Cardiac computed tomography showed a hypodense area in the apex of the left ventricle in a 57-year-old man with a history of anterior myocardial infarction three years earlier. To confirm or rule out a suspected thrombus, he underwent gadolinium-enhanced cardiac magnetic resonance imaging, contrast-enhanced two-dimensional transthoracic echocardiography, and three-dimensional transthoracic echocardiography. Multimodality imaging ruled out the presence of a thrombus.
Varón de 57 años con antecedente de infarto de miocardio anterior. En una tomografía axial computarizada (TAC) cardíaca realizada 3 años más tarde, se objetiva una imagen hipodensa en el ápex del ventrículo izquierdo. Ante la sospecha de trombo, se completa el estudio mediante resonancia magnética cardíaca (RMC) con gadolinio, ecocardiografía transtorácica (ETT) 2D con ecopotenciador y ETT tridimensional. A través de la imagen multimodalidad se comprueba la ausencia de trombo.
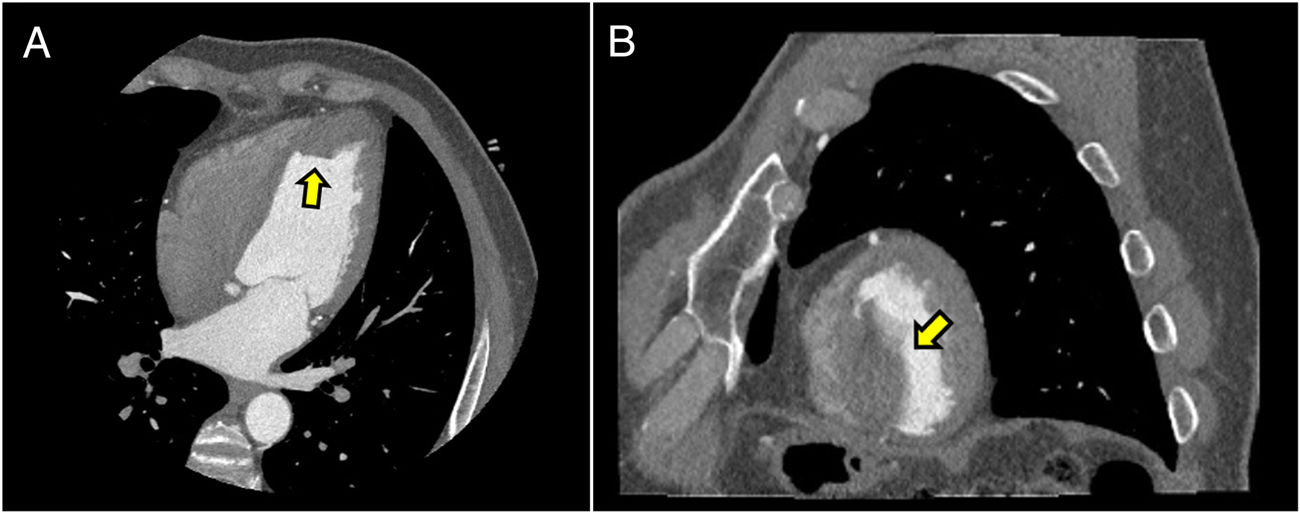
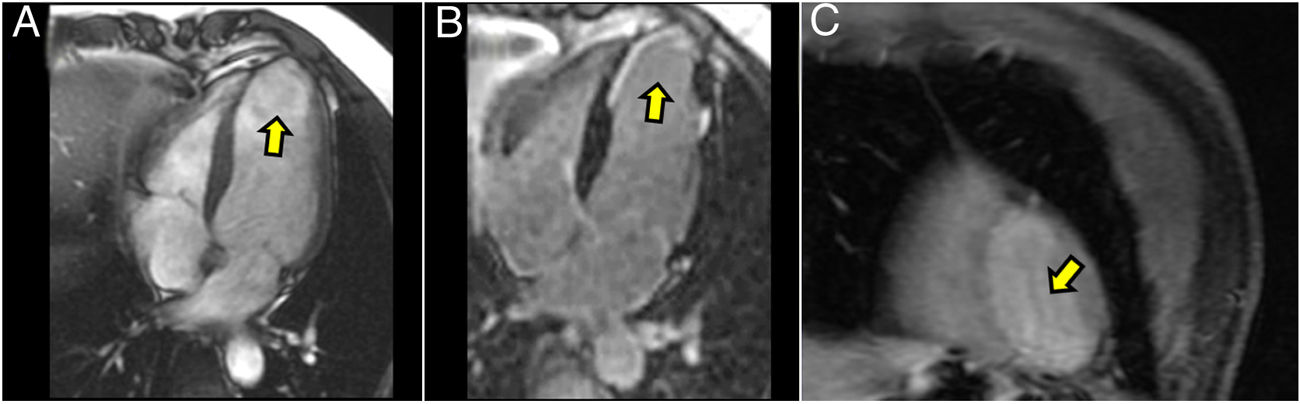
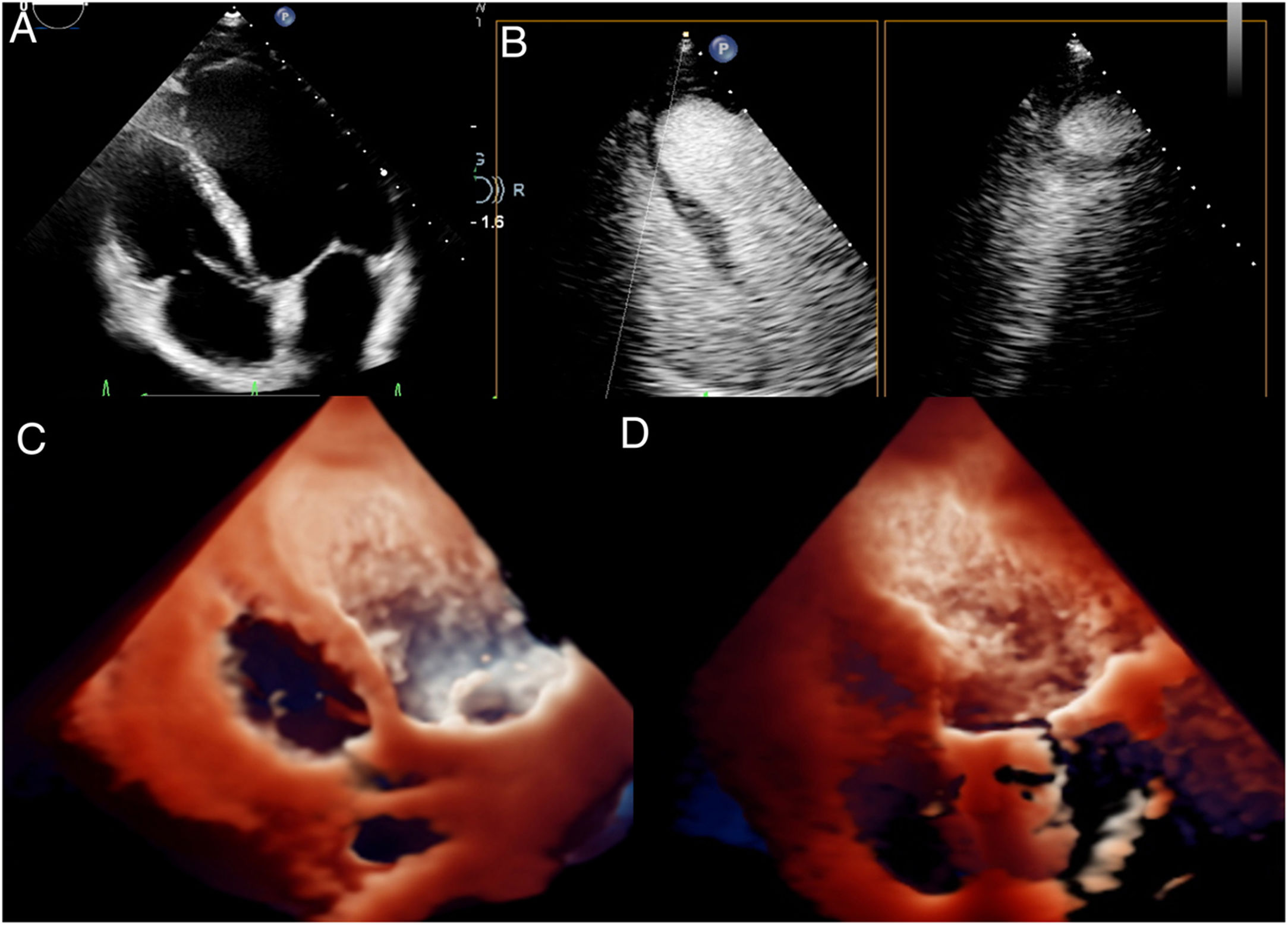
We report the case of a 57-year-old male with a history of a previous acute myocardial infarction (AMI) in 2016. An emergency coronary angiography revealed thrombotic occlusion of the medial left anterior descending artery; therefore, a percutaneous coronary intervention (PCI) was performed with a pharmacoactive stent. A cardiac computed tomography scan (cardiac CT scan), performed 3 years later due to an episode of chest pain (Revolution™ CT 256 GE, Wisconsin, United States; Iopamiro® [Iopamidol] contrast 370mg/ml, 60ml at 5ml/s, cardiac synchronisation with prospective acquisition; BMI 