Facial fractures, often related to traffic accidents, assault, work-related accidents, or falls, account for a considerable number of emergencies in our hospitals and are associated with high morbidity and mortality.
Multidetector computed tomography (MDCT) is the imaging technique of choice in this scenario because it is widely available, fast, and useful for characterising facial fractures and associated complications, including those located in the head. For all these reasons, MDCT is fundamental in the clinical management of these patients and in planning surgery.
This paper describes the radiological anatomy of the facial region, underlining the importance of the facial buttresses, and it indicates the key points necessary for carrying out a structured approach and elaborating the corresponding radiologic report.
Las fracturas faciales, relacionadas frecuentemente con accidentes de tráfico, agresiones, accidentes laborales o caídas, constituyen un considerable número de urgencias en nuestros hospitales y asocian, además, una elevada morbimortalidad. La tomografía computarizada multidetector es la técnica de imagen de elección por su amplia disponibilidad y rapidez, y porque permite tanto la caracterización de las fracturas faciales como de las complicaciones asociadas, incluyendo las de localización craneal. Es, por tanto, fundamental para orientar el manejo clínico y la planificación quirúrgica. En este trabajo se describe la anatomía radiológica de la región facial, destacando la importancia de los contrafuertes o arbotantes faciales, se ilustran los hallazgos característicos en las fracturas faciales, y se indican los puntos clave necesarios para su abordaje estructurado al realizar el correspondiente informe radiológico.
Among hospital emergency departments, facial trauma poses a challenge to radiologists due to the complexity of the facial anatomy and, therefore, the fracture lines, to the subtlety of some findings, and to the difficulty in obtaining synclitic images which is associated with the patient's condition. Facial trauma is a relatively common entity, with a global mortality rate of 15–20%, and is present in more than 50% of deaths due to multiple trauma. It aetiology is associated primarily with road traffic accidents, assaults, accidents at work and falls,1 and nowadays with an increase in sporting and leisure activities.
The aim of imaging studies in facial traumatology is to determine the number and location of fractures, paying particular attention to identifying lesions to functional structures of the face associated with occlusion, swallowing, vision or neighbouring elements in the neck (cervical vertebrae) and skull (cranial vault, base of skull and intracranial structures).2
Multidetector computed tomography (MDCT) is the imaging technique of choice for assessing facial trauma due to its wide availability, its speed and the fact that it can be used to characterise facial fractures, soft tissue injuries and associated complications.
Although the conventional written radiology report still dominates,3 the structured report has gained fans, presumably because of its better comprehensibility and legibility and because it reduces errors attributable to the use of voice recognition programmes. Between 4.8% and 22% of reports created using voice recognition programmes can have errors, and 1.9% of these errors can alter the report's interpretation.4–11 Times have changed, and we must adopt the use of structural reports in those areas where it is possible.12
TechniqueThe area scanned extends from the frontal sinuses to the mandibular symphysis. There is no need to administer intravenous contrast except to rule out the presence of an associated vascular lesion. Images are acquired using the minimum detector width available, which in our centre is 0.5mm. It is also recommended to obtain reconstructions in the coronal and sagittal planes with a bone window from 0.5 to 2mm in width, as well as axial planes with a soft tissue window of greater size. Acquiring images with such thin slices means that a three-dimensional reconstruction is possible in all cases, which is especially helpful for planning surgical treatment.13
Preoperative images do not only have diagnostic value in describing the existence of all fractures, but also for the creation of virtual (3D) or real (stereolithographic) preoperative models that include all fragments in their displaced position, held in place by rods or cylinders. Postoperative models will show the patient with all possible osteosyntheses (surgical plan).14
Image processing will also help to:
- •
Virtually reconstruct missing or displaced bone fragments.
- •
Create personalised preformed osteosynthesis plates.
- •
Where personalised osteosynthesis plates cannot be used, preoperative models will help with preforming standard plates before entering the theatre.
- •
Create facial prostheses to reconstruct bone defects.
