Antibiotic self-medication is a kind of indiscriminate use of antibiotics. This practice has been growing worldwide, and has been identified as a risk factor for bacterial resistance (according to the WHO, it is one of the most difficult public health problems to combat in the XXI century). This activity has also been observed in the university population, and there is some literature reporting factors among young people that could increase it.
ObjectivesTo describe risk factors associated with antibiotic self-medication among university students from Trujillo, Peru.
Materials and methodsAn observational, analytical, retrospective study was performed using a questionnaire. It was applied to 1000 college students selected by proportional allocation from three universities in Trujillo.
ResultsSeventy percent self-medicated two or more times during the last year. The drug most often used for self-medication was amoxicillin, by 133 students (20.33%). An association was found between antibiotic self-medication and the female gender. No association was found between antibiotic self-medication and age (p=0.46), economic monthly income (p=0.83), knowledge level (p=0.23), health sciences programs (p=0.14) and college year (p=0.15).
ConclusionsA high use of antibiotic self-medication was reported and a probable link to females. However, we could not establish an association between antibiotic self-medication and age, income, prior knowledge about antibiotics, school programs or college years.
Antibiotics are one of the most commonly purchased drugs worldwide, especially in developing countries, where the prevalence of infectious diseases increases their use.1 They represent a large impact due to the costs they generate, the damage to health (adverse reactions and therapeutic failure), and poor therapeutic practices, such as long-term self-medication. These present a global public health problem.2,3
Self-medication is the use of medications to treat common health problems without being prescribed by a doctor.4 However, self-medication in the case of the use of antibiotics has become a dangerous trend, which begins at an early age (adolescence). Studies reveal that this practice is facilitated by easy access to antibiotics, low knowledge about antibiotics, low income, the cost of medical consultation, and prior use of antibiotics, among others.5–8
On the other hand, antibiotic self-medication (ABSM) can alleviate some symptoms, which leads some to stop attending medical advice. However, it has been shown to have negative consequences, such as treatment failure and adverse drug effects (leading to death in the most severe cases), but mainly increased bacterial resistance.9–11
Bacterial resistance is considered a global public health problem, and is caused by the indiscriminate use of antibiotics, as seen in ABSM.12,13 The prevalence of this activity is greater in developing countries, in most cases due to a lack of regulatory systems worldwide, and reports indicate that self-medication is more prevalent in cities of low and middle income.3,14 In addition, other factors have been identified in developing countries, such as foreknowledge of antibiotics, age, and monthly income, among others.15 Another study reveals that this population tends to go to pharmacies, and their choice is mainly based on the recommendation of the pharmacist, as found in a Brazilian study, which concluded that 74% of the pharmacies in a municipality sold antibiotics without a prescription.16
ABSM rates are, on average, 50% in Africa, 40% in the Middle East, from 4% to 75% in Asia and 29% in South America, compared to developed countries in Europe, with an average of from 3 to 19%. Studies in China revealed rates of self-medication with antimicrobials from parents to their children to be 62%.17
The reasons for this high prevalence are multifactorial.18 The liberal practice of undergraduates to self-medicate with antibiotics is common, and students base their use on previous successful experiences. However, we have identified that there is low awareness of antibiotic use and students often misuse them.19
In order to take action and prevent increased ABSM, which brings negative effects in the medium and long term, it was considered necessary to seek the prevalence of this activity in the university population of a city in Peru and to identify the main risk factors which could increase this prevalence.
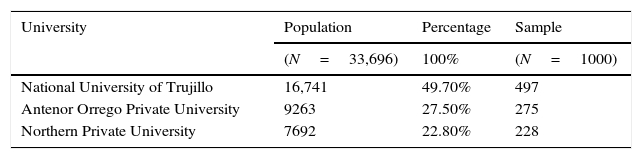
Materials and methodsPopulation and study designAn analytical study using a cross-sectional survey of 1000 undergraduates from three universities in Trujillo was conducted, taking into account the population reference amount used in previous studies.7,12,19 Among the four most representative universities of Trujillo, The National University of Trujillo (UNT by its Spanish acronym) was selected as the only public university in La Libertad, along with 2 randomly selected private universities [The Private Antenor Orrego University (UPAO by its Spanish acronym) and The Northern Private University (UPN)]. The number of students used in the study was selected by proportional allocation based on the number of students enrolled in the 3 universities as per the university national census (INEI 2010) (http://censos.inei.gob.pe/cenaun/redatam_inei/) (see Table 1).
