Anaphylaxis is a severe systemic allergic reaction that is rapid in onset and is potentially fatal. Its severity varies in relation to the affected organs and the intensity of the damage to these. The more severe forms are associated with airway obstruction (laryngeal edema, severe bronchoconstriction) and/or vascular collapse (anaphylactic shock).1,2
The frequency of anaphylaxis ranges from 0.03% to 0.95%. Its lifetime can be of up to 2.6%. Although anaphylaxis occurs more frequently in children and adolescents, fatal cases are more common in adults. Even though mortality rates are sub-reported, it is estimated to occur in 0.65–2% of severe anaphylaxis cases. Laryngeal edema and cardiovascular complications are the main cause of death.2–6
Anaphylaxis can occur as a consequence of immunological and non-immunological mechanisms. In general, the most frequent form of anaphylaxis is associated with IgE-mediated hypersensitivity reactions. Nevertheless, aside from the mechanism involved in the onset of response, a common pathophysiological characteristic of anaphylaxis is the degranulation of basophils and mast cells, with the consequent liberation of mediators of inflammation, including histamine, leukotrienes and prostaglandins. The action of these mediators in the skin, mucous membranes, airways, gastrointestinal tract, cardiovascular system, and other target organs, originates the signs and symptoms of anaphylaxis.2,4 The most common causes of anaphylaxis are medications, drugs and hymenoptera venoms. Other causes of anaphylaxis mediated by immunological mechanisms include allergen immunotherapy, latex, occupational allergens, seminal fluid, aeroallergens and monoclonal antibodies. Exercise, some physical factors (cold, heat and radiation), ethanol, opioid medications and contrast media, may cause non-immunological anaphylaxis. Idiopathic anaphylaxis, where it is not possible to identify the cause, represents over 20% of all anaphylaxis cases.2–7
Anaphylaxis is characterized by a varied clinical presentation and its manifestations include skin, respiratory, ocular, cardiovascular and gastrointestinal symptoms. Vital functions are compromised in the most severe forms, and if this occurs during the first minutes after the onset of the reaction, the risk of death is greater.1,2,8,9
Over 90% of the patients display skin symptoms. Most episodes begin with pruritus and flushing and continue with the progressive development of hives and/or angioedema. Eyes and mucous membranes can acquire a congestive-like aspect, changes generally associated with intense itching, epiphora and rhinorrhea. Gastrointestinal symptoms include abdominal pain, nausea, vomiting, and diarrhea. At a respiratory level, the symptoms can include tightness in the throat, dysphagia, dysphonia, inspiratory stridor and even signs of asphyxia, which is caused by the generation of laryngeal edema. On the other hand, cough, dyspnea, wheezing, a feeling of tightness in the chest may onset as a consequence of bronchoconstriction, which can also cause hypoxemia and cyanosis. Cardiovascular manifestations may onset with tachycardia and a feeling of dizziness or instability, and progress until the loss of consciousness. Peripheral vasodilatation and the increase in vascular permeability, characteristics of anaphylaxis, lead to hypotension and shock, which increase heart rate and reduce coronary perfusion. These cardiovascular changes, in addition to hypoxemia related to the obstruction of the airways, reduce cardiac oxygenation and may lead to arrhythmias and myocardium necrosis, which are causes of cardiac arrest. In some cases, anaphylaxis onset can be abrupt, like syncope, or even cause sudden death. Other manifestations that may occur during anaphylaxis are; disorientation, anxiety, seizures and profuse sweating.1,2,8–11
