Crohn's disease is an autoimmune disease that predominantly affects the gastrointestinal tract. Crohn's disease is diagnosed at a young age and runs a chronic course with acute flare-ups. When patients with Crohn's disease present with flare-ups at the emergency department, they are usually managed in a way similar to patients with acute abdomen; there is no consensus about the most appropriate imaging work-up for patients with flare-ups of Crohn's disease. Thus, we decided to review the literature about the imaging tests indicated (whether related to their diagnostic performance or to lower exposure to ionizing radiation) for acute flare-ups in patients with Crohn's disease.
La enfermedad de Crohn es una patología de etiología autoinmunitaria, con afectación predominante del aparato digestivo. Se trata de una enfermedad que se diagnostica a edad temprana y presenta un curso crónico con reagudizaciones. Estos brotes se suelen manejar de forma similar a un abdomen agudo en los pacientes que acuden a los servicios de urgencias, y no existe un consenso sobre cuáles serían las pruebas de imagen más adecuadas. Debido a esta controversia, se ha decidido realizar una revisión de la bibliografía actual sobre cuáles serían las pruebas de imagen indicadas (ya sea por rendimiento diagnóstico o por menor exposición a radiación ionizante) en el brote agudo de pacientes con enfermedad de Crohn.
Crohn's disease (CD) is an inflammatory bowel disease of autoimmune aetiology which, although predominantly affecting the gastrointestinal system, also has systemic involvement. The most common signs and symptoms are abdominal pain and an increase in the daily number of liquid stools. Patients may also suffer from weight loss, analytical alterations (anaemia, iron deficiency, abnormal liver function tests), rectal bleeding and more serious complications, such as fistulas, strictures and intestinal obstructions, perforations and abscesses. There can also be a variety of extraintestinal manifestations, including rheumatological, dermatological and ophthalmic.1
The incidence is 3.1–20.2 cases per 100,000 person-years. The fact that CD tends to be diagnosed at an early age and follows a chronic course with complications (30–50%) means these patients have frequent visits to emergency departments.2,3 The management of abdominal complications, mainly abscesses, fistulas and strictures with intestinal obstructions, is similar to acute abdomen in patients without CD, with everything that it implies in terms of diagnosis, plain X-rays, ultrasound (US) and computed tomography (CT).
In CD, this clinical scenario means that patients can receive very high cumulative doses of radiation. It is therefore necessary to consider which tests involve the lowest levels of ionising radiation but provide the best diagnostic accuracy to ensure proper management of CD in the emergency department.
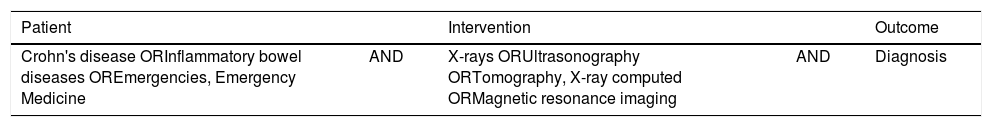
Clinical questionWe formulated the clinical question following the Patient-Intervention-Outcome (PIO) strategy: What imaging tests should be performed in a patient with a flare-up of Crohn's disease who comes to the emergency department with abdominal pain (Table 1)?
Clinical question according to the PIO strategy.
| Patient | Intervention | Outcome | ||
|---|---|---|---|---|
| Crohn's disease ORInflammatory bowel diseases OREmergencies, Emergency Medicine | AND | X-rays ORUltrasonography ORTomography, X-ray computed ORMagnetic resonance imaging | AND | Diagnosis |
PIO: Patient-Intervention-Outcome.
From March to August 2017, we carried out an efficient search following the Haynes pyramid4 on the radiological management of acute flare-ups in CD with the terms specified in Table 1.