The facial skeleton is made up of four unpaired bones (frontal, ethmoid, vomer and mandible) and five paired bones (zygomatic, maxilla, nasal, lacrimal and palatine), which form a bony protective frame over the structures of the orbit, paranasal sinuses and nasal and buccal cavities. Behind them and supporting this frame, is the vitally important sphenoid bone, with the pterygoid processes on its internal surface. There are some systems that divide the facial skeleton into three parts, the upper third, consisting of the frontal bone, the lower third, corresponding to the mandible, and between them the middle third which extends from the orbital rim to the alveolar process of the maxilla15 (Fig. 1).
3D reconstruction images. (A) Division of the facial skeleton into thirds. Frontal (F), zygomatic (Z), sphenoid (S), ethmoid (E), lacrimal (L), nasal (N), upper maxilla (MX) and vomer (V). The upper third corresponds to the frontal bone. The middle third, to the bones located between the line passing through the superior orbital rim and the frontozygomatic, frontomaxillary and frontonasal sutures and the line along the alveolar process of the upper maxilla (red lines). The lower third corresponds to the mandible. (B and C) Maxillofacial buttresses. Vertical: medial maxillary (M MX), lateral maxillary (L MX), posterior maxillary (P MX) and posterior vertical mandibular (PV MD). Horizontal: upper transverse maxillary (UT MX), lower transverse maxillary (LT MX), upper transverse mandibular (UT MD) and lower transverse mandibular (LT MD).
In the bones of the facial skeleton, eight buttresses or pillars can be identified, where the bone is thickest and where the forces generated by trauma are distributed.13
Four of these buttresses are vertical and four are horizontal (Table 1).16 All of them have two-part names; the first part refers to the bone they are part of (maxilla or mandible) and the second to the surface of said bone on which they are found, with different terms for vertical (medial, lateral and posterior) and horizontal (superior and inferior) buttresses.
Facial buttresses. Location and complications of fractures crossing them (see coloured diagram in Fig. 1).
| Vertical | |
| ■ Medial maxillary | Location: nasofrontal suture, lateral margin of piriform aperture and alveolar process of maxillaIncludes medial wall of orbit and maxillary sinusComplications: cerebrospinal fluid fistula, orbital complications, lesion of the nasolacrimal duct, lesions of the medial canthal ligament, epistaxis |
| ■ Lateral maxillary | Location: frontozygomatic suture, lateral orbital rim and zygomaticomaxillary suture, alveolar process of maxillaIncludes lateral wall of orbit and maxillary sinusComplications: lesion of the lateral canthal ligament, orbital complications |
| ■ Posterior maxillary | Location: pterygoid processesComplications: lesion of the carotid artery, carotid-cavernous fistula |
| ■ Posterior mandibular | Location: posterior margin of the mandibular ramusIncludes condyle and angle of mandibleComplications: temporomandibular luxation |
| Horizontal | |
| ■ Upper transverse maxillary | Location: frontomaxillary suture, inferior orbital rim, zygomatic bone and zygomaticotemporal sutureIncludes floor of orbitComplications: orbital complications |
| ■ Upper transverse maxillary | Location: alveolar process of maxillaIncludes hard palateComplications: malocclusion, avulsion and fracture of the teeth |
| ■ Upper transverse mandibular | Location: alveolar process and rami of mandibleComplications: malocclusion, avulsion and fracture of the teeth, lesion of the inferior alveolar nerve |
| ■ Lower transverse mandibular | Location: lower margin of the mandibleComplications: malocclusion, lesion of the inferior alveolar nerve |
The buttresses support the functional units of the face and absorb the forces that act on the bones and on the important structures they contain (brain, eyes, etc.). The involvement of these buttresses can be a predictor of potential complications, as well as altering the dimensions and normal functioning of the face, meaning that they need to be set surgically using osteosynthesis with plates, screws or even bone grafts, generally reinforcing the affected buttresses. It is in understanding this surgical management that knowledge of these buttresses is of interest to radiologists.
