Suplement “Update and good practice in the contrast media uses”
More infoIn diagnostic imaging departments, there has been a technological evolution in recent years. Progress made in interventional processes and the development of new treatments, as well as an increase in the number of diagnostic and therapeutic tests, has generated a growing and exponential need for specific care. Furthermore, the people who come to these departments are often in a vulnerable state and out of their comfort zone.
The implementation of advanced practice nursing (APN) in the context of metabolic therapies and diagnostic imaging provides expert care with a holistic approach to patient care. It uses the nursing care process as a working method which, through research, logical analysis and critical reasoning, enables nursing care to be developed and applied. This approach contributes to safety management in the different processes in which it is engaged.
The aim of this article is to highlight the interventions in which nursing practice can contribute to contrast media safety management in a diagnostic imaging department.
En los departamentos de diagnóstico por la imagen, ha habido en los últimos años una evolución tecnológica. El avance de los procesos intervencionistas y el desarrollo de nuevas terapias, así como el incremento en el número de pruebas diagnósticas y terapéuticas, ha generado una creciente y exponencial necesidad de cuidados específicos. Además, las personas que acuden estos departamentos suelen encontrarse en un estado vulnerable y fuera de su zona de confort.
El desarrollo de la enfermería de práctica avanzada (EPA) en terapias metabólicas y en diagnóstico por imagen, brinda en estas Unidades una atención experta con un enfoque integral en el cuidado del paciente. Utiliza el proceso de atención enfermera como método de trabajo, que, a través de la investigación, el análisis lógico y el razonamiento crítico, permite desarrollar y aplicar los cuidados enfermeros. Mediante este enfoque, contribuye a la gestión de la seguridad en los diferentes procesos en los que participa.
El objetivo de este artículo es dar a conocer las intervenciones que puede ofrecer una consulta de enfermería en la gestión de la seguridad de los medios de contraste en un departamento de diagnóstico por imagen.
The rapid technological evolution in Diagnostic Imaging departments and the complexity of healthcare processes today has created the need for a comprehensive and more personalised approach to the care provided. Advanced practice nursing (APN) emerged in the United States in the 1970s,1 as the figure of the Advanced Practice Registered Nurse. It was later (1990s) introduced in Canada, with Nurse Practitioners in a context of master's or doctoral training. Since then, the role has been further developed in other countries, such as the United Kingdom (advanced nurse practitioners - ANP), Australia, New Zealand, The Netherlands, Sweden and Ireland.2
Sheer et al. confirm that the development of advanced practice in nursing is a global trend3 and, although there is no single definition, there is consensus that it involves highly autonomous practice, employs the maximum use of nursing knowledge and contributes to the advancement of the profession.4
The ANP differs from the general care nurse in that they have a high degree of clinical autonomy, which is reflected in their performing comprehensive assessments, evaluating diagnostic tests, detecting complications, implementing prevention, education and psychological support activities, and conducting clinical follow-up of patients. In addition, they perform management tasks and refer patients to other levels of care or services. They are also a reference for both patients and/or family members as well as other healthcare professionals.5
There has been a generalised expansion in the competencies of ANPs and this has generated great interest both nationally and internationally and led to transformation of the healthcare systems in a number of countries.6 As a result, the push to unify criteria and achieve consensus on the competency framework has led to tools being designed to define and assess these functions.7–10
In Spain, many of the country's Autonomous Communities have set up different initiatives which include figures with innovative profiles and a series of competencies involving greater complexity and autonomy than that provided by the role of general care nurse.11 The aim is to respond to new demands for healthcare, mainly with regard to chronic diseases.12
In 2009, the roles of the technical and nursing staff at the Hospital Clínic de Barcelona were restructured, with nursing focusing exclusively on patient care. This led to the initiative to create a Nursing Clinic in our hospital's Diagnostic Imaging Unit.
The clinic has evolved and currently two ANPs work in this position, providing expert care, therapeutic patient education and follow-up, to ensure the best quality care possible.
