To analyse the impact of a multidisciplinary training programme in magnetic resonance imaging (MRI) for axial spondyloarthritis in daily clinical practice.
MethodsAfter two years of training workshops for radiologists and rheumatologists, we designed a survey to assess changes in: (1) communication and collaboration between departments; (2) radiologists’ interest and keeping up to date in axial spondyloarthritis and rheumatologists’ training in MRI; (3) number of MRI studies done; (4) availability of protocols about technical requirements for studying axial spondyloarthritis by MRI and of standardised reporting templates; (5) evaluation and management of axial spondyloarthritis; (6) areas of improvement.
ResultsAfter 50 workshops, 96 rheumatologists and 51 radiologists completed the survey.
ConclusionsAmong radiologists and rheumatologists, multidisciplinary training in MRI for axial spondyloarthritis seems to have a positive influence on teamwork as well as on the management and evaluation of patients with axial spondyloarthritis.
Analizar el impacto en la práctica diaria tras una formación multidisciplinar en resonancia magnética (RM) en espondiloartritis (EspA) axial.
MétodosTras 2 años de talleres formativos para radiólogos y reumatólogos, se diseñó una encuesta para evaluar los cambios en: comunicación y colaboración entre servicios; interés y actualización de radiólogos en EspA axial y formación en RM entre los reumatólogos; número de RM realizadas; disposición de protocolos sobre requerimientos técnicos para el estudio por RM en EspA axial e informes estandarizados; evaluación y manejo de la EspA axial, y áreas de mejora.
ResultadosTras la realización de 50 talleres, contestaron la encuesta 96 reumatólogos y 51 radiólogos.
ConclusionesLa formación multidisciplinar en RM en EspA axial entre radiólogos y reumatólogos parece influir positivamente en el trabajo conjunto, manejo y evaluación de los pacientes con EspA axial.
Spondyloarthritis (SpA) consists of a heterogeneous group of diseases that are very prevalent in the general population. In Spain, its prevalence is estimated at 0.1–2.5%.1,2 For a considerable number of patients, it is a debilitating disease causing deterioration of their functional capacity and quality of life; therefore, it has significant social and healthcare-related implications.3–5 Therefore, early diagnosis and treatment are essential.
In this regard, the new criteria for classification of forms of SpA, which distinguish axial from peripheral forms, have been a very important milestone.6,7 One of the major new features of these criteria is the addition of magnetic resonance imaging (MRI) of sacroiliac joints. Its use has represented a major advance in early detection of axial inflammatory lesions, which for its part has led to a shortening of the diagnostic delay of axial SpA from 8.58 to 2 years.9 In addition, MRI allows for detecting complications, making a differential diagnosis, monitoring and even predicting treatment response in both spinal and sacroiliac disease.
Therefore, it is essential to join forces and gain a deeper knowledge of MRI in patients with axial SpA. To this end, the PROGRESSES project was started. In this project, radiologists and rheumatologists collaborated for three years through training workshops to increase knowledge among radiologists of this disease and knowledge among rheumatologists of MRI use. They also sought to achieve good communication and relationships between these two specialisms for multidisciplinary management of SpA as currently recommended by the T2T guidelines.10
MethodologyPROGRESSES project (training programme in MRI in axial SpA). This is a project sponsored by the Grupo para el estudio de la Espondiloartritis, de la Sociedad Española de Reumatología [Group for the Study of Spondyloarthritis of the Spanish Association of Rheumatology] (GRESSER) and by the Sociedad Española de Radiología Musculoesquelética [Spanish Association of Musculoskeletal Radiology] (SERME) in order to: (a) improve knowledge of axial SpA and MRI use in cases thereof and (b) promote collaboration between rheumatologists and radiologists. Part of this project consisted of theoretical and practical workshops, held on an annual basis for the last three years (26 the first year, 24 the second and third years) throughout Spain. The workshops were given by a rheumatologist and a radiologist who were experts in SpA and MRI from the same hospital to a group of rheumatologists and radiologists who attended based on geographic proximity in different areas on a national level.
