The current SARS-CoV-2 (causing COVID-19) coronavirus pandemic has been particularly devastating for the elderly, a group that has accounted for more than 85% of deaths from this disease.1 In this context, COVID-19 has severely disrupted nursing homes, where a large number of elderly people live (average age 87 ), with high multimorbidity (46% of people with dementia), complexity (51% of high-risk adjusted morbidity groups [AMG]), and a high prevalence of end-of-life situations (54%), with an overall annual mortality above 20%.2,3
This fact, together with the clinical presentation peculiarities in this population group -which often manifests itself in atypical clinical presentations,4 the coexistence of multiple residents in restricted living spaces, the health care model in these centres and the shortage of human and other resources in the sector, have provided a perfect scenario that has impacted both on a systemic and individual level.5 On a systemic level, care responses in these facilities have been heavily influenced by the impact of the pandemic on all other health and social system resources, which have been overwhelmed in their response capacity.6 On an individual level, the clinical complexity of these people and the epidemiological context have generated significant difficulties in decision-making, both for residents, their families, and the professionals in charge of their care.5
In the absence of definitive data, it is estimated that in developed countries more than half of all deaths from COVID-19 are concentrated in nursing homes - which in the case of Spain could rise to practically 2/3 (17,848 of the total of 26,920 deceased, as of 12th May).7 Taking into account that in Spain there are about 5,450 nursing-homes, with more than 270,000 residents,8 the need for specific measures, solid criteria and key ethical principles is evident in order to guide and support professionals and organizations in this very complex situation.9,10 To this end, the chairs of Palliative Care and Bioethics at the UVic-UCC, the Centre for Social and Health Studies (CESS) and the research group on chronicity in Central Catalonia (C3RG) have promoted a consensus with multiple organisations, which is outlined in this article.
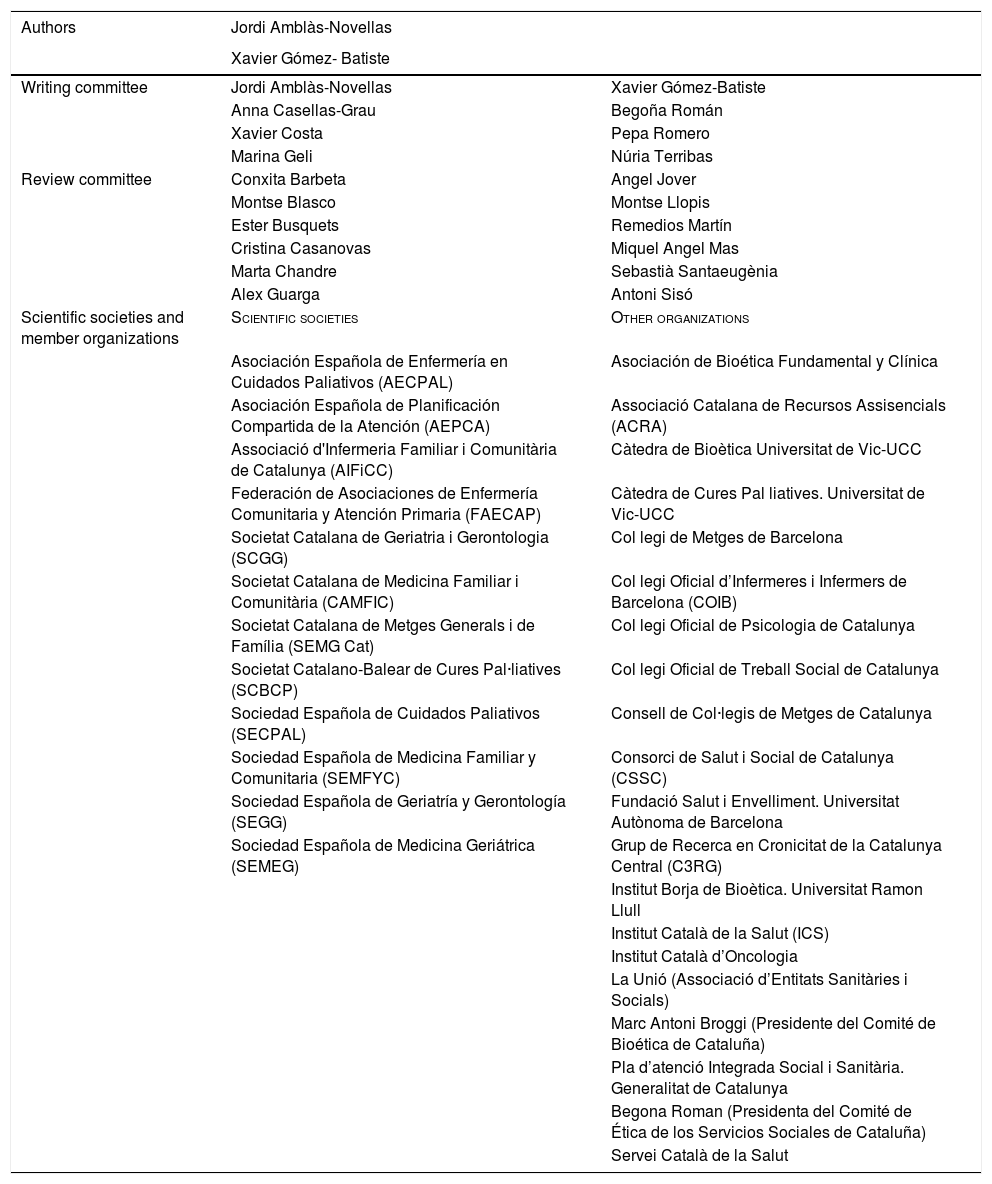
MethodologyGiven the lack of published evidence, as well as the need for a rapid consensus on recommendations, a flexible methodological proposal has been designed in 3 stages: 1) rapid literature review by editors, in a peer review process; 2) establishment of a authoring group and a review group, both made up of multidisciplinary professionals from different areas of the health and social system, and 3) consensus of the master document recommendations with scientific societies and other organizations (Table 1).