Classification of facial fracturesUpper thirdFrontal fracturesFractures of the upper third typically affect the walls of the frontal sinus due to the reduced thickness of the bone in this area.16
The most common is an isolated fracture of the anterior wall of the sinus or one that simultaneously affects the anterior and posterior walls, associated with tearing of the mucosa with haemorrhage and oedema within the sinus, as well as in the adjacent soft tissues that can mask the associated bone depression. Fractures that affect both the anterior and posterior walls are generally associated with other facial fractures and are often a result of very high energy impacts. It is also possible for the fracture to extend downward, reaching the superior orbital rim.15
Extension to the medial wall of the sinus and the nasofrontal duct can give rise to a mucocoele and consequently obstruct the drainage of the sinus, often requiring surgical treatment.16
Isolated fractures of the posterior wall of the sinus are rare and are often an extension of a fracture of the base of the skull or the cranial vault.15
- •
Communication with the anterior cerebral fossa: risk of cerebrospinal fluid leaking due to tearing of the dura15,17 with the appearance of rhinorrhoea.
- •
Herniation of the cerebral parenchyma towards the sinus.
- •
Pneumoencephalus.
- •
Possible infectious and traumatic intra- and extra-axial intracranial lesions.
- •
Indicators of injury to the nasofrontal duct:
- –
Sever obstruction of the same.
- –
Fracture of the floor of the frontal sinus.
- –
Fracture of the anterior ethmoid sinuses and anterior wall.
- –
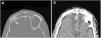
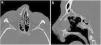
Frontal fracture. (A) Axial computed tomography (CT) with a bone window. Comminuted fracture of the anterior and posterior walls of the frontal sinus with occupation of the same and communication with the anterior cerebral fossa. (B) Axial CT with a brain window. Laminar subdural haematoma and bilateral frontobasal contusive foci.
In 1901, French surgeon René Le Fort performed numerous methodical experiments that involved hitting cadavers with a wide variety of mechanisms, forces and objects. This enabled him to describe three main patterns of fracture of the upper maxilla.18,19
Le Fort's fracture classification has been used for year for complex traumas of the middle third of the face. Although this system has not been completely abandoned, the current trend is to speak of facial subunits that imply certain individual principles with regard to surgical management.
In the report, the most correct method is to focus on the system used by the team of maxillofacial surgeons at our centre. Using the Le Fort classification of fractures in the report, in spite of the difficulty of finding pure fracture lines, is of use to the maxillofacial surgeons, as it facilitates global comprehension of the trauma, informs them about the energy of the impact and alerts them to associated lesions. Moreover, it could be beneficial in any case where someone might want to later analyse our work. For these reasons, and to understand the how the approach to facial trauma has evolved, we have decided to briefly cover firstly the Le Fort classification of fractures and subsequently the classification of the middle third of the face into subunits.
Each of the Le Fort fractures is caused by a force of a different intensity, but the most important thing is that all cases involve a fracture of the pterygoid processes and therefore of the posterior maxillary buttress.
The three types may occur simultaneously or in isolation, and each may be uni- or bilateral. Even in bilateral cases, they are not always symmetrical, but can take different trajectories on either side.
Fracture locations found in one of Le Fort's patterns and not the others are known as specific fractures (Table 2 and Fig. 3),20 and knowledge of these enormously simplifies differentiation between the three types: Le Fort I, also known as a “floating palate” because the hard palate is separated from the base of the skull; Le Fort II, known as a “pyramidal” fracture or “floating maxilla” as the resulting fragment is triangular or pyramidal in shape and corresponds to the maxillary bones, and Le Fort III, known as “craniofacial disassociation” as the facial skeleton is separated from the rest of the base of the skull (Fig. 4).