20.8kg/m2; sinus rhythm 74 beats per minute), revealed a hypodense image measuring 44mm×23mm×23mm in the apex of the left ventricle (Fig. 1A and B). Given that a thrombus was suspected, the study was complemented the following day with cardiac magnetic resonance imaging (CMRI) with gadolinium (MRI 1.5T Signa 450W GE, Gadovist 0.15mmol/kg; FIESTA cine sequences: TR 3.6/TE 1.6, matrix 192×224, FOV 38, angle 65, slice thickness 8mm, NEX 1; first-pass perfusion sequences: T1-enhanced ultra-fast gradient echo with saturation pulse TR 2.7/TE 1.2, matrix 128×92, FOV 40, slice thickness 12mm, NEX 1; late enhancement sequences: gradient echo with inversion-recovery pulse TE 3.2/TE 6.9, matrix 224×192, FOV 38, slice thickness 8mm, NEX 1) (Fig. 2A–C). On the same day, the patient underwent a 2D transthoracic echocardiogram (TTE) with the echo-enhancing agent Sonovue® (Fig. 3B) and three-dimensional TTE in real time (Fig. 3C and D). This ruled out the need to administer anticoagulant therapy. Multimodal imaging confirmed the absence of a thrombus, since the entire left ventricular cavity was uniformly filled both in first-pass perfusion sequences and in late gadolinium enhancement sequences on CMRI (Fig. 2A–C) as well as on 2D TTE with an echo-enhancing agent (Fig. 3B, Video 1). Three-dimensional TTE in real time (Fig. 3C and D, Videos 2–4) with high-definition photo-realistic rendering (EPIQ CVX, TrueVue, Philips Healthcare, Andover, US), for its part, enabled better definition of the apical region, which contributed as a whole to the diagnosis of a “pseudothrombus” due to a flow artefact on CT, as a result of a slow flow rate in the ventricular akinetic region.