Study questionnaireA bibliographical review of previous studies was performed to identify the elements that form part of the survey instrument. Based on this, and taking into account questionnaires previously validated in other countries adapted to the local population of each country, we developed a questionnaire of our own.9,12 Then, a pilot with a group of 30 college students consistent with the study population was performed to establish changes in the content, design, reading comprehension or facility if needed. However, accurate data were obtained.
The questionnaire consisted of four sections, and contains open and closed questions. The first section recorded the socio-demographic characteristics of respondents such as age, sex, year of study, and economic monthly income. The second section consisted of nine closed questions to provide information on the practice of using antibiotics. The third section consisted of 13 questions to assess the respondents’ knowledge of antibiotics in three aspects: action and use (6 statements), side effects (3 statements) and antibiotic resistance (4 statements). The five-point Likert scale (1=strongly disagree, 5=strongly agree) was used to assess the participants’ responses.
Statistical analysisThe data obtained was entered into the Statistical Package for Social Sciences (SPSS version 23.0) for processing. The results are reported as percentages (95% confidence interval). The Chi Square test (χ2) was used to establish significant difference. Associations were considered significant if p<0.05.
Respondents that answered “strongly agree” or “agree” were classified as “agree”, and those who answered “strongly disagree” or “disagree” were classified as “disagree”. A scoring system was applied to measure knowledge. One point was awarded for the correct answer (strongly agree or agree with the correct statement and strongly disagree or disagree with the incorrect statement), and zero for each incorrect or uncertain response, with a maximum obtainable score of 13 for each respondent. The score classified the knowledge into three levels: low (0–6), moderate (7–10), and high (11–13).
Ethical considerationsThis research was carried out respecting the ethical and moral guidelines governing biomedical research in the latest update of the Declaration of Helsinki, General Health Law No. 26842, Articles 25° – literal c and 53°, and according to the Code of Ethics of the Medical College in Chapter 6 Article 42°.
We report that only the researcher personal will have access to this data, and the verbal consent of each of the respondents was obtained before applying the questionnaire.
ResultsA total of 1000 undergraduate students from 3 universities in Trujillo were included in this study. The average age of all respondents was 19.82 years. Women accounted for 49.2% of the sample studied.
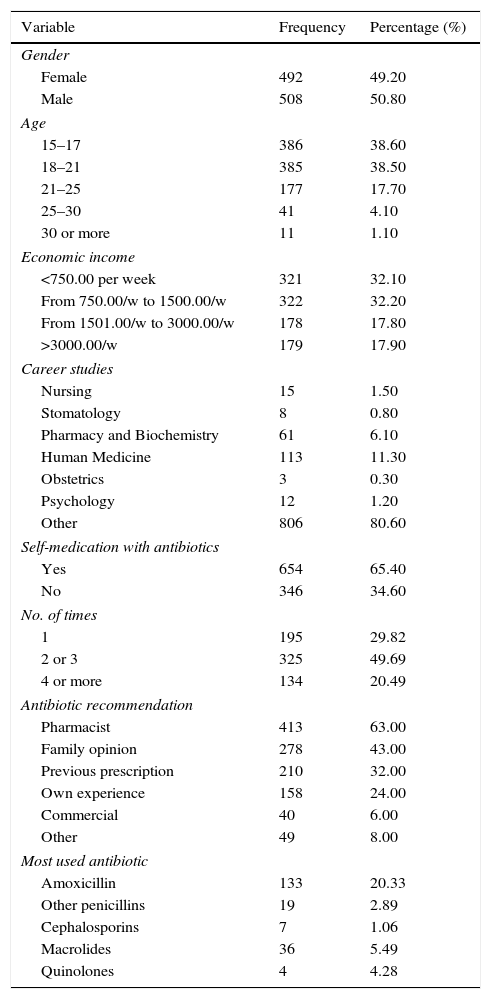
Six out of ten university students said they had consumed at least one antibiotic in the last 12 months preceding the survey. Of these, 70% consumed 2 or more antibiotics in the last year (see Table 2).