Location of fracture lines and specific fractures in the Le Fort patterns.
| The pterygoid process is always involved | Le Fort I (floating palate) | Le Fort II (floating maxilla) | Le Fort III (craniofacial disassociation) |
|---|---|---|---|
| Fracture lines | Hard palate. Lateral, anterior and medial walls of the maxillary sinus. Nasal bone | Lateral and anterior walls of the maxillary sinus. Floor and medial wall of the orbit. Nasal bones | Zygomatic arch. Lateral and medial walls of the orbit. Nasofrontal suture |
| Specific fracture | Hard palateNasal boneMedial wall of maxilla | Floor of orbit | Lateral wall of orbitZygomatic arch |
In the current division into subunits of the middle third of the face, we speak of: the nasoorbitoethmoid (NOE) region, the nasoseptal region, the zygomaticomaxillary complex (ZMC) and the occluding fragment of the maxillary bone.
Nasoorbitoethmoid fracturesThese fractures are caused by high energy trauma to the root of the nose, which is transmitted posteriorly through the ethmoid bone.
The fracture pattern affects the nasal bones, the septum and the ethmoid sinuses that make up the medial wall or the orbits, which are very thin and easily fractured.
All NOE fractures are made up of a single fragment or a series of comminuted fragments split along the five cardinal tracts. These five cardinal tracts are the lateral surface of the nasal bone together with the piriform aperture, tracts which cross the medial maxillary buttress, the inferior orbital rim together with the floor of the orbit, the medial wall of the orbit and the frontomaxillary suture. An NOE fracture must involve at least four for these five cardinal lines, so they must be specifically sought out in cases where there is doubt regarding the existence of an NOE fracture pattern21–24 (Fig. 5).
(A) Representation of the five cardinal lines of the NOE region: nasal bone and piriform aperture (blue), medial maxillary buttress (yellow), floor of orbit (green), medial wall of orbit (purple) and frontomaxillary suture (red). (B and C) Axial computed tomography (CT) with a bone window and 3D reconstruction. Comminuted left NOE fracture with displaced and depressed fragments. Involvement of the nasolacrimal duct (arrow tip). Palpebral emphysema and blood in the sinus. (D and E) Axial CT with a bone window and 3D reconstruction. Left NOE fracture with large fragment without displacement. Fracture of the left maxillary sinus with blood in the sinus and the external wall of the left orbit (arrow tip).
Clinically, they are characterised by depression of the root of the nose (saddle nose) and there may be associated exophthalmos due to an increase in intraorbital volume, telecanthus (increased distance between the medial canthus of each eye) due to lesion of the medial canthal ligament, or rhinorrhoea and anosmia due to lesion of the cribiform plate.
Anatomically, the importance of the aforementioned medial canthal ligament, which laterally joins the tarsus of the upper and lower eyelids and medially inserts in the region of the lacrimal crests in the medial orbit, is worth noting.21,25
Although the medial canthal ligament cannot be seen in computed tomography (CT), the specific degree of comminution in its bone insertion together with the clinical examination are very important data with regard to surgical planning.
In addition to the tendon, attention should also be paid to the nasolacrimal duct and lacrimal sac, the olfactory nerve and the ethmoid vessels.
Key observations:
- •
Comminution or simple fracture.
- •
Unilateral or bilateral.
- •
Assess the medial rim of the orbit, where the medial canthal tendon inserts.
- •
Obstruction of the nasolacrimal duct.
- •
Involvement of the nasofrontal duct (frontal mucocoeles).26,27
- •
Study of the telecanthus and/or enophthalmos.
The nasal bones are the most commonly broken bones in the body.
These bones articulate with the nasal process of the frontal bone and with the frontal process of both maxillary bones, forming the so-called bony nasal pyramid. The posterior surface of the nasal bones articulates at the midline with the nasal septum, the main components of which are, from front to back: the medial wall of the major alar cartilages, the quadrangular cartilage, the perpendicular plate of the ethmoid bone and the vomer. The lower-front part, the septum is in contact with the anterior nasal spine of the maxilla. The aforementioned cartilaginous portion of the septum and the bony nasal pyramid articulate with the upper lateral cartilages. The latter's integrity is highly important to avoid post-traumatic nasal deformity, and that of the nasal septum in turn is essential for supporting the anatomy of the bridge and tip of the nose, as well as airway patency.28,29 Fractures of the anterior nasal spine are considered a marker for fracture or luxation of the nasal septum.28
One of the most widely used classifications for nasal fractures is that of Stranc and Robertson,30 which is based on impact type (Fig. 6):
- •
Lateral impact. More common and better prognosis. Disruption between bone and cartilage compartments is rare and there may be septal involvement:
- –
Grade 1: unilateral depression of the nasal pyramid.
