Pleural empyema is a severe complication of pneumonia, tipically caused by Streptococcus pneumoniae or Staphylococcus aureus. We present a rare case of empyema due to Gemella morbillorum, an orophrarynx commensal. Risk factors include alcoholism, immunocompromised state, and poor oral hygiene. Its slow growth and resemblance to Streptococcus viridans complicate diagnosis, often requiring Matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF) mass spectrometry for accurate identification. While beta-lactams (penicilins and most cephalosporins) remain first-line therapy, our case highlights successful treatment in a penicillin-allergic patient using vancomycin and clindamycin, providing an alternative regimen. Other options, including macrolides, fluoroquinolones and tetracyclines, may be considered based on antimicrobial susceptibility testing. Optimal management combines pleural drainage and prolonged antibiotic therapy (≥4 weeks).
El empiema pleural es una complicación grave de la neumonía, causada con mayor frecuencia por microorganismos como Streptococcus pneumoniae o Staphilococcus aureus. En este caso clínico presentamos un caso poco frecuente de empiema debido a Gemella morbillorum. Gemella morbillorum, un microorganismo comensal de la orofaringe, es un patógeno poco común. Los factores de riesgo descritos incluyen alcoholismo, inmunosupresión e higiene bucal deficiente. A nivel del laboratorio, destaca la dificultad para su aislamiento y diagnóstico debido a su lento crecimiento y su parecido con Streptococcus Viridians que complica su identificación, requiriendo a menudo espectrometría de masas mediante MALDI-TOF para una identificación precisa. Mientras tanto, los antibióticos betalactámicos, incluyendo las penicilinas y mayoría de las cefalosporinas, constituyen el tratamiento de primera línea. Nuestro caso destaca el éxito en el tratamiento de nuestro paciente alérgico a los betalactámicos con el empleo de vancomicina y clindamicina. Otras opciones, incluyen macrólidos, fluoroquinolonas y tetraciclinas, dependiendo de la susceptibilidad del antibiograma. El manejo óptimo combina un drenaje pleural eficaz junto con una terapia antibiótica prolongada de más de 4 semanas.
Pleural empyema represents a severe complication of community-acquired pneumonia. While typically caused by Streptococcus pneumoniae, Staphylococcus aureus, or anaerobes, isolation of uncommon pathogens remains rare. We present a case of pleural empyema secondary to Gemella morbillorum, an exceptional finding in clinical practice.1
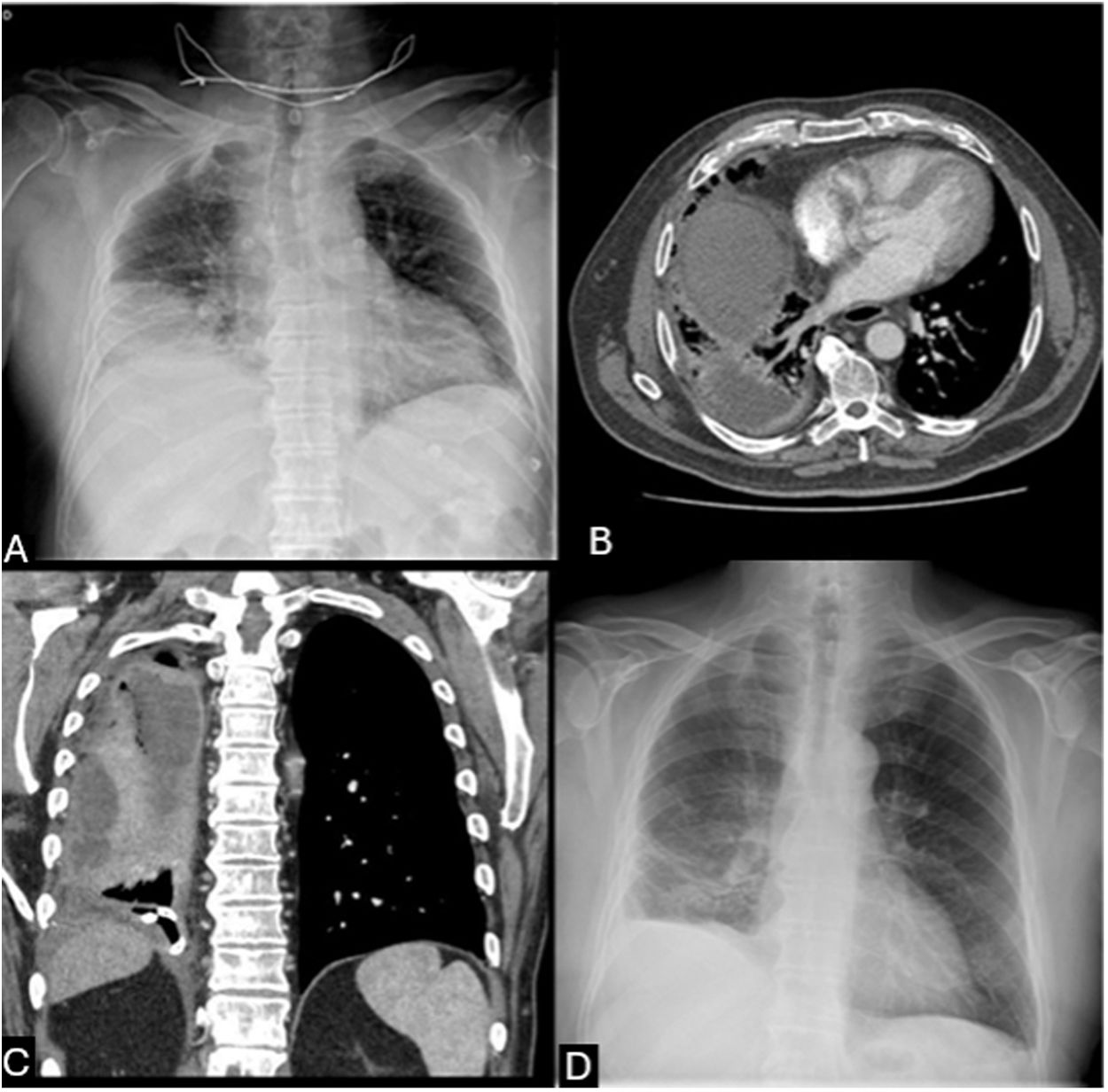
A 72-year-old male with chronic alcohol abuse, hypertension, dyslipidemia, and beta-lactam/streptomycin allergy presented with one week of fever, productive cough, and right-sided pleuritic pain. On admission, he manifested acute respiratory failure and chest X-ray revealed a right lower lobe consolidation (Fig. 1A).