Using MeSH terms and free terms, we consulted the meta-search engine ACCESSSS5 and obtained literature references in abstract form (UpToDate and DynaMed).1–3 We also searched databases, such as PubMed and Trip Database, finding clinical practice guidelines (European Crohn's and Colitis Organisation-European Society of Gastrointestinal and Abdominal Radiology [ECCO-ESGAR])6–8 and guidelines on appropriateness (American College of Radiology [ACR]),9 and carried out a systematic review.10 A total of 133 documents were obtained, but we found no management algorithms with sufficient scientific evidence. In November 2018 the search was updated using the same terms, but we still found no relevant references.
We analysed the publications which were of use for the PIO question and presented the highest level of evidence: the systematic review,10 the ECCO-ESGAR clinical practice guidelines6–8 and the ACR Appropriateness Criteria.9
Critical reading- 1.
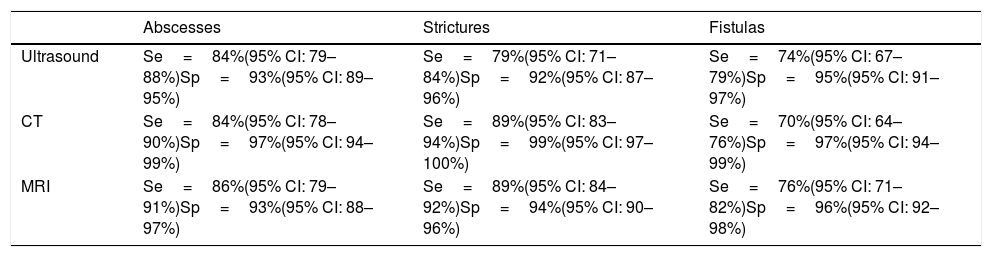
In 2011, Panés et al.10 published a systematic review covering from 1994 to 2010 and including a final selection of 68 articles; levels of evidence (LE) and grade of recommendation (GR) were generated according to the criteria agreed by the Oxford Centre for Evidence-Based Medicine. In the section on diagnosis of complications, they analysed the US, CT and magnetic resonance imaging (MRI) studies carried out to detect fistulas, abscesses and strictures. For the diagnosis of fistulas they concluded that the three techniques had high sensitivity (Se) (US 74%, CT 70%, MRI 76%) and specificity (Sp) (US 95%, CT 97%, MRI 96%), with similar diagnostic accuracy (LE-2, GR-B). Se and Sp were also high for the techniques used to detect abscesses (US: Se 84%, Sp 93%; CT: Se 84%, Sp 97%; and MRI: Se 86%, Sp 93%), with CT and MRI showing greater diagnostic accuracy (LE-2, GR-B). Last of all, to identify areas of stricture, they reported that all three techniques showed high Se (US 79%, CT 89%, MRI 89%) and Sp (US 92%, CT 99%, MRI 94%) with similar diagnostic accuracy. These data are shown in Table 2.
Table 2.Diagnostic accuracy of imaging tests in complications of Crohn's disease.
Abscesses Strictures Fistulas Ultrasound Se=84%(95% CI: 79–88%)Sp=93%(95% CI: 89–95%) Se=79%(95% CI: 71–84%)Sp=92%(95% CI: 87–96%) Se=74%(95% CI: 67–79%)Sp=95%(95% CI: 91–97%) CT Se=84%(95% CI: 78–90%)Sp=97%(95% CI: 94–99%) Se=89%(95% CI: 83–94%)Sp=99%(95% CI: 97–100%) Se=70%(95% CI: 64–76%)Sp=97%(95% CI: 94–99%) MRI Se=86%(95% CI: 79–91%)Sp=93%(95% CI: 88–97%) Se=89%(95% CI: 84–92%)Sp=94%(95% CI: 90–96%) Se=76%(95% CI: 71–82%)Sp=96%(95% CI: 92–98%) CI: confidence interval; CT: computed tomography; MRI: magnetic resonance imaging; Se: sensitivity; Sp: specificity.
Source: Panés et al.10
- 2.