Role of Advanced Practice Nursing in a diagnostic imaging departmentAccording to Vargas Acauan et al.,13 nursing work in an imaging department requires very specific knowledge, in order to be able to recognise, prevent and provide assistance for possible complications related to imaging processes, with a focus on quality of care and from the perspective of patient safety.
The ANP in these units promotes specialised care with an overall approach coordinated with the rest of the healthcare professionals throughout the entire care process, in order to provide the best possible patient care. They are an active member of a multidisciplinary team and collaborate closely with a range of healthcare professionals, communication with whom is essential for proper coordination of patient-focused care.
At our centre, ANPs currently participate in the following healthcare processes:
- 1
Targeted metabolic therapies with radiopharmaceuticals in Nuclear Medicine.
- 2
Computerized tomography colonography studies and gastrointestinal transit time in colon.
- 3
Interventional processes in the modalities of computerized tomography and ultrasound in the musculoskeletal, chest, abdomen, genitourinary and neurology sections.
- 4
Cerebral arteriograms with radial access in outpatients.
- 5
Contrast media safety:
- a)
Patients with kidney failure requiring administration of intravascular iodinated contrast with glomerular filtration (GF) values <30 ml/min.
- b)
Patients with a history of adverse drug reactions (ADR) to radiological contrast media (RCM).
- c)
Assessment, monitoring and therapeutic education for patients with parotitis/sialadenitis associated with the administration of intravenous iodinated contrast.
- d)
Assessment and monitoring of RCM extravasation.
- a)
The interventions carried out by ANPs include a prior assessment with a comprehensive previous medical history to identify risk factors. This information is crucial to detecting, managing and streamlining the care process effectively and safely. They also provide information, therapeutic education and emotional support to both the patient and their family, always focused on the patient's well-being. They plan the interventions to be conducted in the department's various nursing units and carry out a continuous assessment and monitoring of the process.
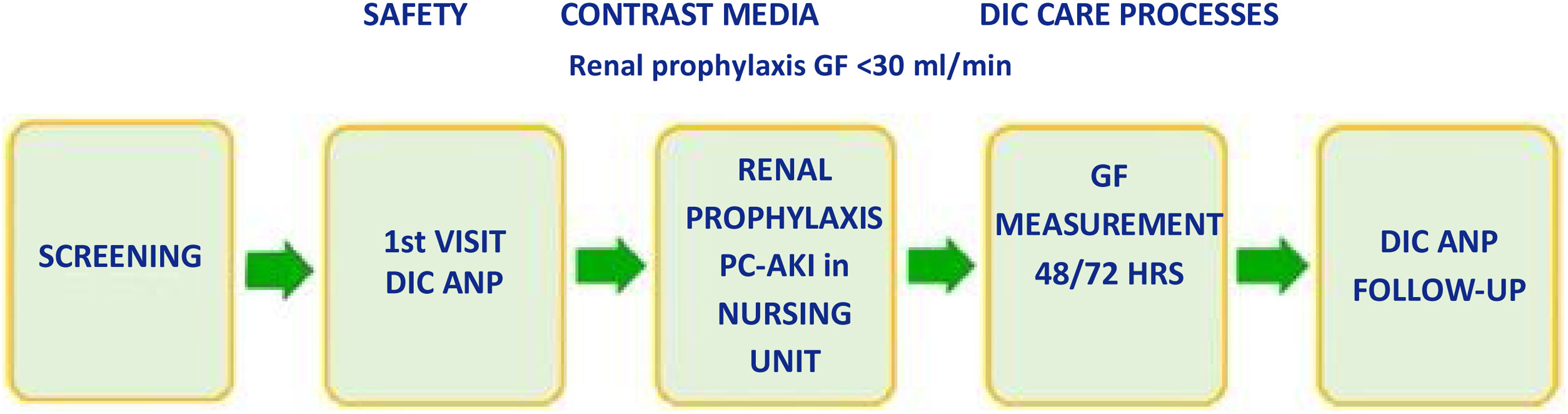
Advanced Nursing Practice plays a key role in facilitating communication with the multidisciplinary team, primary care centres and other hospitals. These nurses are responsible for requesting consultations with specialised services, such as allergy, haemostasis and primary care, in order to ensure that comprehensive care is provided (Fig. 1).
