The SARS-CoV-2 infection presents, in most cases, with mild symptoms.1 However, up to 13% of cases develop severe symptoms,2 with acute respiratory distress associated with a massive release of pro-inflammatory mediators.3 The identification of patients at risk of developing severe symptoms would allow optimization of therapeutic algorithms. This study analyses demographic, clinical-radiological and analytical data of admitted patients to try to establish predictive mortality and ICU admission variables.
Fifty-two patients admitted to the Navarra Hospital Complex from 22nd March to 5th April 2020 with confirmed SARS-CoV-2 infection were prospectively included. Patients with pathologies other than SARS-CoV-2 infection as a cause of admission were excluded. The CURB65 clinical scale was calculated4 for stratification of patients. Blood tests were performed upon admission with the following inflammatory markers: lymphocyte count (⋅109), fibrinogen (mg/dl), dimer-D (ng/ml), ferritin (μg/l), LDH (U/l), troponin-I (pg/ml) and CRP (mg/l). These determinations were repeated at 48 h of admission after the implementation of the treatment protocols indicated at that time. The main outcome variable was a combined variable that included death during admission or the need for transfer to the ICU due to SARS-CoV-2 infection. Univariate logistic regression models were constructed for the outcome variable and ROC (receiver-operating characteristics) analysis of the models was performed.
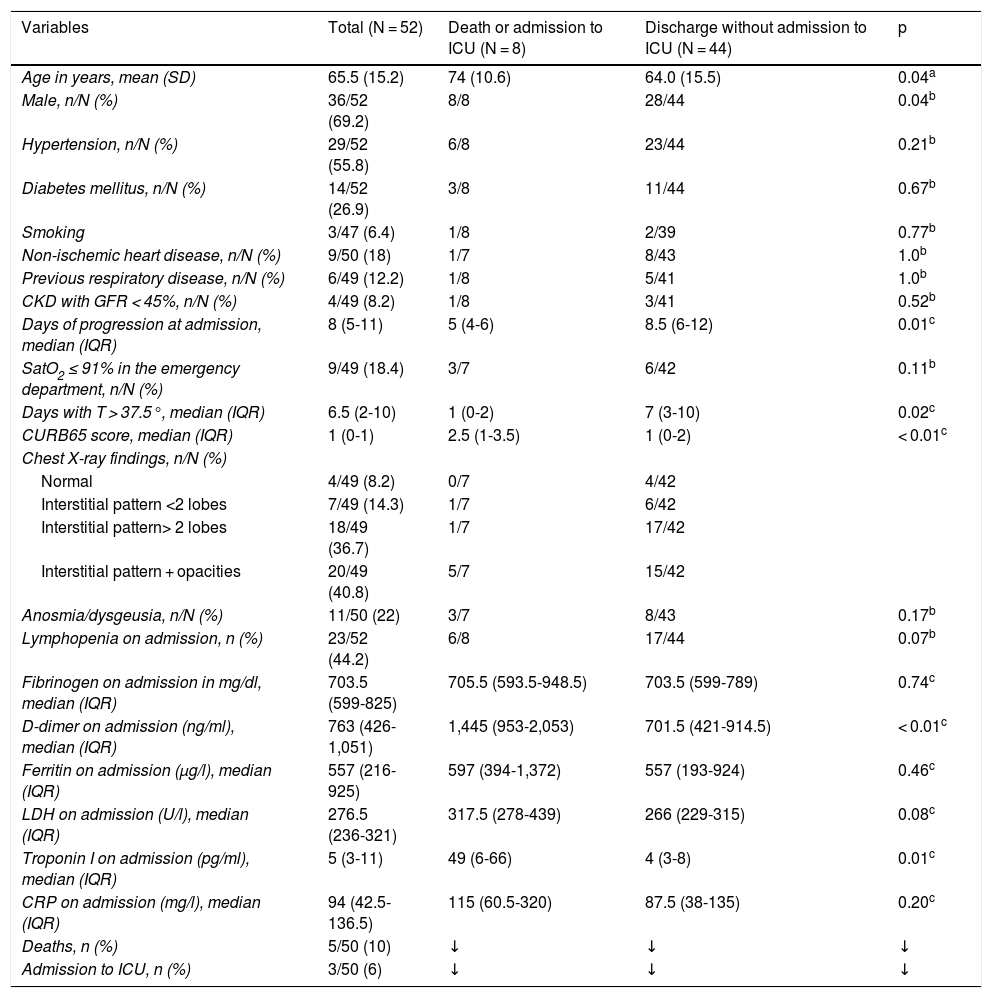
A total of 52 patients were analysed (Table 1). At least 3 of the 7 parameters of inflammation evaluated were elevated in all of them. A correlation was observed between CRP levels and LDH levels (Pearson's r coefficient, 0.44, p < 0.01), fibrinogen (0.74, p < 0.01) and ferritin (0.40, p < 0.01). D-dimer levels at admission were correlated with troponin-I levels (0.66, p < 0.01) but not with acute phase reactants (CRP, LDH, fibrinogen, and ferritin).