The evidence-based consensus guidelines developed by ECCO and ESGAR published in 20136 establish a series of conclusions on each of the techniques and their use in the diagnosis of the most common intra-abdominal complications:
- •
US, CT and MRI have high Se and Sp (>80%) for the diagnosis of strictures affecting the small intestine. The diagnostic accuracy of MRI and CT is based on the use of intraluminal contrast (LE-2).
- •
The accuracy of each of the techniques depends on the type of inflammatory process and the severity (LE-1).
- •
Ultrasound, CT and MRI have high accuracy in the diagnosis of penetrating complications (fistula, abscess, etc.) (LE-1).
- •
For deep-penetrating fistulas, CT and MRI are preferable to ultrasound (LE-4).
- •
Abdominal US and plain abdominal X-ray should be considered in all patients with acute abdominal pain and established CD. CT should be considered in patients with suspected perforation and negative or inconclusive first-line tests (LE-2).
- •
- 3.
The ACR guide for CD9 presents a single clinical scenario in acute flare-up (leucocytosis, pyrexia, abdominal pain, etc.), for which they recommend as the most appropriate test (9/9) CT with enterography, followed by CT with intravenous contrast or MRI (8/9) and US (5/9).
According to the highest quality evidence currently available, the main conclusion after this review is that there are no significant differences between the techniques described (US, CT and MRI) for the diagnosis of the most common acute complications in CD.
The ACR9 guidelines establish different grades of recommendation, but only present one single clinical scenario in which to apply them, without specifying clinical suspicions (abscesses, fistulas or strictures) or degrees of severity.
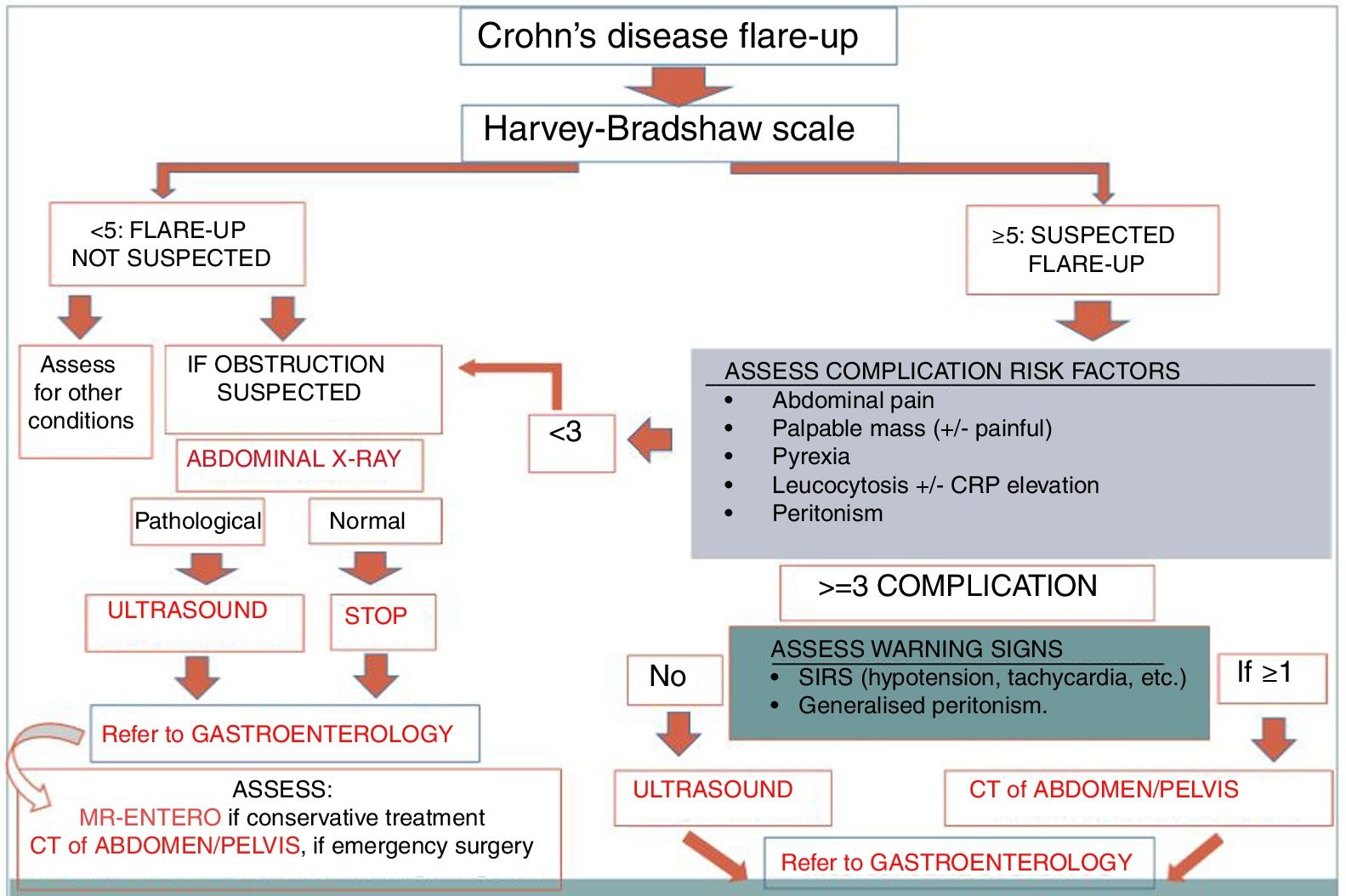
No validated algorithm was found for choosing the ideal imaging test. However, following our analysis of the literature, we, the investigators (radiologists, gastroenterologists, emergency and internal medicine specialists and methodologists), and the centres included in the MAPAC-Imagen II project (Mejora de la Adecuación de la Práctica Asistencial y Clínica en pruebas de Imagen [Improvement in the appropriateness of care