We present a case of a female patient with ovarian cancer who had an inadvertent vascular access device implantation in the subclavian artery, being detected after 10 days. She was successfully treated with a covered stent without immediate complications.
Presentamos el caso de una paciente afectada de neoplasia de ovario a quien se le colocó inadvertidamente un reservorio venoso central en la arteria subclavia, que fue detectado 10 días después. Fue tratada con éxito mediante la colocación de un stent recubierto, sin presentar complicaciones inmediatas.
Implantable venous access systems are a major boon for oncology patients requiring repeated venepuncture. Placement of a central venous catheter (CVC) is performed by surgeons or interventional radiologists through one or two incisions. The procedure has a learning curve and is not free from complications. Their incidence varies depending on whether access is created through the subclavian or internal jugular vein (5% vs 1.5%),1 but decreases if the technique is done under ultrasound guidance.2 Potential complications include pneumothorax, haemothorax, arrhythmias, catheter malposition and artery damage. Accidental arterial puncture may cause haematoma, haemothorax, thrombosis and pseudoaneurysm.
We report a case of inadvertent improper placement of a CVC in the subclavian artery, detected after 10 days and treated by means of an arterial stent.
Case reportWe present the case of a 55-year-old patient with a body mass index (BMI) of 33kg/sq m and a history of ovarian neoplasia requiring placement of a CVC to start chemotherapy. An 8.5-Fr CVC (Celsite® ST301 B.Braun Medical, Melsungen, Germany) was placed in an outpatient procedure under sedation. The procedure was performed by a general surgeon with perioperative radioscopic guidance, and a chest X-ray was subsequently taken. The patient was discharged and referred to the oncology department.
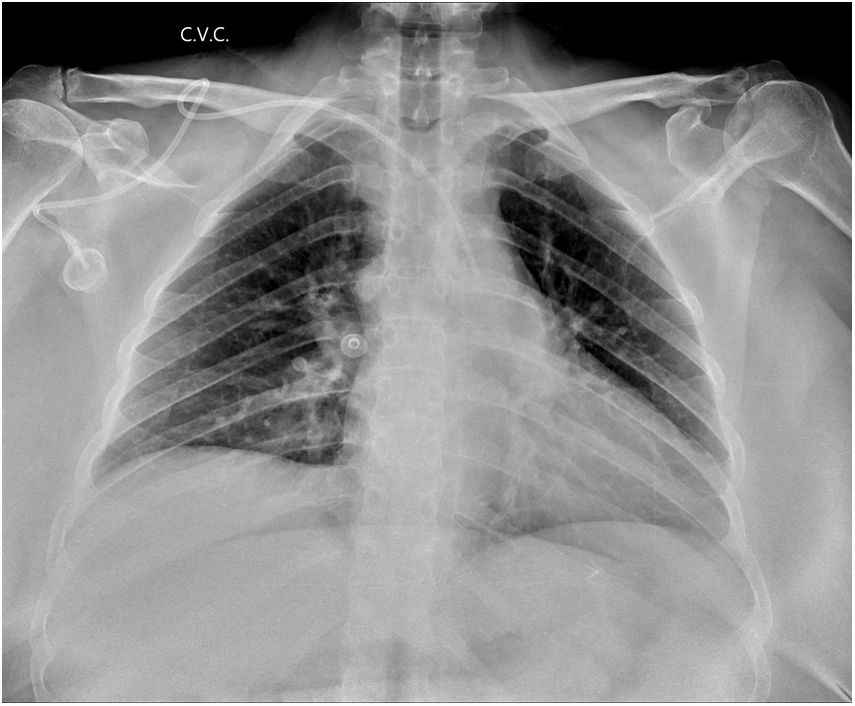
The oncology nursing team suspected that the CVC was placed in the artery when they manipulated it for the first time 10 days later and observed outflow of pulsatile arterial blood following chamber puncture. The malposition of the device was confirmed following a review of the X-ray taken following the initial procedure, which revealed that the chamber was located in the axillary area, the catheter pathway had a loop and the distal end was located in the aortic arch. (Fig. 1). A physical examination of the patient showed a single incision and the axillary placement of the chamber.