Characteristics of the patients.
| Variables | Total (N = 52) | Death or admission to ICU (N = 8) | Discharge without admission to ICU (N = 44) | p |
|---|---|---|---|---|
| Age in years, mean (SD) | 65.5 (15.2) | 74 (10.6) | 64.0 (15.5) | 0.04a |
| Male, n/N (%) | 36/52 (69.2) | 8/8 | 28/44 | 0.04b |
| Hypertension, n/N (%) | 29/52 (55.8) | 6/8 | 23/44 | 0.21b |
| Diabetes mellitus, n/N (%) | 14/52 (26.9) | 3/8 | 11/44 | 0.67b |
| Smoking | 3/47 (6.4) | 1/8 | 2/39 | 0.77b |
| Non-ischemic heart disease, n/N (%) | 9/50 (18) | 1/7 | 8/43 | 1.0b |
| Previous respiratory disease, n/N (%) | 6/49 (12.2) | 1/8 | 5/41 | 1.0b |
| CKD with GFR < 45%, n/N (%) | 4/49 (8.2) | 1/8 | 3/41 | 0.52b |
| Days of progression at admission, median (IQR) | 8 (5-11) | 5 (4-6) | 8.5 (6-12) | 0.01c |
| SatO2 ≤ 91% in the emergency department, n/N (%) | 9/49 (18.4) | 3/7 | 6/42 | 0.11b |
| Days with T > 37.5°, median (IQR) | 6.5 (2-10) | 1 (0-2) | 7 (3-10) | 0.02c |
| CURB65 score, median (IQR) | 1 (0-1) | 2.5 (1-3.5) | 1 (0-2) | < 0.01c |
| Chest X-ray findings, n/N (%) | ||||
| Normal | 4/49 (8.2) | 0/7 | 4/42 | |
| Interstitial pattern <2 lobes | 7/49 (14.3) | 1/7 | 6/42 | |
| Interstitial pattern> 2 lobes | 18/49 (36.7) | 1/7 | 17/42 | |
| Interstitial pattern + opacities | 20/49 (40.8) | 5/7 | 15/42 | |
| Anosmia/dysgeusia, n/N (%) | 11/50 (22) | 3/7 | 8/43 | 0.17b |
| Lymphopenia on admission, n (%) | 23/52 (44.2) | 6/8 | 17/44 | 0.07b |
| Fibrinogen on admission in mg/dl, median (IQR) | 703.5 (599-825) | 705.5 (593.5-948.5) | 703.5 (599-789) | 0.74c |
| D-dimer on admission (ng/ml), median (IQR) | 763 (426-1,051) | 1,445 (953-2,053) | 701.5 (421-914.5) | < 0.01c |
| Ferritin on admission (μg/l), median (IQR) | 557 (216-925) | 597 (394-1,372) | 557 (193-924) | 0.46c |
| LDH on admission (U/l), median (IQR) | 276.5 (236-321) | 317.5 (278-439) | 266 (229-315) | 0.08c |
| Troponin I on admission (pg/ml), median (IQR) | 5 (3-11) | 49 (6-66) | 4 (3-8) | 0.01c |
| CRP on admission (mg/l), median (IQR) | 94 (42.5-136.5) | 115 (60.5-320) | 87.5 (38-135) | 0.20c |
| Deaths, n (%) | 5/50 (10) | ↓ | ↓ | ↓ |
| Admission to ICU, n (%) | 3/50 (6) | ↓ | ↓ | ↓ |
SD: standard deviation; CKD: chronic kidney disease; GFR: glomerular filtration; LDH: lactate dehydrogenase; CRP: C-reactive protein; IQR: interquartile range 25-75; ICU: intensive care unit.
The score on the CURB65 scale was associated with a higher risk of dying or requiring admission to the ICU (OR 4.27; CI 95%: 1.6-11.25). Among the inflammatory parameters on admission, troponin-I levels (OR 2.21; CI 95%: 1.17-4.16) and D-dimer (OR 11.98; CI 95%: 1.72-83.27) were associated with a worse prognosis. Increasing D-dimer levels above laboratory normal limits (500 ng/ml) showed a negative predictive value of 100%. The ROC analysis of the predictive ability of D-dimer levels showed an AUC of 0.81 (CI 95%: 0.69-0.92), and a cut-off point> 1,200 ng/ml showed a sensitivity of 71.43% and a specificity of 90.91%.
Increasing levels of troponin-I above laboratory normal limits (34 pg/ml) associated a worse prognosis (Wilcoxon test, p < 0.01). ROC analysis for troponin-I levels yielded an AUC of 0.81 (CI 95%: 0.67-0.92), with a cut-off point of 34 pg/ml to obtain the best sensitivity (66.67%) and specificity (91.89%) data.
D-dimer values (OR 4.89; CI 95%: 1.26-18.93) and CRP at 48 h were associated with the risk of dying or requiring admission to the ICU (OR 5.36; CI 95%: 1.19-24.09). A prognostic scale was created with the number of inflammatory parameters increased above the normal limits, associating the score at admission to a worse prognosis (for each increased value: OR 2.6; CI 95%: 1.17-5.76).
Some of the factors described in the literature as predictors of a worse prognosis in SARS-CoV-2 infection (age and male sex) are maintained in our study.1 All of the deceased patients (5/52) and those who required ICU were male, and advanced age was associated with higher mortality. In addition, higher scores on the CURB65 scale were associated with higher mortality, as in other published studies.5
Previous studies have shown an increase in inflammatory parameters and mild cytopenia in cases of severe progression.3 Elevated levels of D-dimer and troponin-I on admission were associated with higher mortality and disease severity in our population, with a negative predictive value of 100% in the case of D-dimer.
In conclusion, the use of inflammatory parameters such as troponin-I or D-dimer, as well as clinical scales such as CURB65, help to predict a worse COVID-19 disease progression. Their implementation in clinical practice makes it possible to optimize therapeutic algorithms and rationalize resources in situations of health crisis.
Please cite this article as: Marta-Enguita J, Corroza-Laviñeta J, Ostolaza A. Factores de riesgo y predictores de gravedad en pacientes hospitalizados por COVID-19: análisis de 52 casos. Med Clin (Barc). 2020;155:360–361.