Approximately 20% of patients presenting anaphylaxis may suffer biphasic reactions. In these cases, the late phase begins between 1 and 72h after the initial phase, usually with similar clinical manifestations. No clinical data has been identified which allows the prediction of risk of late reactions in a trustworthy manner. However, the patients who present severe initial reactions may have a greater risk of suffering biphasic reactions.1,8,9
DiagnosisThe diagnosis of anaphylaxis is fundamentally clinical. Clinical history constitutes the most important tool in the identification of a patient who is suffering from anaphylaxis and it is also of great help to identify its cause. In addition to the detailed description of signs and symptoms present in the patient, it is important to obtain information about the moment of onset of the reaction, medication used to treat it, the duration of the episode and exposure to allergens or potential triggers. Whenever possible, we ought to question the people who witnessed the event.9–13
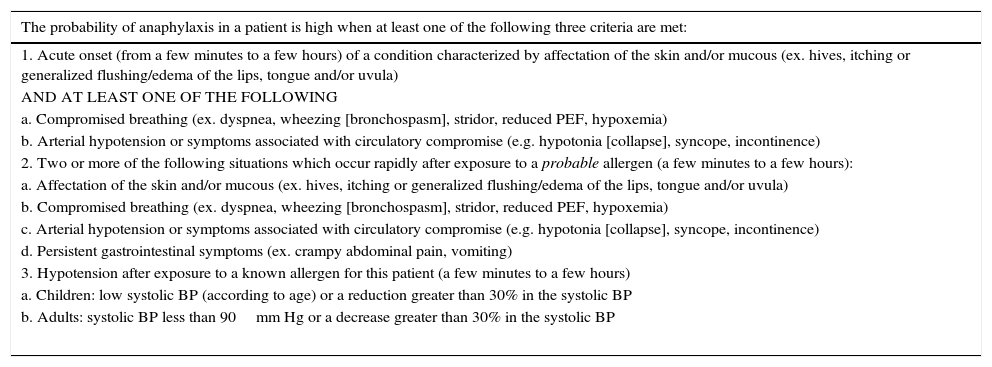
Useful clinical criteria have been established for the diagnosis of anaphylaxis, which are listed in Table 1. With the proper use of these criteria, it is possible to identify over 95% of anaphylaxis cases.1
Clinical criteria for anaphylaxis diagnosis.
| The probability of anaphylaxis in a patient is high when at least one of the following three criteria are met: |
|---|
| 1. Acute onset (from a few minutes to a few hours) of a condition characterized by affectation of the skin and/or mucous (ex. hives, itching or generalized flushing/edema of the lips, tongue and/or uvula) |
| AND AT LEAST ONE OF THE FOLLOWING |
| a. Compromised breathing (ex. dyspnea, wheezing [bronchospasm], stridor, reduced PEF, hypoxemia) |
| b. Arterial hypotension or symptoms associated with circulatory compromise (e.g. hypotonia [collapse], syncope, incontinence) |
| 2. Two or more of the following situations which occur rapidly after exposure to a probable allergen (a few minutes to a few hours): |
| a. Affectation of the skin and/or mucous (ex. hives, itching or generalized flushing/edema of the lips, tongue and/or uvula) |
| b. Compromised breathing (ex. dyspnea, wheezing [bronchospasm], stridor, reduced PEF, hypoxemia) |
| c. Arterial hypotension or symptoms associated with circulatory compromise (e.g. hypotonia [collapse], syncope, incontinence) |
| d. Persistent gastrointestinal symptoms (ex. crampy abdominal pain, vomiting) |
| 3. Hypotension after exposure to a known allergen for this patient (a few minutes to a few hours) |
| a. Children: low systolic BP (according to age) or a reduction greater than 30% in the systolic BP |
| b. Adults: systolic BP less than 90mm Hg or a decrease greater than 30% in the systolic BP |
PEF, peak expiratory flow; BP, blood pressure.
*Low systolic blood pressure in children is defined as less than 70mm Hg in children from 1 month to 1 year old; less than 70mm.
Hg+2× years of age, in children from 1 to 10 years old, and less than 90mm Hg in patients from 11 to 17 years old.