Characteristics of respondents (N=1000).
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Gender | ||
| Female | 492 | 49.20 |
| Male | 508 | 50.80 |
| Age | ||
| 15–17 | 386 | 38.60 |
| 18–21 | 385 | 38.50 |
| 21–25 | 177 | 17.70 |
| 25–30 | 41 | 4.10 |
| 30 or more | 11 | 1.10 |
| Economic income | ||
| <750.00 per week | 321 | 32.10 |
| From 750.00/w to 1500.00/w | 322 | 32.20 |
| From 1501.00/w to 3000.00/w | 178 | 17.80 |
| >3000.00/w | 179 | 17.90 |
| Career studies | ||
| Nursing | 15 | 1.50 |
| Stomatology | 8 | 0.80 |
| Pharmacy and Biochemistry | 61 | 6.10 |
| Human Medicine | 113 | 11.30 |
| Obstetrics | 3 | 0.30 |
| Psychology | 12 | 1.20 |
| Other | 806 | 80.60 |
| Self-medication with antibiotics | ||
| Yes | 654 | 65.40 |
| No | 346 | 34.60 |
| No. of times | ||
| 1 | 195 | 29.82 |
| 2 or 3 | 325 | 49.69 |
| 4 or more | 134 | 20.49 |
| Antibiotic recommendation | ||
| Pharmacist | 413 | 63.00 |
| Family opinion | 278 | 43.00 |
| Previous prescription | 210 | 32.00 |
| Own experience | 158 | 24.00 |
| Commercial | 40 | 6.00 |
| Other | 49 | 8.00 |
| Most used antibiotic | ||
| Amoxicillin | 133 | 20.33 |
| Other penicillins | 19 | 2.89 |
| Cephalosporins | 7 | 1.06 |
| Macrolides | 36 | 5.49 |
| Quinolones | 4 | 4.28 |
Sixty three percent of college students who self-medicate took the recommendation of a pharmacist as the basis of their choice of antibiotic. Half of the population who self-medicated with antibiotics decided to stop taking them after the disappearance of symptoms (see Table 2).
The antibiotic most commonly used for self-medication was amoxicillin, by 133 university students (20.33%). Sore throat and fever were the most common complaints, with 54.1% and 47% respectively of students who decided to self-medicate with antibiotics. Approximately one third (35.32%) reported using symptomatic drugs such as paracetamol.
The study shows that 57.3% of college students have a low level of knowledge about antibiotics (see Table 2).
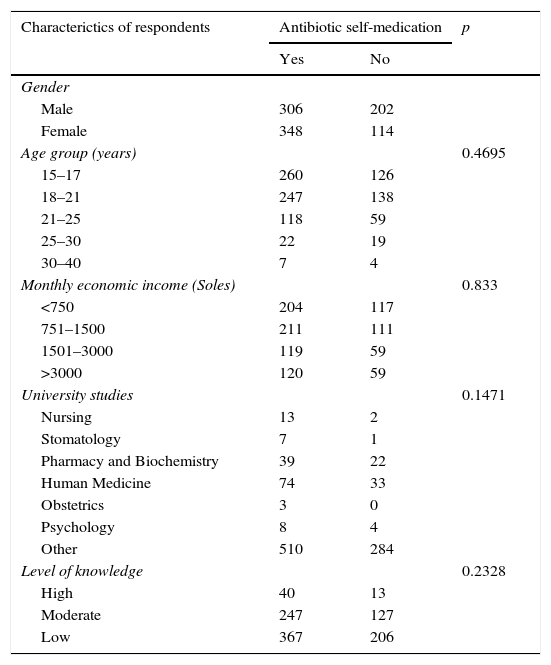
We studied the association between ABSM and certain factors, such as gender, age, monthly income, year of study, a career related to health sciences, and knowledge level. We found an association between the female gender and ABSM {OR: 1595; 95% (1226–2076)}. By contrast, no association between ABSM was found with age, monthly income, level of knowledge, careers related to health sciences or year of study (see Table 3).