Cardiac magnetic resonance imaging. (A) 4-Chamber cine SSFP view. Apical aneurysmal dilation of the left ventricle. (B) Late gadolinium enhancement. Absence of thrombus at the apical level. Practically transmural subendocardial enhancement in the region of the previous infarct. (C) First-pass perfusion of gadolinium; short axis at the apical level of the left ventricle, defect of myocardial perfusion in the inferior segment, absence of ventricular thrombus.
Transthoracic echocardiogram (TTE). (A) 4-chamber 2D TTE, poor visualisation of the akinetic apical region. (B) TTE with echo-enhancing agent, multi-planar image simultaneously showing orthogonal planes over the region of the probable thrombus, revealing complete filling of the cavity (absence of a thrombus) with an echo-enhancing agent. (C) Three-dimensional TTE in real time with photo-realistic rendering. Light source towards the basal region of the left ventricle. (D) Three-dimensional TTE in real time with photo-realistic rendering. Light source towards the apical region of the left ventricle. Absence of a thrombus.
The formation of a left ventricular thrombus (LVT) generally occurs in the presence of AMI, dilated cardiomyopathy or ventricular aneurysm.1 Regarding ischaemic heart disease, a prevalence of LVT within 90 days after infarct of 4.3% has been observed in the postoperative PCI period.2 The following precipitating factors have been identified: depressed left ventricular ejection fraction, heart failure prior to AMI, high heart rate, previous AMI and higher levels of cardiac troponin at the time of the event.2
Flow artefacts and poor blood opacification may simulate the appearance of a thrombus in vascular structures in CT scans, such as the well-known phenomenon in the inferior vena cava1 or in the left auricle3,4; however, their prevalence in the left ventricle has scarcely been documented.1,3 Patients with a ventricular thrombus are at higher risk of systemic embolism and are generally treated by means of anticoagulation therapy in the absence of a contraindication. Patients with a false positive diagnosis may receive this therapy unnecessarily and increase their risk of bleeding with devastating consequences.
The appearance of a pseudothrombus on CT originates from incomplete filling with contrast in the ventricular cavity during the arterial phase, as has been recognised in the left auricle of some patients who have undergone these studies,3,4 where the false image of the thrombus is correlated with the presence of spontaneous echo contrast in slow-flow states.4 The recently developed three-dimensional echocardiography technology of high-definition photo-realistic rendering promotes three-dimensional visualisation of anatomical structures and enables changes of lighting conditions in imaging, thus improving our perception of anatomical depth.5 To our knowledge, this is the first instance in the literature of the use of three-dimensional echocardiography with TrueVue photo-realistic rendering technology to rule out the presence of a thrombus. Our case confirmed the importance of making use of multimodality in cardiac imaging in this type of patient. Cardiac imaging techniques such as TTE with an echo-enhancing agent and three-dimensional TTE; sequences based on injection of gadolinium in CMRI such as first-pass perfusion, inversion-recovery in early enhancement with a very prolonged inversion time6 and late enhancement; and CT in the arterial phase and the late venous phase (60s following injection of iodinated contrast)4 will enable the clinician to distinguish a pseudothrombus from a true ventricular thrombus and the patient to benefit from the major therapeutic and prognostic implications that correct diagnosis of this condition entails.
Conflict of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Urmeneta Ulloa J, Álvarez Vázquez A, Martínez de Vega V, Cabrera JÁ. Pseudotrombo en ventrículo izquierdo. “Imagen fantasma” en tomografía axial computarizada. Diagnóstico multimodalidad. Radiología. 2020. https://doi.org/10.1016/j.rx.2020.01.004