- –
Grade 2: lateral displacement of the contralateral nasal bones.
- –
Grade 3: displacement of both maxillary frontal processes.
- –
- •
Frontal impact. Three planes are defined, which determine the degree of severity:
- –
Grade 1: absence of involvement behind the plane joining the lower edge of the nasal bones and the anterior nasal spine.
- –
Grade 2: involvement limited to the nose, in front of the orbital rims.
- –
Grade 3: associated orbital and probably intracranial involvement.
- –
The assessment of septal haematomas and the degree of involvement of the cartilaginous structures can rarely be adequately performed by CT.28
Key observations:
- •
Unilateral or bilateral.
- •
Comminution or simple fracture.
- •
Degree of displacement.
- •
Deviation from the midline.
- •
Soft tissue lesion.
These are caused by a direct trauma to the malar process and are known as tetrapod fractures as they can involve four pillars delimited by sutures: frontozygomatic, zygomaticomaxillary, temprozygomatic and sphenozygomatic (Fig. 7).
(A) 3D representative of the pillars of the zygomaticomaxillary complex (ZMC) delimited by the frontozygomatic (purple), temporozygomatic (red), zygomaticomaxillary (green) and sphenozygomatic (yellow) sutures. (B and C) Axial and coronal computed tomography (CT) with a bone window. Zingg type B fracture of the ZMC; the zygomatic bone is free and displaced medially, reducing the orbital volume. (D–F) 3D reconstruction, axial and coronal CT with a bone window. Zingg type C ZMC fracture with involvement of the four pillars and comminution of the zygomatic bone.
With a view to surgical treatment, the Zingg classification divides them into three types31:
- •
Zingg A: incomplete, isolated fractures involving only one branch of the zygomatic bone.
- –
A1: the branch involved is the zygomatic arch. Stable after closed reduction.
- –
A2: involvement of the rim and lateral wall of the orbit. Generally suitable for closed reduction.
- –
A3: involvement of the rim and floor of the orbit. Generally suitable for closed reduction.
- –
- •
Zingg B: complete malar tetrapod fractures with a single free zygomatic bone fragment. Unstable and require internal fixation.
- •
Zingg C: comminuted fractures. Always require surgical fixation.
After a fracture, the forces of rotation applied to the zygomatic bone by the masseter muscle can lead to difficulty chewing or an increase in orbital volume and enophthalmos. If there is medial rotation of the free zygomatic fragment, the degree of defect to the floor of the orbit may be underestimated in comparison to surgical findings.
Particular attention should be given to the sphenozygomatic suture, as displacement, overriding or angulation of this suture is the most sensitive indicator of misalignment and changes in the orbital volume and implies a high likelihood that the orbital apex will be involved, compromising the optic nerve and ophthalmic artery. Moreover, these fractures are difficult to correct once the bone has set poorly.32–35
Key observations:
- •
Medial displacement: malar depression and reduced mandibular opening.
- •
Lateral displacement: increased orbital volume, diplopia.
- •
Inferior displacement: increased orbital volume, diplopia.
These are mostly split into two types36–38:
- •
Pure: fractures of the internal walls of the orbit without involvement of the orbital rim. The eyeball acts as a transmitter of the force of the trauma.39,40 In most cases, the fracture occurs through the floor or medial wall of the orbit, as these sections of bone are the thinnest and most fragile.
- •
Impure: fractures that also involve the orbital rim in addition to the internal orbit. The main difference is that they require reduction of defects in the ring of bone around the orbit prior to repairing the internal orbit.
In pure blow-out fractures, the fractured floor of the orbit herniates towards the interior of the maxillary sinus, while in the less common pure blow-in fractures, the fractured floor of the orbit herniates towards the interior of the orbit.15 In both cases, the orbital rim remains intact.