Association between antibiotic self-medication and gender, age group, monthly income, university degree and level of knowledge.
| Characterictics of respondents | Antibiotic self-medication | p | |
|---|---|---|---|
| Yes | No | ||
| Gender | |||
| Male | 306 | 202 | |
| Female | 348 | 114 | |
| Age group (years) | 0.4695 | ||
| 15–17 | 260 | 126 | |
| 18–21 | 247 | 138 | |
| 21–25 | 118 | 59 | |
| 25–30 | 22 | 19 | |
| 30–40 | 7 | 4 | |
| Monthly economic income (Soles) | 0.833 | ||
| <750 | 204 | 117 | |
| 751–1500 | 211 | 111 | |
| 1501–3000 | 119 | 59 | |
| >3000 | 120 | 59 | |
| University studies | 0.1471 | ||
| Nursing | 13 | 2 | |
| Stomatology | 7 | 1 | |
| Pharmacy and Biochemistry | 39 | 22 | |
| Human Medicine | 74 | 33 | |
| Obstetrics | 3 | 0 | |
| Psychology | 8 | 4 | |
| Other | 510 | 284 | |
| Level of knowledge | 0.2328 | ||
| High | 40 | 13 | |
| Moderate | 247 | 127 | |
| Low | 367 | 206 | |
This study is the first conducted in Peru to demonstrate ABSM prevalence and factors associated with this activity in college students.
High rates of antibiotics without a prescription were identified in our study: 65.4% (654/1000). These results are similar to previous studies in Ghana and Uganda (with rates of 70 and 75%, respectively),15,20 but higher than in China, European countries and Brazil (38–48%, 40% and 29.3%, respectively).11,21,22 This high prevalence could be due to the difficulty of access to the Health Care System and insufficient income levels to access private physicians. The similarity with studies in Ghana and Uganda is possibly the result of the sociodemographic characteristics of the populations studied, and belonging to developing countries, which does not happen with countries like China, Brazil and European countries.
In our study, we found that 40% of college students attended a pharmacist directly and 30% used prior medical prescriptions for similar symptoms. This correlates with the studies found in the literature which show that the patient's expectation is a factor in antibiotic prescriptions by pharmacists.10,22
The most common drug used by college students who self-medicated was amoxicillin, by 133 (20.3%), which is also consistent with other published studies.23,24 This may be because it is the most used antibiotic worldwide and the antibiotic most prescribed by doctors.
Our study found an association between ABSM and the female gender, as found in a study conducted in the UK.25 No association between ABSM and age group, monthly income, year of university study, study program or level of knowledge was found, as is seen in other studies, which may be because the number of respondents in each subgroup were insufficient to establish an association.14,25,26
It must be mentioned that in Peru, the General Health Law 26842, in Article 26, states that: “Only doctors can prescribe medication. Dentists and obstetricians may prescribe within the area of their competence.” Article 33 states: “The pharmaceutical chemist is responsible for dispensing, user information and guidance on the use of medicines. They are not authorized to prescribe drugs.” However, the results of our study show that an audit system should be implemented for pharmaceutical centers, so that they are susceptible to the corresponding fine prescribed in the Pharmaceutical Establishments Regulation (RM-Ministerial Resolution No. 304-2002/SA/DM). This would help reduce the irrational use of antibiotics in our population, also, the data revealed will form the basis for future campaigns on the rational use of antibiotics in this population group.
Being that this analytical cross-sectional study used a survey to estimate the prevalence of ABSM in the past, recall bias cannot be ruled out. Respondents could also have no knowledge about what an antibiotic is, although this may be a minor problem, particularly among our respondents, as they were all college students. For these reasons, it is unclear whether our findings are generalizable to other universities in Peru.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo external funding was received for the development of this work.
Conflict of interestThe authors of this paper declare no conflict of interest.