A 44-year-old woman, former smoker, underwent apical segmentectomy of the right lower lobe in 2015 for a typical carcinoid tumor (1.5cm, Ki 67<2%, T1aN0M0R1). In 2024, follow-up CT revealed a suspicious lesion, and PET scan confirmed a 13mm nodule (SUVmax 6). In January 2025, she had an extended right lower lobectomy with bronchoplasty. Weeks later, flexible bronchoscopy showed reduced bronchial lumen, partially visualizing the middle lobe bronchi (ML). Two months post-surgery, due to increasing dyspnea, an almost complete distal stenosis of the intermediate bronchus was discovered, preventing access to the ML. After unsuccessful balloon dilation and anatomical uncertainty, the procedure was stopped. CT with 3D reconstruction (Fujifilm Synapse 3D software) and virtual bronchoscopy navigation (VBN) was performed with this planner. Guided by VBN, biopsies and successful balloon dilation reopened the ML bronchial orifice. The case highlights the value of VBN and 3D reconstruction for planning and guiding complex endoscopic procedures.
Una mujer de 44 años, exfumadora, se sometió a una segmentectomía apical del lóbulo inferior derecho en 2015 por un tumor carcinoide típico (1,5cm, Ki 67 <2%, T1aN0M0R1). En 2024, una TC de seguimiento reveló una lesión sospechosa y una tomografía por emisión de positrones (PET) confirmó un nódulo de 13mm (SUVmax 6). En enero de 2025, se le realizó una lobectomía inferior derecha extendida con broncoplastia. Semanas después, una broncoscopia flexible mostró una reducción de la luz bronquial, visualizando parcialmente los bronquios del lóbulo medio (LM). Dos meses después de la cirugía, debido a un aumento de la disnea, se descubrió una estenosis distal casi completa del bronquio intermedio, lo que impedía el acceso al LM. Tras una dilatación con balón fallida y la incertidumbre anatómica, se detuvo el procedimiento. Se realizó una TC con reconstrucción 3D (software Fujifilm Synapse 3D) y navegación bronquial virtual (NBV) con este planificador. Guiadas por NBV, las biopsias y la dilatación con balón exitosa reabrieron el orificio bronquial de la LM. El caso destaca la utilidad de la NBV y la reconstrucción 3D para planificar y guiar procedimientos endoscópicos complejos.
Recurrent carcinoid disease is uncommon, and surgery may be offered on the same premise of perioperative risk and stage selection as primary surgery. Cases of regional recurrences have been noted up to and beyond 30 years from the original resection of the primary tumor.1 Other studies have reported recurrences>10 years from the initial resection. Sometimes, it is possible to treat local recurrences with further surgery.2
A 44-year-old woman, former smoker, in 2015 underwent apical segmentectomy of the right lower lobe with wedge bronchoplasty for a typical carcinoid measuring 1.5cm, Ki 67<2%, classified as T1aN0M0R1. In 2024, during follow-up thoracic surgery, a CT scan showed soft tissue density in the parenchyma of 53mm×21mm, with local recurrence not excluded.
PET scan showed a nodular area of 13mm in the axial plane with a SUVmax of 6. Based on these findings, in January 2025 she underwent an extended right lower lobectomy involving the hilar portion of the middle lobe and the posterior region of the right upper lobe, with a terminoterminal bronchoplasty between the intermediate and middle lobe (ML). Weeks later, an outpatient flexible bronchoscopy (FB) was performed, showing a reduction in the lumen of the intermediate bronchus (IB), but with the possibility of visualization of permeable lumens of the ML.
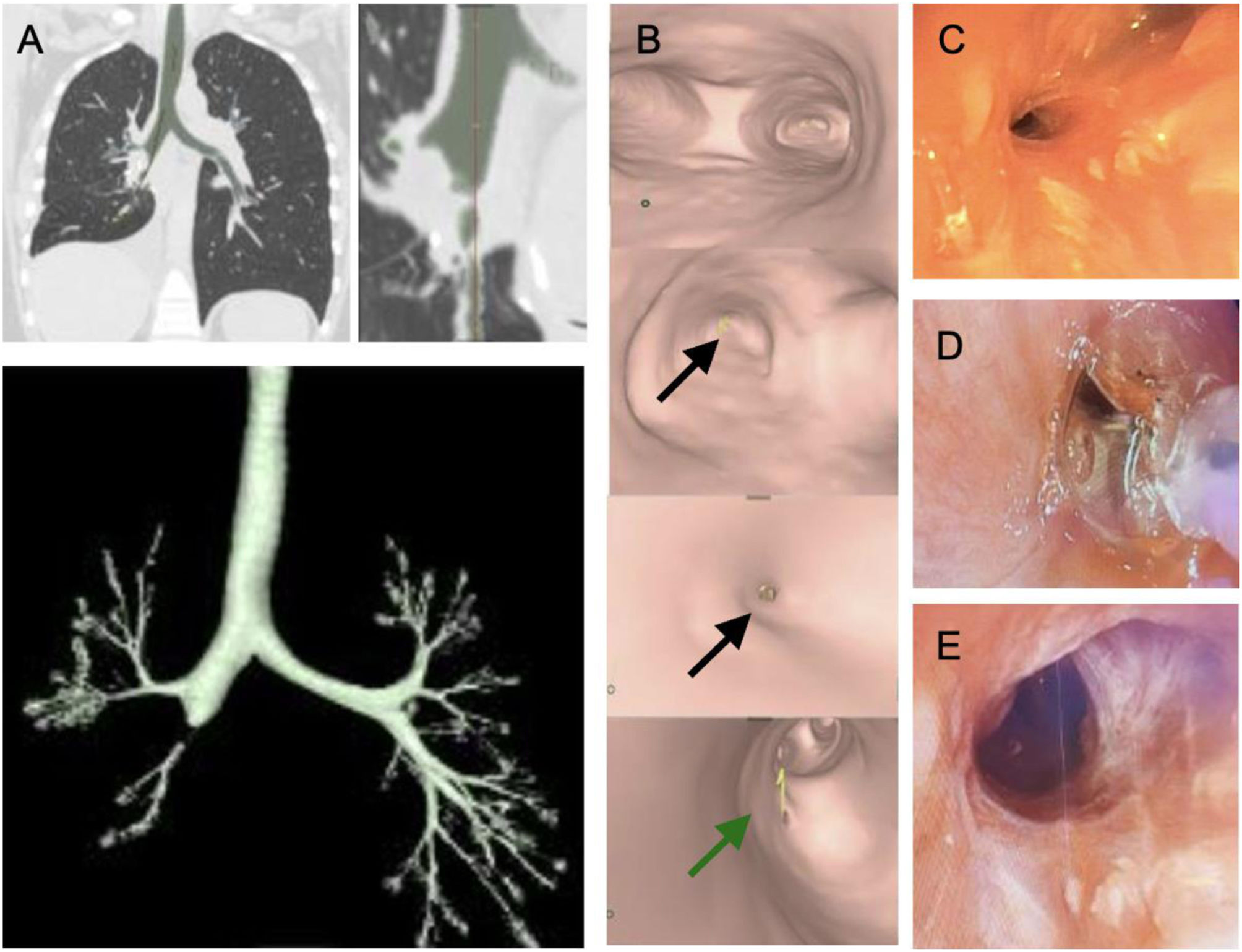