(A) Chest X-ray showed a right lower lobe consolidation containing air foci and ipsilateral pleural effusion. (B) Chest CT scan showed a complex multiloculated pleural collection in the right hemithorax with septations and compressive atelectasis. (C) Coronal CT reconstruction confirming the loculated pleural collection in the right hemithorax. (D) Follow-up chest-X-ray at discharge documents complete resolution of pleural effusion, lung re-expansion and minimal residual basilar opacities in the right hemithorax.
Empirical levofloxacin therapy and high-flow oxygen support were initiated. Subsequent radiological deterioration (Fig. 1B and C) and ultrasound-guided thoracentesis yielded purulent pleural fluid, with matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF) mass spectrometry identifying G. morbillorum. A pig-tail catheter drained 4800ml, but loculations required intrapleural urokinase and a second drainage, which isolated Prevotella oris, confirming polymicrobial infection.
Given the patient's allergy and polymicrobial suspicion, levofloxacin was replaced with intravenous clindamycin and vancomycin for 14 days. This regimen addressed both Gemella (vancomycin), polymicrobial anaerobes coverage and synergistic activity against Gemella (clindamycin) demonstrating this antibiotic regimen combination as an effective alternative for beta-lactam-allergic patients. Subsequent step-down therapy consisted of a 6-week course of oral clindamycin and azithromycin. Also, multidisciplinary management with repeated drainage and fibrinolytics was critical, reflecting the need for aggressive source control in complex empyema. The patient achieved full clinical and pleural effusion resolution confirmed at discharge (Fig. 1D).
The Gemella genus comprises facultatively anaerobic, Gram-positive cocci first described in 1917.1,2 These organisms are commensals of the oropharynx, genitourinary and gastroinstestinal tract. Over 10 species have been identified, G. morbillorum and G. haemolysans are most frequently implicated as opportunistic pathogens in human infections.1–5 Clinical manifestations include endocarditis, bacteriemia, meningitis, abscess formation (pulmonary, cerebral and hepatic), mediastinitis, septic arthritis and empyemas.1,3,4
Although often considered of low pathogenicity, approximately 20 cases of pleural empyema due to G. morbillorum have been reported.2,3 Predisposing factors include alcoholism, diabetes, poor oral hygiene, and immunocompromised states.1–5 Microbiologically, their slow growth and similarity to Streptococcus viridans may complicate identification, hence techniques like MALDI-TOF mass spectrometry enhance diagnosis.1,3
G. morbillorum isolates typically demonstrate susceptibility to beta-lactam antibiotics, including penicillins and most cephalosporins, making these agents first-line therapy. For severe infections (e.g., endocarditis, bacteriemia), synergistic combination therapy with beta-lactam and aminoglycoside is recommended.1,4,5
In penicillin-allergic patients, vancomycin serves as an effective alternative due to consistent susceptibility. Clinical success has also been documented with clindamycin; however, their use should be guided by confirmed susceptibility testing. Macrolides, fluoroquinolones and tetracyclines are not recommended empirically due to potential resistance, necessitating microbiological confirmation prior to use1.1,4,5 Optimal treatment combines effective pleural drainage with prolonged antibiotic therapy (≥4 weeks).1–5
To conclude, while G. morbillorum remains a rare etiology of pleural empyema, it should be considered in patients with significant comorbidities or predisposing factors. Diagnostic challenges underscore the importance of advanced techniques like MALDI-TOF mass spectrometry for accurate identification. Successful management requires a dual strategy: prompt pleural drainage and tailored antibiotic therapy guided by susceptibility testing and clinical context. Our case illustrates that vancomycin/clindamycin is an effective alternative for G. morbillorum empyema in beta-lactam-allergic patients, particularly when polymicrobial infection is suspected.
Declaration of generative AI and AI-assisted technologies in the writing processNo AI software or tool was involved in this manuscript.
Ethical and informed consentInformed consent was obtained from the patient for the publication, clinical data and images submitted.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributionsAll authors have contributed equally to the preparation and review of this article.
Conflicts of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.