During the clinical evaluation of the patient, we should always consider other conditions which may occur with similar signs and symptoms to those of anaphylaxis. Differential diagnoses include: vasovagal reactions, anxiety, myocardial dysfunction, pulmonary embolism, foreign body aspiration, poisoning, hypoglycemia, convulsive disorders, urticaria and angioedema, hereditary angioedema and asthma. Although urticaria and angioedema may occur up to 90% of anaphylaxis episodes, when it occurs without affecting other organs or systems, it does not correspond to anaphylaxis cases.9–13
Serum tryptase, plasmatic histamine and histamine metabolites in urine (methyl-histamine) may be useful to confirm an anaphylaxis diagnosis. The best time for its measurement after the onset of the anaphylaxis episode is between 1 and 6h for serum tryptase, from 10min to 1h for histamine and during the first 24h for methyl-histamine. Nevertheless, these studies are not always available and the administration of the treatment should not be delayed.1,10–14
On the other hand, as a part of the attention in the emergency service, in moderate to severe anaphylaxis, it is convenient to perform a complete blood count, metabolic panel, arterial blood gas, and chest x-rays in order to assess the patient's general condition as well as rule out other diagnoses.9,11–13,15
TreatmentTimely treatment considerably reduces the risk of mortality in patients with anaphylaxis. Management ought to begin with an evaluation and the maintenance of airways, ventilation and circulation.1,9–15
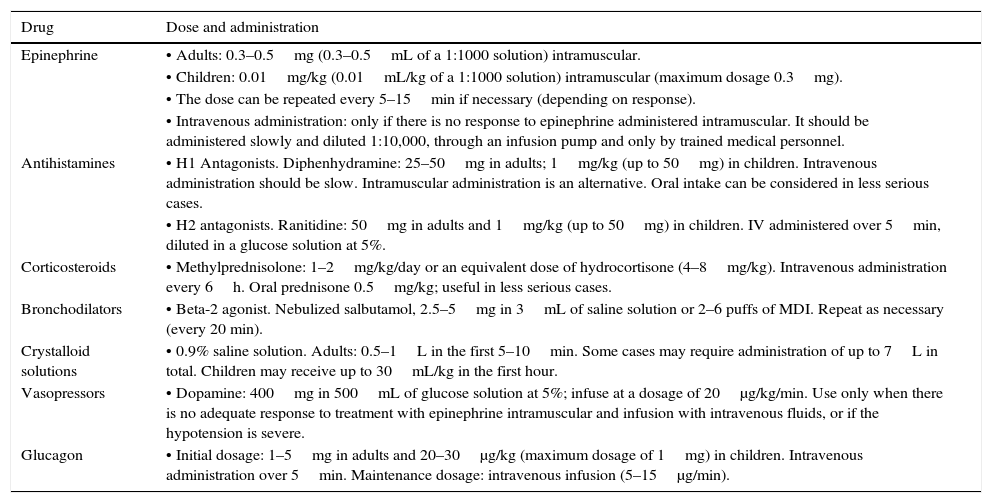
If the patient meets clinical criteria for an anaphylaxis diagnosis, epinephrine should be administered immediately. The recommended dose is 0.01mg/kg (maximum dose of 0.3mg in children and 0.5mg in adults) administered intramuscular in the antero-lateral area of the thigh, repeating every 5–15min if necessary (Table 2). Intravenous administration is an option in patients with severe hypotension or cardiovascular collapse who do not respond to treatment with intramuscular epinephrine and intravenous fluids. Nevertheless, due to the risks of lethal arrhythmia, the latter form of administration should be considered only when continuous cardiac monitoring is possible.1,2,4,8–16
Drugs indicated in the treatment of anaphylaxis.
| Drug | Dose and administration |
|---|---|
| Epinephrine | • Adults: 0.3–0.5mg (0.3–0.5mL of a 1:1000 solution) intramuscular. |
| • Children: 0.01mg/kg (0.01mL/kg of a 1:1000 solution) intramuscular (maximum dosage 0.3mg). | |
| • The dose can be repeated every 5–15min if necessary (depending on response). | |
| • Intravenous administration: only if there is no response to epinephrine administered intramuscular. It should be administered slowly and diluted 1:10,000, through an infusion pump and only by trained medical personnel. | |
| Antihistamines | • H1 Antagonists. Diphenhydramine: 25–50mg in adults; 1mg/kg (up to 50mg) in children. Intravenous administration should be slow. Intramuscular administration is an alternative. Oral intake can be considered in less serious cases. |
| • H2 antagonists. Ranitidine: 50mg in adults and 1mg/kg (up to 50mg) in children. IV administered over 5min, diluted in a glucose solution at 5%. | |
| Corticosteroids | • Methylprednisolone: 1–2mg/kg/day or an equivalent dose of hydrocortisone (4–8mg/kg). Intravenous administration every 6h. Oral prednisone 0.5mg/kg; useful in less serious cases. |
| Bronchodilators | • Beta-2 agonist. Nebulized salbutamol, 2.5–5mg in 3mL of saline solution or 2–6 puffs of MDI. Repeat as necessary (every 20 min). |
| Crystalloid solutions | • 0.9% saline solution. Adults: 0.5–1L in the first 5–10min. Some cases may require administration of up to 7L in total. Children may receive up to 30mL/kg in the first hour. |
| Vasopressors | • Dopamine: 400mg in 500mL of glucose solution at 5%; infuse at a dosage of 20μg/kg/min. Use only when there is no adequate response to treatment with epinephrine intramuscular and infusion with intravenous fluids, or if the hypotension is severe. |
| Glucagon | • Initial dosage: 1–5mg in adults and 20–30μg/kg (maximum dosage of 1mg) in children. Intravenous administration over 5min. Maintenance dosage: intravenous infusion (5–15μg/min). |
The need for therapeutic procedures in addition to the administration of epinephrine in the patient with anaphylaxis should be individualized according to the present situation in each particular case and the response to treatment. 9–16 These measures include:
- •
Monitoring of vital signs and surveillance of the level of consciousness.