Two months after the surgery, a repeat bronchoscopy was requested due to an increase in dyspnea. It showed an almost complete stenosis in the most distal part of the IB, which prevented exploration of the ML bronchial orifices visible on the previous one. In the medial and distal wall of the IB, a millimeter sized orifice was observed surrounded by suture points which could not be traversed or visualized distally. A Fogarty 5Fr balloon was introduced to dilate the orifice, revealing another suture point inside, which prevented the passage of the bronchoscope. Saline was instilled through the orifice without distal permeability nor bubbles. An empirical guess was made as to the location of the ML ostium, but as there had been a previous segmentectomy, we wanted to confirm the distal lumen and avoid creating a false pathway. For that reason, given the uncertainty as to whether the lumen corresponded to the entry of the ML bronchi or a bronchial fistula, it was decided to terminate the procedure and to perform an urgent chest CT scan. After performing the CT scan, the images were reconstructed using Fujifilm Synapse 3D software (Fig. 1. A) from Fujifilm Healthcare and virtual bronchoscopy navigation (VBN) was performed using the pathway of the planner (Fig. 1B), showing airy middle lobe bronchial orifices. A new bronchoscopy was performed under Synapse 3D guidance. As the previous FB, a millimeter orifice in the medial and distal wall of the IB was found (Fig. 1C). With confidence and planning, biopsies were taken from the scarred lateral wall, which allowed the stenosis to open slightly enough to later advance the VATHIN 2.2mm bronchoscope and visualize distal openings free of stenosis. Therefore, a new entry was made with the Olympus TH1100 therapeutic bronchoscope and a bronchial guide was inserted through the stenosis followed by a high-pressure balloon (7.5F–2.5mm; 8–10mm). Three balloon dilatations are performed (Fig. 1D): First at 1atm for 30s; then at 2atm for 30s; 2.5atm for 30s; and finally at 3atm for 30s. An opening of at least 8mm of the stenosis is then observed, allowing visualization of free ML orifices (Fig. 1E).
VBN is a technique to improve the diagnostic performance of peripheral lung lesions.3 Synapse 3D is a strong software that provides a reconstruction good enough to understand the anatomy and calculate the dimensions of a stenosis. We show a case where VBN can also plan and localize the site of the recanalization ostium of a bronchial stenosis,4 allowing you to choose the most optimal treatment with a high degree of confidence.5 It is a powerful shaper that even if the reconstruction is good enough helps you calculate the dimensions of a stenosis and more accurately choose the stent to place. Even with certain features it can serve as a guide for certain pleural procedures such as ultrasound-guided transthoracic biopsies or for planning medical thoracoscopic in multiloculated compartments.
Artificial intelligence involvementNo use of IA has been used to elaborate this scientific letter.
Informed consentInformed consent was obtained from the patient for publication of the clinical data and images present in this manuscript. It was collected in the electronic medical record.
FundingThe authors declare that no funding was received for this article.
Authors’ contributionAll the authors of the article have contributed substantially to the elaboration of the manuscript.
Conflict of interestThe authors declare that they have no conflict of interest directly or indirectly related to the contents of this manuscript.
We would like to thank the Director of the Thoracic Area, Dr. Antoni Rosell Gratacós, and Dr. Carlos Martínez Bareyns for their contribution to the discussion and execution of this case.