Population data consistently show that asthma is both under- and over-diagnosed; a phenomenon which may approach a false positive diagnosis of 30%.1 In patients with clinical suspected asthma in whom spirometry with bronchodilator testing has been negative, additional tests should be performed to confirm the diagnosis of asthma such us measurement of fractional nitric oxide concentration in exhaled breath (FeNO) and bronchial hyperresponsiveness challenge.1
Asthma is a heterogeneous disease, usually characterised by chronic airway inflammation mediated by different cells (such us eosinophils and mastocytes2) and their mediators. Identification of underlying T2-type airway inflammation is characteristic of certain types of asthma. Measurement of eosinophils in bronchial biopsy and induced sputum are the gold standard method for determining airway inflammation. However, they are not routinely performed, as they are invasive and not widely available due to their technical complexity. Therefore, FeNO is useful as an inflammatory marker, as well as a non-invasive and is easy to perform test.3 It is important to highlight that a FeNO value <40ppb does not rule out asthma and borderline FeNO values (40–50ppb) themselves do not certainly confirm asthma diagnosis considering that they can be increased by other factors.1 Because of that, other tests should be performed for the diagnosis of asthma.
Among hyperresponsiveness bronchial challenge tests, methacholine test is one of the most standardised, mainly useful for its negative predictive value. Unlike spirometry and FeNO, methacholine tests should be done at a secondary hospital care.1
Patients with T2 inflammation have a higher proportion of bronchial hyperresponsiveness.4,5 The aim of our study was to assess if a borderline FeNO value (40–60ppb) was associated with an increased bronchial hyperresponsiveness and complications in patients with suspected asthma.
We conducted a prospective observational study including patients with suspected bronchial asthma who underwent a methacholine test between January 2019 and June 2023. Per protocol, spirometry and FeNO determination were performed prior to methacholine challenge test, following the recommendations of the Spanish Society of Pneumology and Thoracic Surgery (SEPAR).6 The FeNO cut-off point of 40 parts per billion (ppb) was used, a value proposed for asthma diagnosis by the European Respiratory Society1 and the Spanish Guidelines for the Management of Asthma (GEMA).7 In our centre, methacholine test is performed by dosimeter method. The result of the methacholine test is interpreted as the cumulative dose of methacholine that decreases forced expiratory volume in first second (FEV1) by more than 20% (PD20), being considered a moderate–severe hyperresponsiveness when PD20 was less than 0.3mg. Patients with positive methacholine test were administered short acting beta agonists per protocol and short acting muscarinic antagonist if bronchospasm persisted. Complications of methacholine challenge were defined as bronchospasm requiring treatment with systemic corticosteroids. Epidemiological variables, respiratory function and peripheral blood eosinophils in the 6 months prior or after the challenge were collected from each patient. Descriptive and contrast hypothesis statistical analysis were performed. This study was approved by the ethics committee of our hospital.
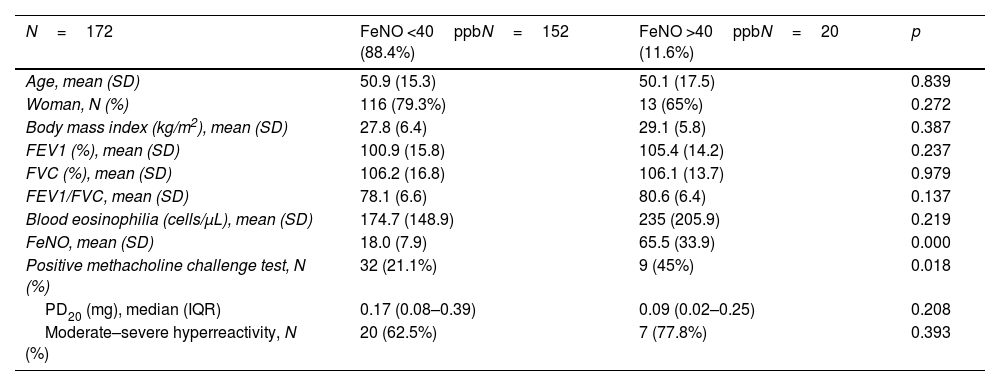
172 patients were included and their characteristics are summarised according to FeNO values in Table 1. When patients were classified according to FeNO, there were no statistically significant differences in epidemiological variables, peripheral blood eosinophilia and spirometry results (FEV1, forced vital capacity (FVC), FEV1/FVC). Mean FeNO was of 23.6ppb (standard deviation 20.4). Patients with FeNO >40ppb represented 11.6% of the sample (80% with a value between 40 and 60ppb).
Characteristics of the included population.
| N=172 | FeNO <40ppbN=152 (88.4%) | FeNO >40ppbN=20 (11.6%) | p |
|---|---|---|---|
| Age, mean (SD) | 50.9 (15.3) | 50.1 (17.5) | 0.839 |
| Woman, N (%) | 116 (79.3%) | 13 (65%) | 0.272 |
| Body mass index (kg/m2), mean (SD) | 27.8 (6.4) | 29.1 (5.8) | 0.387 |
| FEV1 (%), mean (SD) | 100.9 (15.8) | 105.4 (14.2) | 0.237 |
| FVC (%), mean (SD) | 106.2 (16.8) | 106.1 (13.7) | 0.979 |
| FEV1/FVC, mean (SD) | 78.1 (6.6) | 80.6 (6.4) | 0.137 |
| Blood eosinophilia (cells/μL), mean (SD) | 174.7 (148.9) | 235 (205.9) | 0.219 |
| FeNO, mean (SD) | 18.0 (7.9) | 65.5 (33.9) | 0.000 |
| Positive methacholine challenge test, N (%) | 32 (21.1%) | 9 (45%) | 0.018 |
| PD20 (mg), median (IQR) | 0.17 (0.08–0.39) | 0.09 (0.02–0.25) | 0.208 |
| Moderate–severe hyperreactivity, N (%) | 20 (62.5%) | 7 (77.8%) | 0.393 |
SD: standard deviation; FEV1: forced expiratory volume in first second; FVC: forced vital capacity; FeNO: fractional nitric oxide concentration; PD20: cumulative dose of methacholine that decreases forced expiratory volume in first second (FEV1) by more than 20%; IQR: interquartile range.
Patients with FENO > 40ppb had a higher percentage of positive methacholine tests compared to the group with FENO <40ppb (45% vs 21%, p=0.018). Boulet et al. described similar results of positive tests among patients with higher FeNO.4 However, there was no statistical significantly higher severity of bronchial hyperresponsiveness (assessed quantitatively by PD20 and qualitatively) in patients with FeNO >40ppb compared to patients with FeNO <40ppb (p=0.208, p=0.393). Among the 41 cases with positive methacholine test, a correlation analysis was performed between FeNO values and severity of bronchial hyperresponsiveness with no correlation (Pearson test −0.054, p=0.736). Among patients with clinically suspected asthma with FeNO >40ppb, 55% had a negative methacholine bronchial test (negative predictive value for asthma). No complications were observed in any patient.
In our study, patients with FeNO >40ppb had a higher percentage of positive methacholine tests, with no greater severity of bronchial hyperresponsiveness neither more complications. It seems safe to perform a methacholine challenge test in patients with borderline FeNO values, taking into account the test's negative predictive value.
FundingThis work was not supported by any funding.
Authors’ contributionsAll authors contributed equally to this manuscript.
Conflicts of interestWe have no conflicts of interest to disclose.