The process management software we use has been adapted to meet the current needs of the department, enabling initial screening which generates a first nursing visit prior to the procedure. With this system, the GF value from the patient's previous analysis can be viewed and any patients with a history of adverse reaction to an RCM can be identified. This allows us to anticipate and plan the nursing intervention.
All processes in which ANPs are involved include the following:
- •
Asynchronous appointment: a prior non-simultaneous "store-and-forward" screening is made, which generates a first nurse appointment.
- •
First appointment, which includes an overall assessment of the patient:
- ◦
Review of clinical progress and reports from medical case conferences, previous medical history, usual drug treatment and risk factors for each type of process. This assessment includes validated scales as measurement instruments (Barthel, pain scale, Goldberg).
- ◦
Therapeutic education and information to the patient about the care process.
- ◦
The assessment and any interventions performed are recorded in the electronic medical record (EMR), providing continuity of care.
- ◦
The patient/family is provided with the telephone number and email address of their reference ANP.
- ◦
If necessary, specialised services (for example, allergy, haemostasis), primary care or other hospital centres are contacted.
- ◦
- •
Check-up visit, which includes assessment and follow-up after the interventions carried out. Our department's safety and quality indicators are also recorded in an internal database.
The records are documents specific to the profession and are essential to the medical records, for the purposes of optimising communication between members of the healthcare team and, consequently, ensuring continuity of care; they are also a legal support, while at the same time enabling retrospective evaluation of the quality of care.14
Role of ANPs in RCM safety in a diagnostic imaging departmentRCM is administered daily to thousands of patients, and although it is very safe, it is not without risks. It is therefore necessary to understand its indications, mechanisms of action, contraindications, adverse effects and routes of administration.14
ANPs are responsible for these processes in terms of the safety of RCM.
a. Assessment and monitoring of glomerular filtrationPatients requiring intravascular iodinated contrast administration with GF <30 ml/min.
GF, calculated from serum creatinine, is the recommended method for estimating renal function before administration of a contrast medium.15 The European Society of Urogenital Radiology (ESUR) defines post-contrast acute kidney injury as an increase in serum creatinine ≥0.3 mg/dl, or more than 1.5 times its baseline value, which occurs in the first 48−72 h after intravascular administration of iodinated contrast, without another concurrent cause to explain it.16
Davenport et al.17 state that it is impossible to separate causal from coincidental acute kidney injury since most studies on post-contrast acute kidney injury have not included a control group of similar patients who were not exposed to contrast media. In our hospital, by implementing the ESUR 10.0 guidelines16 and avoiding patients coming to the test dehydrated, considered to be a risk factor for PC-AKI, we have made oral hydration universal in the process, consisting of drinking 500 ml of water 2 h before the test and drinking 2,000 ml of water during the 24 h afterwards (except in patients who have water restriction).18
Intravenous hydration, either with saline or bicarbonate solutions, is currently the cornerstone of PC-AKI prophylaxis in GF <30 ml/min.16 However, oral hydration may also be an option in the prophylaxis of post-contrast acute kidney injury, as indicated by the results of the NICIR trial19 and a meta-analysis published by Zhang et al.20 (Fig. 2).
ANP interventionOutpatient:
- •
Asynchronous appointment: a prior non-simultaneous "store-and-forward" screening is made, which generates a first nurse appointment.
- •
Comprehensive assessment of the patient as explained in the previous section.
- •
Review GF values from the previous blood test (valid for six months) in the EMR.
- •
For GF of 30−15 ml/min and no medical contraindication, renal prophylaxis is prescribed, to be performed in the nursing unit of the diagnostic imaging department at Hospital Clínic de Barcelona.
- •
Record the intervention in the EMR for continuity in healthcare and proper communication with the other healthcare professionals.
Renal prophylaxis protocol:
- -
3 ml/kg/h normal saline/1/6 M bicarbonate solution. Intravenously 1 h before the procedure.
