PET-CT scan was also performed and showed mild, non-significant metabolic activity in the solid component (Fig. 1C). The imaging study was completed with an MRI that showed an isointense signal in T1-weighted sequences and hyperintense in T2-weighted sequences in the solid part, with no signs of invasion into the chest wall or diaphragm (Fig. 1D).
Chest CT axial slices of the lung bases with soft tissue window (A) and lung window (B) showing a left basal pleural lesion (yellow arrow) with an adjacent air cavity containing solid mural nodules (red arrow). C) Axial PET-CT slice at the same level as the CT images demonstrating non-significant metabolic activity in the solid part of the lesion, similar to that of the liver parenchyma. (D) Axial MRI slice of a fat-suppressed T2-weighted sequence at a similar level to the previous ones, showing moderate signal hyperintensity in the lesion under study.
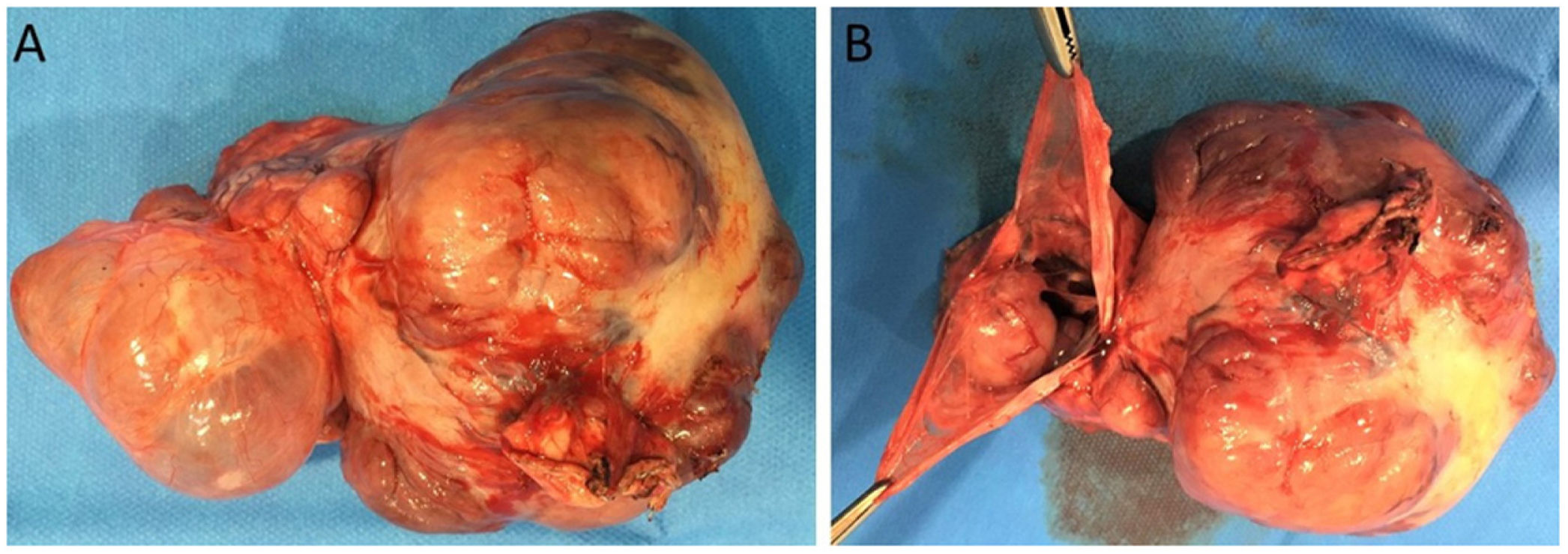
Subsequently, a CT-guided core needle biopsy was performed, yielding cells compatible with an SFTP, which led to the decision to perform surgery. During the operation, a pedunculated lesion in the visceral pleura was found and an atypical resection of the left lower lobe was performed with wide margins. Gross examination of the specimen revealed a large polylobulated pleural lesion, yellowish-brown in colour, with an air-containing cystic portion that had tumor nodules inside (Fig. 3A and B). Histological examination revealed the presence of spindle cells with scant cytoplasm, positive staining for CD34 and STAT6, and negative staining for cytokeratins, confirming the diagnosis of SFTP. There were no signs of malignancy, such as necrosis, pleomorphism or high mitotic count. The patient was discharged 48 h after surgery and 12 months later is disease-free.
DiscussionSFTP is a rare neoplasm of mesenchymal origin that typically originates in the visceral pleura and appears on CT as a well-defined, solid soft-tissue mass.1,2,7 SFTP containing air are very rarely seen on imaging and there are only a few reports in the literature.2–6 It appears as a thin-walled air cavity containing the entire tumor, either as single or multiple solid nodules, and radiologically resembles the appearance of a CPAM or even an aspergilloma.2–4 There are also cases where it presents as an air-containing cystic lesion adjacent to the solid part of the neoplasm, creating a gap between the tumor and the air component.2,5,6 In our case it was a combination of the above, in the form of a homogeneous pleural mass with an adjacent large air-containing cyst, which contained several solid nodules inside.
The origin of the air component is not fully known. The most plausible hypothesis is that peripheral lung tissue is trapped during tumor growth, causing air to accumulate inside the tumor due to a valvular mechanism. This mechanism allows air to enter, but not to exit, due to the compressive effect of the mass on the bronchioles. This hypothesis was proposed by Baek et al.5 and Kanai et al.6 A second hypothesis suggests the possibility that the mass grows on top of a pre-existing bulla,4 and a third possible aetiological cause is that alterations in genetic sequencing lead to the cystic degeneration and air component of the tumor.3
Most SFTP are benign, with malignant or potentially malignant cases accounting for 10–15%.2 It is difficult to predict malignancy of SFTP by CT, although certain features have been associated with a higher possibility: larger size, heterogeneous density, the presence of abundant vascularity, or pleural effusion.2 Histological features such as high cellularity, the presence of abundant mitoses or cellular pleomorphism often imply a greater tendency for recurrence or metastasis.1,2 In the case presented, as in previously published cases of air-containing SFTP,3–6 the presence of intratumoral air did not imply that the tumor was more aggressive, and no complications or recurrences have been described in these cases.
In conclusion, the radiological diagnosis of a SFTP should not be ruled out when an air-containing pleural mass is detected, and a differential diagnosis should be made with CPAM or even aspergilloma.
FundingThis research has not received funding support from public sector agencies, the business sector or any non-profit organisations.
Author contributions- 1
Research coordinators:
- 2
Study concept: ARA.
- 3
Study design: ARA.
- 4
Data collection: ARA, CMRG and NCA.
- 5
Data analysis and interpretation: ARA, CMRG and NCA.
- 6
Data processing:
- 7
Literature search: ARA and CMRG.
- 8
Writing of article: ARA.
- 9
Critical review of the manuscript with intellectually relevant contributions: CMRG and NCA.
- 10
Approval of the final version: CMRG and NCA.
The authors declare that they have no conflicts of interest.