The presence of herniation of fat, the inferior rectus muscle and the inferior oblique muscle must always be assessed, as must trapping of the latter two as a cause of diplopia, which may also be due to oedema and haemorrhage, which are often associated with such fractures. Fractures of the orbital floor can involve the infraorbital nerve canal.
Fractures of the lamina papyracea of the ethmoid bone in the internal wall are difficult to identify if there is no associated displacement or orbital emphysema. Such emphysema more commonly originates in the ethmoid sinuses than in the maxillary sinus in a fracture of the floor, as in the latter herniation, haemorrhage and oedema often seal the bone defect. The appearance of emphysema following the increase in intranasal pressure when the patient blows their nose is not uncommon in ethmoid fractures.15
Key observations41–43 (Fig. 8):
- •
Trapping of the extraocular muscles: diplopia.
- •
Fat herniation: cause of enophthalmos.
- •
Superior orbital fissure syndromes: involvement of the III, IV and VI cranial nerves and the first branch of the V, as well as the superior ophthalmic vein.
- •
Orbital apex syndrome: involvement of the optic nerve and ophthalmic artery.
- •
Assessment of the eyeball.
- •
Orbital emphysema, foreign bodies.
This is a subunit with its own separate management, equivalent to Le Fort type I and II fractures. It includes the lateral, anterior and medial walls of the maxillary sinuses, the piriform aperture, the nasal septum, the hard palate and the alveolar edge of the maxillary bone. In fractures of this type, the fragments are often impacted rearwards. Of greater importance than signalling whether the pterygoid process is affected is differentiating between:
- •
Complete fractures: the fragments are completely free and can move passively.
- •
Incomplete fractures: these are impacted fractures or those that do not cross the two cortical bones. They may require reduction by osteotomy.
The classification proposed by Chen et al. distinguishes three types of fractures of the hard palate with specific surgical treatment44:
- •
Type I: the fracture lines extend sagittally.
- •
Type II: the fracture extends coronally.
- •
Type III: comminuted fractures.
Key observations:
- •
Le Fort I and II fractures.
- •
Fractures of the palate.
- •
Simple or comminuted fracture.
- •
Altered occlusion.
- •
Dentoalveolar fractures.
These are the second most common fractures of the facial skeleton after nasal fractures, because the mandible is a prominent bone and the only mobile bone in the facial region.16 They are important from an anatomical, aesthetic and functional point of view, as they affect activities such as chewing and speech.
The following units are distinguished in the mandible: condyle (with head, neck and subcondylar region), coronoid process, ramus, angle, body, symphysis and parasymphysis region (separated by from the body by an imaginary line drawn from the canines), alveolar process (where the teeth are found) and basal segment (along the lower margin of the mandible). The angle of mandible is delimited above by the region of the third molar and below by the area of the inferior insertion of the masseter muscle (Fig. 9).
(A) 3D representation of the mandibular units. Coronoid (Cr), condyle (Cd), ramus (R), angle (A), body (B), symphysis (S), alveolar process (Av) and basal segment (BS). (B and C) 3D reconstruction. Fracture of the occluding segment of the maxilla with dentoalveolar involvement and marked displacement of the fragments (asterisk). Fracture of the mandibular symphysis (arrow) and both condyles with impaction (arrow tips). (D) 3D reconstruction. Bilateral fracture of the body of the mandible with marked posterior displacement of the free fragment and risk of compromising the airway.
The mandible has a characteristic U-shaped morphology and articulates with the skull via the synovial temporomandibular joints (TMJ), forming a ring-shaped structure that is the reason for the presence of two fracture lines after trauma. Occasionally, only one fracture is identified as some of the force of the impact dissipates through the TMJ.45 Fracture and luxation of the TMJ can also occur, and should be reduced prior to imaging.16 A high percentage of mandibular fractures are associated with one direct mechanism causing a fracture line at the site of the impact, and a second indirect mechanism due to transmission of the energy, with another fracture line at some distance from the initial impact.