- •
If GF <15 ml/min. The requesting physician must assess whether or not to administer intravenous iodinated contrast. If necessary, they should make arrangements with the corresponding day hospital to carry out a long-term renal prophylaxis regimen.
- •
Long-term renal prophylaxis protocol:
- -
3 ml/kg/hr. normal saline/1/6 M bicarbonate solution. Intravenously 1 h before the procedure.
- -
1 ml/kg/h normal saline/1/6 M bicarbonate solution. Intravenously 4 h after the procedure.
- •
ANP requests and schedules outpatient blood screening tests at 48/72 h
- •
The next day, follow-up and evaluation of the blood test results in the EMR. In case of an increase in serum creatinine >0.3 mg/dl, the analysis should be repeated after 15 days.
- •
If the increase persists, we should contact the referring radiologist and the requesting physician for assessment.
- •
Hospitalised patient:
- •
Asynchronous appointment: a prior non-simultaneous "store-and-forward" screening is made, which generates a first nurse appointment.
- •
Comprehensive patient assessment.
- •
The GF and creatinine values from the previous blood test are reviewed in the EMR (valid for seven days) and the procedure is the same as for outpatients.
- •
The hospital nursing staff of the unit where the patient is admitted is contacted to inform them of the need to carry out the renal prophylaxis protocol and be able to adequately coordinate the time for performing the test. The physician in charge of the patient must assess whether there are any contraindications and prescribe the necessary fluid therapy prior to the test.
- •
If the patient has been prescribed fluid therapy as part of their usual treatment, it will not be necessary to carry out this protocol.
- •
The ANP orders follow-up blood tests at 48/72 h, which should be drawn by the hospital nursing staff.
- •
The next day, follow-up and assessment of the blood test results in EMR and, in case of an increase in serum creatinine >0.3 mg/dl, we should contact the responsible radiologist and the requesting physician for assessment.
According to the World Health Organization (WHO), an ADR is defined as a "harmful and unwanted reaction that occurs after the administration of a drug, at doses normally used in humans, to prevent, diagnose or treat a disease".
In the approach to patients who require the administration of RCM, the risks and benefits of its use must be considered on a personalised basis.21 Both iodinated contrast media (ICM) and gadolinium contrast media are associated with a very low rate of adverse effects; most of these are mild and can be managed by the healthcare professionals in the department, without the need to provide treatment or transfer the patient to an accident and emergency department.22
There is often confusion between adverse reactions to RCM and allergies. True allergic reactions involve the activation of the immune system and a large percentage of patients are mistakenly labelled as allergic to RCM, with the inconvenience this means for future administrations. Hypersensitivity reactions are not predictable. It has been recommended that the term "hypersensitivity" be used to describe all reactions to RCM which are not toxic or are nonspecific, reserving the term "allergic" for those hypersensitivity reactions in which an immunological mechanism is recognised as the basis of the reaction.23
Most adverse effects that occur after RCM administration are mild events which are not life-threatening for the patient. Many reactions resolve after a short period of observation without treatment. Therefore, it is important to make a correct initial assessment and have a standardised classification system to minimise risks. The American College of Radiology (ACR) guidelines21 propose classifying immediate reactions according to the degree of severity into three groups: mild, moderate and severe.
Skin challenge tests for RCM should be mandatory after the onset of a reaction, although the methodology is not standardised.24 Each medical centre has its own protocols and it is not always possible to follow this recommendation.
According to the time interval between administration and the onset of symptoms, adverse reactions are divided into immediate reactions, which occur within one hour after administration of RCM, and non-immediate reactions, which appear more than one hour after exposure.25
In its guidelines, the ESUR16 explains that the management of acute adverse reactions is the same for reactions to ICM, gadolinium contrast media and ultrasound contrasts, and recommends that multidisciplinary teams should receive regular training in how to manage these reactions.
At Hospital Clínic in Barcelona, when a moderate or severe reaction occurs, the allergy and anaphylaxis protocol is activated in the nursing unit, which includes a blood test, referral to the allergy department and an ADR notification to our centre's own programme, which notifies the Spanish pharmacovigilance system, which includes the centre for the Autonomous Community and the Spanish Medicines Agency.