- •
Supine position with elevation of lower extremities in case of hypotension.
- •
Canalization of the peripheral venous way.
- •
Ventilatory assistance with a bag-valve-mask device. Consider endotracheal intubation or cricothyroidotomy if the severity of the episode requires it.
- •
Administration of oxygen (6–8L/min). Pulse oximetry is a guide to determine the oxygen requirements.
- •
Fluid resuscitation. The use of crystalloid solutions (normal saline) is preferred (Table 2). Colloid volume expanders are an option, but they have not shown be better than crystalloid solutions for the treatment of hypotension in anaphylaxis.
- •
Antihistamines. They are second line drugs in anaphylaxis. Antihistamines may be useful for the treatment of cutaneous and mucous membranes symptoms. In anaphylaxis, it is recommended the use of a combination of H1 and H2 antagonists (Table 2).
- •
Inhaled beta-2 adrenergic agonists, if there is bronchospasm resistant to epinephrine (Table 2).
- •
Corticosteroids. Although they are not useful in the early phase of anaphylaxis, they can potentially reduce the risk of late phase reactions (Table 2).
- •
In cases of hypotension refractory to treatment with intravenous fluids and epinephrine, The administration of vasopressors should be considered, with the aim of maintaining arterial pressure above 90mm Hg. Continuous hemodynamic monitoring is necessary (Table 2).
- •
Glucagon is an alternative in patients who are undergoing treatment with beta-adrenergic blockers and do not respond to treatment with epinephrine (Table 2).
- •
Vasopressors. If epinephrine injections and fluid resuscitation fail to alleviate hypotension, vasopressors (such as dopamine) should be administered (Table 2).
- •
If the patient presents cardiopulmonary arrest, life support maneuvers should be applied and the patient should be transferred to an intensive care unit, if necessary.
Considering the possibility of late reactions, an observation period is recommended after the early phase, even though the symptoms may have disappeared with the initial attention. The observation periods should be personalized. In most cases, a 4–6h observation period in emergency services is reasonable. However, in patients with severe symptoms or refractions to the treatment, the observation period should be longer. The need of hospitalization should be considered in cases of respiratory or cardiovascular compromise which puts the patient's life at risk, anaphylaxis refractory to the initial treatment, late reactions, and patients with a significant risk of severe complications due to pre-existing cardiac or pulmonary diseases.1,8–16
Discharge recommendationsDischarge recommendations for a patient who has suffered an anaphylaxis episode should include:
- 1.
A prescription of self-administered epinephrine in case of a new episode of anaphylaxis. The use of auto-injector devices is recommended whenever possible.
- 2.
Provide a written emergency plan guiding the patient on the steps to take in case of onset of anaphylaxis symptoms.
- 3.
Instructions and enough information on the nature of their problem should be provided, as well as how to avoid exposure to allergens or potential triggers.
- 4.
Refer the patient to an allergist for his/her study and possible identification of the specific cause of anaphylaxis, as well as to evaluate the possibility of a desensitization treatment or specific allergen immunotherapy.9–16
Anaphylaxis is a systemic reaction, it is life-threatening and it has a rapid onset. The most frequent triggers are medications, foods and hymenoptera venom. Diagnosis is based on clinical criteria. Clinical manifestations include skin, respiratory, cardiovascular and gastrointestinal signs and symptoms. Epinephrine (intramuscular) is the first choice of treatment and should be administered as soon as the anaphylaxis diagnosis is made. Treatment additional to the epinephrine will depend on the clinical manifestations of each case. The patient's observation period after the attention of the early phase should be individualized according to the severity of the anaphylaxis. At the moment of hospital discharge, self-administration of epinephrine should always be prescribed for all patients who suffered anaphylaxis. It is essential to provide a written action plan in case of future events of anaphylaxis and to refer the patient to an allergist for long-term attention.
Conflict of interestThe author has no conflicts of interest to declare.
FundingNo financial support was provided.