Survey. A survey was designed to evaluate effects and possible changes in clinical practice following two years of workshops. This survey (in paper format) was filled in by all participants (rheumatologists and radiologists) during the workshops in the 3rd year of the project.
The survey included the following questions: (1) In the last year, has communication with your rheumatology/radiology department seemed easier, more agile and more efficient? (answer from 1 to 5 where 1 is not at all easy, agile or efficient and 5 is very easy, agile and efficient). (2) Changes in levels of interest and up-to-dateness among radiologists in SpA (Assessment of SpondyloArthritis International Society [ASAS] criteria, recommendations, etc.) and in levels of MRI training among rheumatologists (sequences, slices, types of lesion, differential diagnosis, etc.) (answer yes, no, doesn’t know/no answer). (3) Changes in the number of axial (spinal and sacroiliac) MRIs to study patients with SpA (answer yes, no, doesn’t know/no answer). (4) Availability of a protocol on technical requirements for the MRI study of SpA (answer yes, no, doesn’t know/no answer). (5) If the previous answer was yes, whether the protocol pre-dated the PROGRESSES project (answer yes, no, doesn’t know/no answer). (6) Availability of standardised reports that enable the rheumatologist to properly interpret a patient's MRI (answer yes, no, doesn’t know/no answer). (7) Outsourcing of MRI to centres outside of the hospital (answer yes, no, doesn’t know/no answer). (8) Whether the PROGRESSES project has had a positive impact on the management and evaluation of patients with SpA (answer yes, no, doesn’t know/no answer). (9) Aspects of their clinical practice to which MRI contributes most in SpA (differential diagnosis, early diagnosis, evaluation, activity, clinical prognosis, prediction of treatment response, treatment monitoring). (10) Whether the PROGRESSES project has improved and promoted multidisciplinary rheumatology/radiology work (answer yes, no, doesn’t know/no answer). (11) Whether there are still any barriers to the rheumatologist/radiologist relationship in cases of SpA (answer yes, no, doesn’t know/no answer). (12) How much more they can work on training in MRI in SpA to continue improving (answer from 1 to 10, where 1 is not at all and 10 is the maximum).
Statistical analysisA descriptive analysis of the data was performed.
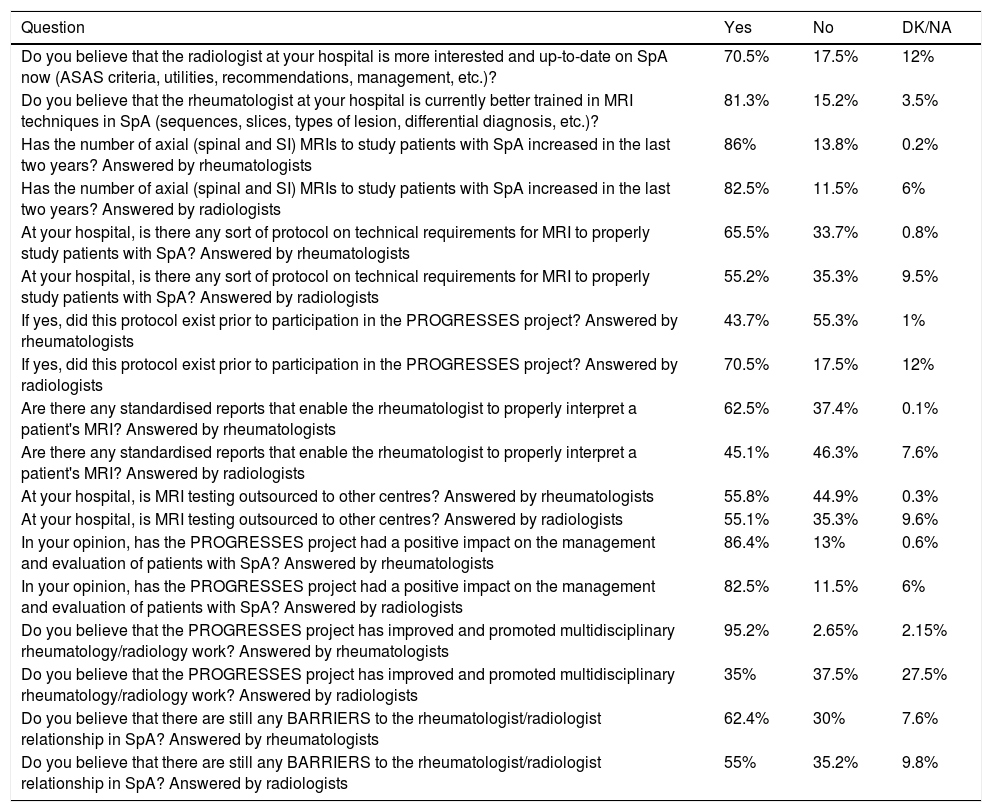
ResultsAltogether, 147 participants — 96 rheumatologists and 51 radiologists — filled in the survey. The main results are described below (see also Table 1).