It is essential to record the information and details of the patient's reaction in the EMR: name, batch, RCM dose, symptoms and treatment required in order to conduct proper follow-up and for future occasions.
At our centre, ANPs perform prior screening in patients who have had a previous reaction and require further administration of RCM (Fig. 3).
ANP intervention- •
Asynchronous appointment: a prior non-simultaneous "store-and-forward" screening is made, which generates a first nurse appointment.
- •
Comprehensive assessment of the patient where the EMR is checked for any reports from an Allergy specialist indicating how the patient should be managed. If there is none, the ANP conducts an assessment and classification of cases with the information provided by the patient and the clinical presentation: when it happened, whether it happened at our centre or another, whether medication was required, and whether the patient had to go to Accident and Emergency. With this information, the nurse classifies the type of ADR as mild/moderate/severe.
- •
Depending on the information provided by the patient:
- -
The requesting physician and radiologist are contacted for an alternative test.
- -
The allergy department is consulted and the ANP conducts follow-up to monitor the patient's management in future administrations.
- -
- •
At the inpatient level, it has been agreed between the radiodiagnosis and allergy departments that in patients with mild ADR who have been traditionally given prophylactic medication prior to the administration of RCM and do not have a medical report, the same procedure should be followed so as not to delay procedures. In these cases, the ANP should contact the patient to verify the information and confirm that they have the protocolised medication regimen, to ensure that the appointment does not have to be rescheduled due to lack of preparation.
- •
If the allergy department has assessed the situation, their recommendations should be followed.
- •
The intervention and the action to be performed on the day of the procedure are recorded in the EMR to ensure continuity of care.
- •
A telephone assessment and follow-up is carried out 24 h after the administration of the RCM.
This is a very rare adverse reaction, with a self-limiting course and uncertain pathogenesis.26 True incidence remains unclear and some studies believe it may be underdiagnosed.27
The first cases of ICM sialadenitis were described in 1956 by Sussman and Miller,28 who coined the term "iodine mumps" due to the similarity with the salivary gland inflammation caused by the mumps virus.
Abnormal inflammation of the salivary glands occurs in association with intravascular ICM administration and is characterised by rapid, usually painless, enlargement of the salivary glands.29,30
The patient develops swelling in the affected glandular area (parotid, submandibular) accompanied by mild inflammatory symptoms (erythema, oedema, pain), all of which is self-limiting, resolving itself spontaneously in a few days.
Treatment for this process is usually conservative, with observation, supportive therapy and patient education. Sialadenitis may recur after further ICM administration, and premedication protocols are not useful as a preventive method.23
ANP interventionThese patients are usually referred to the ANP with a suspected hypersensitivity reaction, but on assessment it is confirmed to be parotitis secondary to ICM administration.
- •
They contact the patient and assess the symptoms and associated risk factors, and provide therapeutic education and emotional support.
- •
They confirm the patient has understood the information provided and help resolve their doubts with active and empathetic listening, reinforcing the fact that it is not an allergic reaction and that it will likely happen again with subsequent administrations of ICM.
- •
If the patient requires further administration of RCM, assessment and telephone follow-up is provided within 24 h of the new RCM administration, which is recorded in EMR
Proper selection of the intravenous catheter is essential31 for the flow we want to administer, the speed of administration, the viscosity of the contrast and the insertion site. The peripheral route should be the route of choice for the administration of RCM, especially if it is done with an injector. The needle catheter, better known as “Abocath®”, is the most widely used in outpatients for its versatility. For central catheters and peripherally inserted venous catheters,32 the manufacturer's instructions should be followed regarding their suitability for contrast use. In the case of patients with a subcutaneous reservoir, we need to know whether or not the device allows high-flow injections.