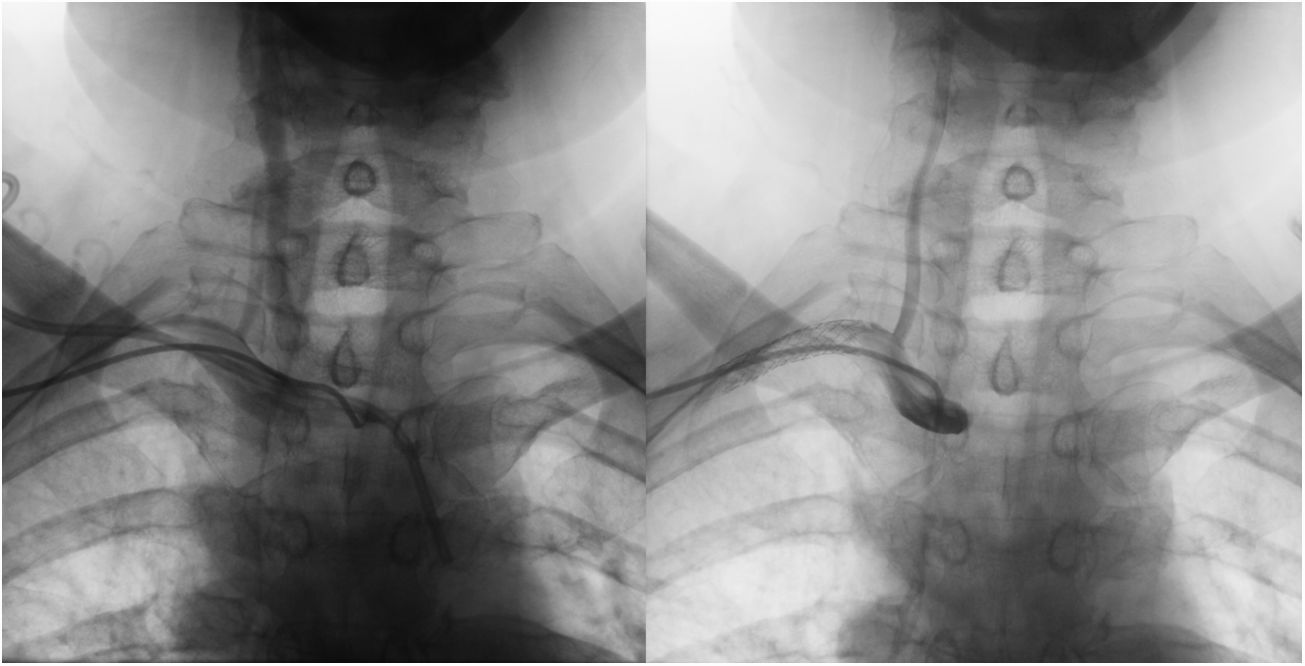
A multidisciplinary team assessed the case and decided on management by interventional radiology. The right humeral artery was punctured and an 8-Fr catheter was inserted to perform arterial catheterisation and angiographic monitoring. The point of entry into the right subclavian artery was located and its location in relation to the ipsilateral vertebral and carotid arteries was assessed (Fig. 2A). A BeGraft Bentley® balloon-expandable coated stent (BeGraft, Bentley, Hechingen, Germany) measuring 10mm in diameter and 37mm in length was implanted. The stent was expanded when the arterial catheter was removed from the CVC, and the proximal end was located 1cm from the origin of the vertebral artery. Angiographic monitoring showed no leaks and indicated that the stent was ultimately properly implanted (Fig. 2B).
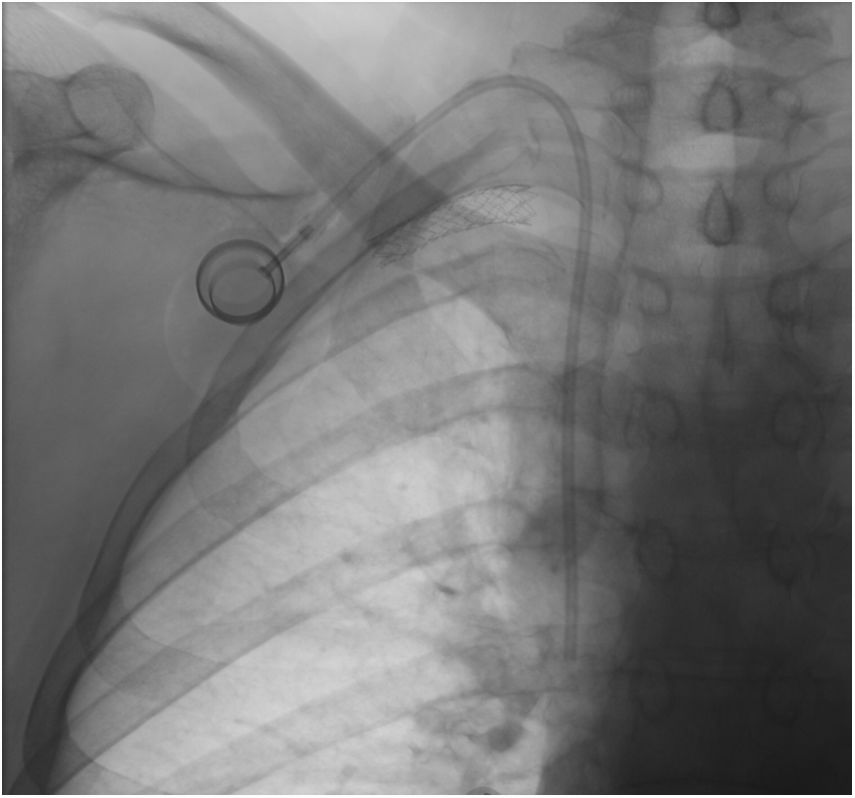
A new 8.5-Fr CVC (Celsite® ST301 B.Braun Medical, Melsungen, Germany) was placed in the ipsilateral side via the internal jugular route, with the chamber located in the subclavicular area (Fig. 3). The patient did not present any neurological deficits or vascular complications in her upper limbs, and was discharged after 24h on dual antiplatelet treatment with clopidogrel and acetylsalicylic acid.