provision and clinical practice in imaging tests]), have reached a panel of expert (Delphi type) consensus on a system of management based on clinical and analytical parameters, the Harvey-Bradshaw scale11 (numerical index of disease activity based on five variables, which are obtained quickly and easily by means of a brief medical history) and SIRS (systemic inflammatory response syndrome) parameters (Fig. 1).
The resulting algorithm, the level of evidence of which would be classed as “expert opinion”, is based mainly on the similar efficacy of the different diagnostic techniques (US, CT and MRI). Additionally, the stratification of severity according to clinical parameters only permits candidates for urgent surgical/interventional treatment to undergo a test with ionising radiation (CT). Other advantages are that practically all patients are assessed by imaging tests with high Se and Sp (US) and the initial plain abdominal X-ray is avoided in many patients.
Source of fundingMAPAC-IMAGEN II (Mejora de la Adecuación de la Práctica Asistencial y Clínica en pruebas de Imagen [Improvement in the appropriateness of care provision and clinical practice in imaging tests]) Working Group. This study received funding from the Instituto de Salud Carlos III [Carlos III Health Institute] (State Plan for R&D&i 2013–2016) Projects (P16/00296, PI16/01786, P16/01828, P16/00558) and it was co-financed by the European Regional Development Fund (ERDF), “A way to make Europe”.
Authorship- 1.
Responsible for the integrity of the study: PMG.
- 2.
Study conception: PMG and AVB.
- 3.
Study design: PMG and ALFLJ.
- 4.
Data acquisition: PMG.
- 5.
Analysis and interpretation of the data: PMG and AVB.
- 6.
Statistical processing: N/A.
- 7.
Literature search: PMG and ALFLJ.
- 8.
Drafting of the paper: PMG.
- 9.
Critical review of the manuscript with relevant intellectual contributions: PMG, AVB and ALFLJ.
- 10.
Approval of the final version: PMG and AVB.
The authors declare that they have no conflicts of interest.
Please cite this article as: Marazuela García P, López-Frías López-Jurado A, Vicente Bártulos A. Dolor abdominal agudo en la enfermedad de Crohn. ¿Qué prueba de imagen urgente se debe hacer? Radiología. 2019;61:333–336.