Extravasation of iodinated contrast means the accidental release of RCM from the intravascular space into adjacent tissues and compartments due to rupture of the vein; it should be recorded as an adverse event related to a procedure. The incidence of this adverse event is reported to be in the range of 0.1–0.9% in some Spanish studies or up to 1.2% in the latest revision of the ACR guidelines.21
There are aetiopathogenic factors associated with the technique and factors associated with the patient (for example, capillary fragility, distal veins). Most extravasations are limited to the immediately adjacent soft tissue, skin and subcutaneous tissue.
If the extravasation is severe enough to result in compartment syndrome (occurring in less than 1% of cases), a fasciotomy may be necessary to prevent muscle necrosis and nerve damage. This syndrome develops when pressure within a muscle compartment increases to dangerous levels, compromising blood circulation and nerve function. Immediate symptoms are swelling, tightness and/or stabbing pain, although sometimes it occurs with little or no discomfort,16 in which case sensitivity, swelling, erythema, paraesthesia and perfusion should be assessed, in addition to monitoring for possible progression to more serious lesions which can develop over hours or days.
According to ACR and ESUR, most extravasations are corrected with local measures:
- -
Elevation of the limb.
- -
Application of dry cold/heat.32
- -
Monitoring of the wound.
Elevation is indicated because it decreases capillary hydrostatic pressure and promotes reabsorption. There is some controversy regarding the use of hyaluronidase, recommended by some authors.16 With regard to manual compression and aspiration of extravasated fluid through the catheter, some healthcare professionals state that the manoeuvre is productive in some cases and does not involve risk. By applying heat, vasodilation is promoted, which increases reabsorption, and by applying cold, vasoconstriction is promoted, which reduces pain and inflammation. Heat and cold should be dry, as moisture on fragile skin can cause maceration and deterioration. Dr Roca i Sarsanedas33 presented a comparative study between the application of cold alone and the combination with heat, demonstrating that the combined method (heat during the first hour and cold for 24 h) every 3−4 h), helped reabsorption and reduced inflammation. He also recommended marking the edges so that the progress can be assessed. In serious lesions involving alteration of perfusion or decreased range of motion, referral should be made to a specialist for assessment.
When the patient leaves the hospital after an extravasation, we must instruct them on how to monitor symptoms such as tingling, numbness or decreased range of motion, which may indicate the development of a serious lesion hours later. The recording and documentation of extravasation and treatment in the patient's EMR allows us to improve the safety of healthcare organisations and minimise the likelihood of adverse events, and facilitates the provision of scientific evidence and advancement in the culture of patient safety, as well as contributing to the development of best nursing practices.34,35
ANP interventionFrom the nursing unit we are informed by email that an extravasation has occurred: affected limb, quantity, type of RCM, clinical symptoms, immediate outcome and recommendations given.
- •
At 24 h telematic/face-to-face follow-up in order to assess signs and symptoms such as tingling, numbness or decreased range of motion that may indicate a serious lesion.
- •
Request that the patient or family member/caregiver measure the diameter of the extravasation using the marks made the previous day in the nursing unit.
- •
In case of suspected serious lesion, the appointment will be in-person.
- •
Recorded in EMR. Resolve any questions or doubts the patient may have.
- •
Pain assessment with a validated scale: numeric pain scale
- •
Discharge or referral to a specialist doctor.
- •
Record in EMR and add extravasation alert.
- •
In patients with a history of RCM extravasation and known difficulty with previous venous access, we should assess the possibility of intravascular access using ultrasound and coordination with the Angiography radiology department.
The ANP in a diagnostic imaging department provides comprehensive, specialised care to patients, collaborates with interdisciplinary teams and acts as a reference healthcare professional for both patients and/or family members and healthcare professionals alike. They participate in case management, planning interventions and ensuring continuity of care. They coordinate healthcare at various levels of care and collaborate in research and evidence-based practice, in order to improve the outcomes of treated patients, and provide sustainability to the diagnostic imaging department, and therefore to the healthcare system, since planning interventions avoids unnecessary rescheduling or cancellation.
FundingThis study received no specific grants from public agencies, the commercial sector or non-profit organisations.
CRediT authorship contribution statementAll the authors declare having contributed to the preparation of this article, in the preparation of the draft copy, the critical review of the intellectual content, and the final approval of the submitted manuscript.