DiscussionComplications following central venous catheter placement are widely reported in the scientific literature, as is the basis for its proper placement.3 Many studies have shown higher success rates and fewer immediate complications with ultrasound guidance,2 this technique presenting a lower incidence of arterial puncture compared to blind insertion. Accidental arterial puncture occurs in around 4.2–9.3% of cases. It is detected by outflow of arterial blood, which is difficult to recognise in patients in critical condition and patients with hypotension.4 This incident usually does not cause major complications, and local compression is the most common treatment. However, accidental arterial cannulation using Seldinger’s technique is rarely reported in the scientific literature5 and entails greater morbidity. Its complications include cervical–thoracic haematoma which may compromise the airway, haemothorax, pseudoaneurysm, arteriovenous fistula and cerebrovascular accident. Reportedly influential risk factors include obesity (BMI>30kg/sq m), multiple attempts at puncture and lack of experience on the part of the person performing the puncture.6 There are no guidelines to indicate ideal management to treat these cases, though algorithms for action have been proposed.7
Different treatment options have been reported. Simply removing the catheter and applying external compression may entail more complications; therefore, these actions are contraindicated in 7-Fr catheters and those of a greater diameter. These complications include uncontrollable bleeding, pseudoaneurysm and arteriovenous fistula. The recommended action would be leaving the catheter in situ and repairing it early, since this entails less morbidity and mortality.7 Endovascular techniques, such as occlusion balloons, percutaneous sealant systems (Angio-Seal®) and stents have been reported in the literature to be effective, and surgical treatment is currently limited to specific cases.
Temporary balloon tamponade is an alternative and effective technique for managing these lesions.8 A case similar to our own, though detected during the procedure, was successfully resolved by means of an occlusion balloon system.9
The Angio-Seal® sealing system (St. Jude Medical, St. Paul, Minnesota, USA), normally used for femoral artery puncture, has been reported to be successful in cases with catheter persistence.5,10 The system is a haemostatic device that seals the puncture site, thereby enabling the intra-arterial catheter to be removed. Its mechanism of action consists of the compression effect caused by an absorbable anchor in the lumen of the artery and an external collagen sponge, with the site of arterial puncture between the two. We ruled out this option given the lengthy distance between the start of the catheter and the point of entry into the artery, as well as the winding pathway.
Another endovascular option is treatment with a coated stent which has been used with success in several documented cases.6
Few cases have been reported in the literature, but reviews indicate that the selected technique is based on several factors: the patient’s clinical status, time since lesion onset, catheter persistence or lack thereof, catheter size and exact location of the point of entry into the artery. The choice of treatment is made on a case-by-case basis.
In our case, the patient was asymptomatic and the CVC had been implanted for 10 days; hence we were able to pursue a planned strategy and take a multidisciplinary approach. The time having elapsed, the long and winding subcutaneous pathway of the catheter, the point of entry into the artery in relation to the vertebral artery and the size of the catheter (8.5 Fr) led us to decide on endoluminal treatment with a coated stent. The patient started treatment with the new CVC functioning properly, and subsequent clinical monitoring continued not to show any neurological deficits or abnormalities in the upper limbs.
Authorship- 1
Responsibility for study integrity: DCL, SMM, CROL, JMM.
- 2
Study conception: DCL, SMM, CROL, JMM.
- 3
Study design: DCL, SMM, CROL, JMM.
- 4
Data acquisition: DCL, SMM, CROL, JMM.
- 5
Data analysis and interpretation: DCL, SMM, CROL, JMM.
- 6
Statistical processing: Not applicable.
- 7
Literature search: DCL, SMM, CROL, JMM.
- 8
Drafting of manuscript: DCL, SMM, CROL, JMM.
- 9
Critical review of manuscript: DCL, SMM, CROL, JMM.
- 10
Approval of final version: DCL, SMM, CROL, JMM.
The authors declare that they have no conflicts of interest.
Please cite this article as: Coroleu Lletget D, Mechó Meca S, Rodríguez-Otero Luppi C, Muchart Masaller J. Detección y manejo de implantación inadecuada de reservorio venoso central en arteria subclavia. Radiología. 2019;61:509–512.