The condyle is often the most affected region due to its structural weakness, and almost half of these fractures are caused by an indirect mechanism and associated with another type of mandibular fracture, commonly in the symphyseal or parasymphyseal region.17 In mandibular condyle fractures with displacement, this is often towards the midline due to the traction of the lateral pterygoid muscle that inserts at the head of the condyle. Sagittal fractures of the head of the condyle go unnoticed as they have no repercussions on eventual occlusion. Approximately 40% of mandibular fractures have more than one line1 and most affect both the superior and inferior mandibular buttresses.16
Fractures affecting the teeth are considered open. This is the case for fractures of the alveolar process.16 If displaced, dentoalveolar bone fragments often need to be removed as they often become devitalised. In dental avulsion or fracture of the crown, the presence of an ingested or aspirated tooth should be ruled out.45 Involvement of the mandibular canal along the ramus, angle and body of the mandible, between the mandibular and mental foramina, may be associated with a lesion of the inferior alveolar or dental nerve, which originates from the third branch of the trigeminal nerve, especially if there are displaced bone fragments larger than 5mm,45 giving rise to sensory alterations in the lower lip, chin, gums and mandibular teeth.16
Key observations1,45:
- •
Displaced fractures of the body of the mandible: inferior dental nerve lesion.
- •
Bilateral fractures of the body of the mandible: risk of compromising the airway due to posterior displacement of the tongue caused by lack of anterior support.
- •
Intraoral bleeding and haematomas in the floor of the mouth: risk of compromising the airway.
- •
Sagittal fractures of the mandibular condyle.
The various models of structured report in MDCT for facial trauma have been found to reduce reporting time by as much as 35%, increase diagnostic precision and facilitate the description of findings and their objective transmission to other specialists in the multidisciplinary team.46 Moreover, they open the door to “big data” analysis, and can be a source of information for generating radiological reports using programmes based on computer-aided neural networks.
Of course, the structured report for facial trauma has its detractors,28 who consider it to be merely a long list of unconnected points with no orientative value for reconstructive surgery. Nevertheless, a structured report need not do away with the advantages of conventional reporting and can adhere to the basic premises of brevity, clarity and relevance.47,48
We propose a structured report model based on the information contained in Table 3. With the aim of avoiding errors caused by fatigue, we first assess the cervical spine and cranial vault together with lesions to the associated soft tissues. We then study the pterygoid processes to determine whether we are dealing with a Le Fort-type transfacial fracture. Next, we identify the bone structures that form the three thirds of the facial region, paying special attention in each region to the key observations outlined above, which we include in the “observations” section.49
ConclusionsRadiologists’ knowledge of the patterns of maxillary fractures and their implication throughout the process of preoperative diagnosis and postoperative assessment is crucial to facilitate effective and, above all, efficient communication with the surgeon, which is considerably improved through the use of a structured radiological report agreed between radiologists and maxillofacial surgeons.
The accuracy of radiological tests will be a determining factor in the ability to later use suitable software for surgical planning, creating surgical guides, alloplastic materials and personalised miniplates.
Authorship- 1.
Responsible for the integrity of the study: ABR.
- 2.
Study conception: ABR.
- 3.
Study design: ABR, DDB.
- 4.
Data collection: ABR, DDB.
- 5.
Data analysis and interpretation: ABR, DDB.
- 6.
Statistical processing: Not applicable.
- 7.
Literature search: ABR, DDB, MMM, NN.
- 8.
Drafting of the article: ABR, DDB, MMM.
- 9.
Critical review of the manuscript with intellectually relevant contributions: ABR, DDB, MMM, NN.
- 10.
Approval of the final version: ABR, DDB, MMM, NN.
The authors declare that they have no conflicts of interest.
Please cite this article as: Boscà-Ramon A, Dualde-Beltrán D, Marqués-Mateo M, Nersesyan N. Tomografía computarizada multidetector en el traumatismo facial: informe estructurado y observaciones clave para un abordaje sistemático. Radiología. 2019;61:439–452.