Survey resultsa
| Question | Yes | No | DK/NA |
|---|---|---|---|
| Do you believe that the radiologist at your hospital is more interested and up-to-date on SpA now (ASAS criteria, utilities, recommendations, management, etc.)? | 70.5% | 17.5% | 12% |
| Do you believe that the rheumatologist at your hospital is currently better trained in MRI techniques in SpA (sequences, slices, types of lesion, differential diagnosis, etc.)? | 81.3% | 15.2% | 3.5% |
| Has the number of axial (spinal and SI) MRIs to study patients with SpA increased in the last two years? Answered by rheumatologists | 86% | 13.8% | 0.2% |
| Has the number of axial (spinal and SI) MRIs to study patients with SpA increased in the last two years? Answered by radiologists | 82.5% | 11.5% | 6% |
| At your hospital, is there any sort of protocol on technical requirements for MRI to properly study patients with SpA? Answered by rheumatologists | 65.5% | 33.7% | 0.8% |
| At your hospital, is there any sort of protocol on technical requirements for MRI to properly study patients with SpA? Answered by radiologists | 55.2% | 35.3% | 9.5% |
| If yes, did this protocol exist prior to participation in the PROGRESSES project? Answered by rheumatologists | 43.7% | 55.3% | 1% |
| If yes, did this protocol exist prior to participation in the PROGRESSES project? Answered by radiologists | 70.5% | 17.5% | 12% |
| Are there any standardised reports that enable the rheumatologist to properly interpret a patient's MRI? Answered by rheumatologists | 62.5% | 37.4% | 0.1% |
| Are there any standardised reports that enable the rheumatologist to properly interpret a patient's MRI? Answered by radiologists | 45.1% | 46.3% | 7.6% |
| At your hospital, is MRI testing outsourced to other centres? Answered by rheumatologists | 55.8% | 44.9% | 0.3% |
| At your hospital, is MRI testing outsourced to other centres? Answered by radiologists | 55.1% | 35.3% | 9.6% |
| In your opinion, has the PROGRESSES project had a positive impact on the management and evaluation of patients with SpA? Answered by rheumatologists | 86.4% | 13% | 0.6% |
| In your opinion, has the PROGRESSES project had a positive impact on the management and evaluation of patients with SpA? Answered by radiologists | 82.5% | 11.5% | 6% |
| Do you believe that the PROGRESSES project has improved and promoted multidisciplinary rheumatology/radiology work? Answered by rheumatologists | 95.2% | 2.65% | 2.15% |
| Do you believe that the PROGRESSES project has improved and promoted multidisciplinary rheumatology/radiology work? Answered by radiologists | 35% | 37.5% | 27.5% |
| Do you believe that there are still any BARRIERS to the rheumatologist/radiologist relationship in SpA? Answered by rheumatologists | 62.4% | 30% | 7.6% |
| Do you believe that there are still any BARRIERS to the rheumatologist/radiologist relationship in SpA? Answered by radiologists | 55% | 35.2% | 9.8% |
Regarding changes in communication between departments in the last year, more than 50% of those surveyed believed that it had distinctly improved. This was clear both among rheumatologists (mean 4.25) and among radiologists (mean 3.82). In addition, a large percentage of rheumatologists (70.5%) believed that the radiologists at their hospital had become more interested and up-to-date on SpA, and 72% believed that they were more involved in the importance of early detection of SpA. Similarly, 81.3% of radiologists thought that the level of MRI training among rheumatologists had improved, and a very similar percentage believed that rheumatologists had come to contribute more and better information in orders for MRIs to study a patient with SpA.
In addition, more than 80% of rheumatologists and radiologists answered that larger numbers of axial MRIs had been performed to study patients with SpA in the last two years.
Regarding the availability of a protocol on technical requirements for the MRI study of SpA, percentages of affirmative answers were 65.5% among rheumatologists and 55.2% among radiologists, respectively. Interestingly, among centres with such a protocol, more than 50% of rheumatologists and somewhat more than 70% of radiologists reported that it was already in place at their centres prior to the project. In the same vein, only about 50% of participants reported that there were standardised reports that enabled the rheumatologist to properly interpret a patient's MRI.
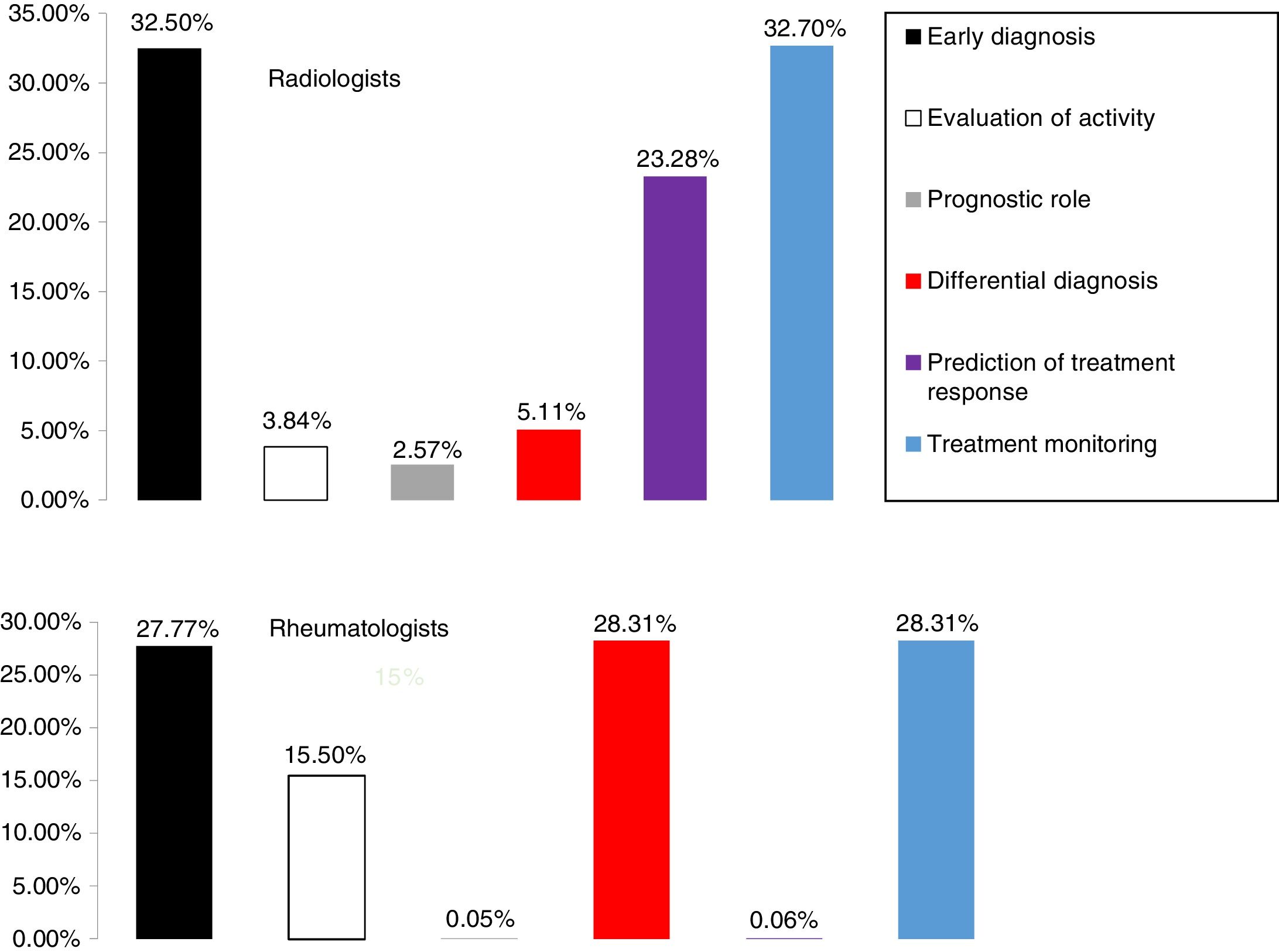
We found that 55% of centres outsource MRIs, and that most participants (more than 80%) believe that the PROGRESSES project has had a positive impact on the management and evaluation of patients with SpA. Concerning aspects of clinical practice to which MRI may contribute most in this disease (Fig. 1), for rheumatologists they would be differential diagnosis, early diagnosis and treatment monitoring, and for radiologists they would be early diagnosis, prediction of treatment response and treatment monitoring.
Among 95% of rheumatologists and among 62% of radiologists is a belief that the PROGRESSES project has improved and promoted multidisciplinary rheumatology/radiology work. However, when asked whether there were still any barriers in the rheumatologist/radiologist relationship, 62.4% of rheumatologists and 55% of radiologists answered yes. Furthermore, when asked to offer their opinion on whether they can work more (maximum score of 10) on training in MRI in SpA to continue improving, rheumatologists’ answers averaged 7.65 and radiologists’ answers averaged 8.53.
DiscussionIn this study, we analysed the results of a survey designed to evaluate changes following two years of multidisciplinary (rheumatology/radiology) theoretical and practical training workshops in MRI in axial SpA throughout Spain. We also identified possible areas for improvement.
First, it should be noted that, following 50 workshops, many participants perceived positive changes in communication and collaboration between departments, as well as greater interest in SpA among radiologists and in the level of MRI training among rheumatologists. A multidisciplinary approach is strongly recommended in national and international guidelines and consensuses1,10,11 and has proven to be highly beneficial for all.12 Curiously, a larger percentage of rheumatologists than radiologists believed that the PROGRESSES project had improved and promoted multidisciplinary work. Since MRI is still a service that the radiologist provides for the rheumatologist, the establishment of new pathways for communication may be more beneficial to the latter. These changes have manifested on a practical level in the form of increased numbers of MRI studies in axial SpA as well as better patient evaluation and management. The emAR II study, conducted in 2010, revealed that less than 20% of patients with axial SpA had had an MRI in the last two years in Spain,13 as opposed to other European cohorts where the percentage of patients who had had an MRI was significantly higher.14
However, other areas in which more work is needed have been detected. There is a need for greater implementation of protocols on technical requirements for the MRI study of SpA. There is also a need for standardised MRI reports that enable the rheumatologist to interpret them properly. Finally, more than half of patients believed that there were still barriers to the relationship between specialists.
One of the main limitations of this study is that it is an opinion survey. However, we believe that the high rate of participation of specialists (rheumatologists and radiologists) after several years of workshops means that these results may reflect positive changes in day-to-day clinical practice. In any case, more studies which demonstrate that these workshops lead to better health outcomes in patients with SpA are needed.
FundingThe PROGRESSES project was funded by AbbVie.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Almodóvar R, Zarco P, Loza E, Bueno Á. Evaluación de un programa de formación multidisciplinar en resonancia magnética en espondiloartritis axial: Proyecto PROGRESSES. Radiología. 2019;61:94–98.