Proffesionals and entities participating in the consensus, in alphabetical order.
| Authors | Jordi Amblàs-Novellas | |
|---|---|---|
| Xavier Gómez- Batiste | ||
| Writing committee | Jordi Amblàs-Novellas | Xavier Gómez-Batiste |
| Anna Casellas-Grau | Begoña Román | |
| Xavier Costa | Pepa Romero | |
| Marina Geli | Núria Terribas | |
| Review committee | Conxita Barbeta | Angel Jover |
| Montse Blasco | Montse Llopis | |
| Ester Busquets | Remedios Martín | |
| Cristina Casanovas | Miquel Angel Mas | |
| Marta Chandre | Sebastià Santaeugènia | |
| Alex Guarga | Antoni Sisó | |
| Scientific societies and member organizations | Scientific societies | Other organizations |
| Asociación Española de Enfermería en Cuidados Paliativos (AECPAL) | Asociación de Bioética Fundamental y Clínica | |
| Asociación Española de Planificación Compartida de la Atención (AEPCA) | Associació Catalana de Recursos Assisencials (ACRA) | |
| Associació d'Infermeria Familiar i Comunitària de Catalunya (AIFiCC) | Càtedra de Bioètica Universitat de Vic-UCC | |
| Federación de Asociaciones de Enfermería Comunitaria y Atención Primaria (FAECAP) | Càtedra de Cures Pal liatives. Universitat de Vic-UCC | |
| Societat Catalana de Geriatria i Gerontologia (SCGG) | Col legi de Metges de Barcelona | |
| Societat Catalana de Medicina Familiar i Comunitària (CAMFIC) | Col legi Oficial d’Infermeres i Infermers de Barcelona (COIB) | |
| Societat Catalana de Metges Generals i de Família (SEMG Cat) | Col legi Oficial de Psicologia de Catalunya | |
| Societat Catalano-Balear de Cures Pal·liatives (SCBCP) | Col legi Oficial de Treball Social de Catalunya | |
| Sociedad Española de Cuidados Paliativos (SECPAL) | Consell de Col·legis de Metges de Catalunya | |
| Sociedad Española de Medicina Familiar y Comunitaria (SEMFYC) | Consorci de Salut i Social de Catalunya (CSSC) | |
| Sociedad Española de Geriatría y Gerontología (SEGG) | Fundació Salut i Envelliment. Universitat Autònoma de Barcelona | |
| Sociedad Española de Medicina Geriátrica (SEMEG) | Grup de Recerca en Cronicitat de la Catalunya Central (C3RG) | |
| Institut Borja de Bioètica. Universitat Ramon Llull | ||
| Institut Català de la Salut (ICS) | ||
| Institut Català d’Oncologia | ||
| La Unió (Associació d’Entitats Sanitàries i Socials) | ||
| Marc Antoni Broggi (Presidente del Comité de Bioética de Cataluña) | ||
| Pla d’atenció Integrada Social i Sanitària. Generalitat de Catalunya | ||
| Begona Roman (Presidenta del Comité de Ética de los Servicios Sociales de Cataluña) | ||
| Servei Català de la Salut |
Firstly, a rapid non-systematic search was carried out, highlighting 5 articles on COVID-19 in the nursing home setting which were considered particularly relevant by the editors4,7–10 as well as 3 other articles related to palliative care and ethics in decision-making in this setting.11–13 In order to provide some context for the project, it was necessary to review the data related to the COVID-19 pandemic and the situation of nursing-homes in Spain.1–3,7,8
Preparation of recommendationsOn the basis of this evidence and the experience of the corresponding professionals, the writing group produced a first draft, which was subsequently assessed and improved by the review group. In the preliminary document resulting from this process, and pending final contributions from scientific societies and other organisations, the following recommendations were agreed:
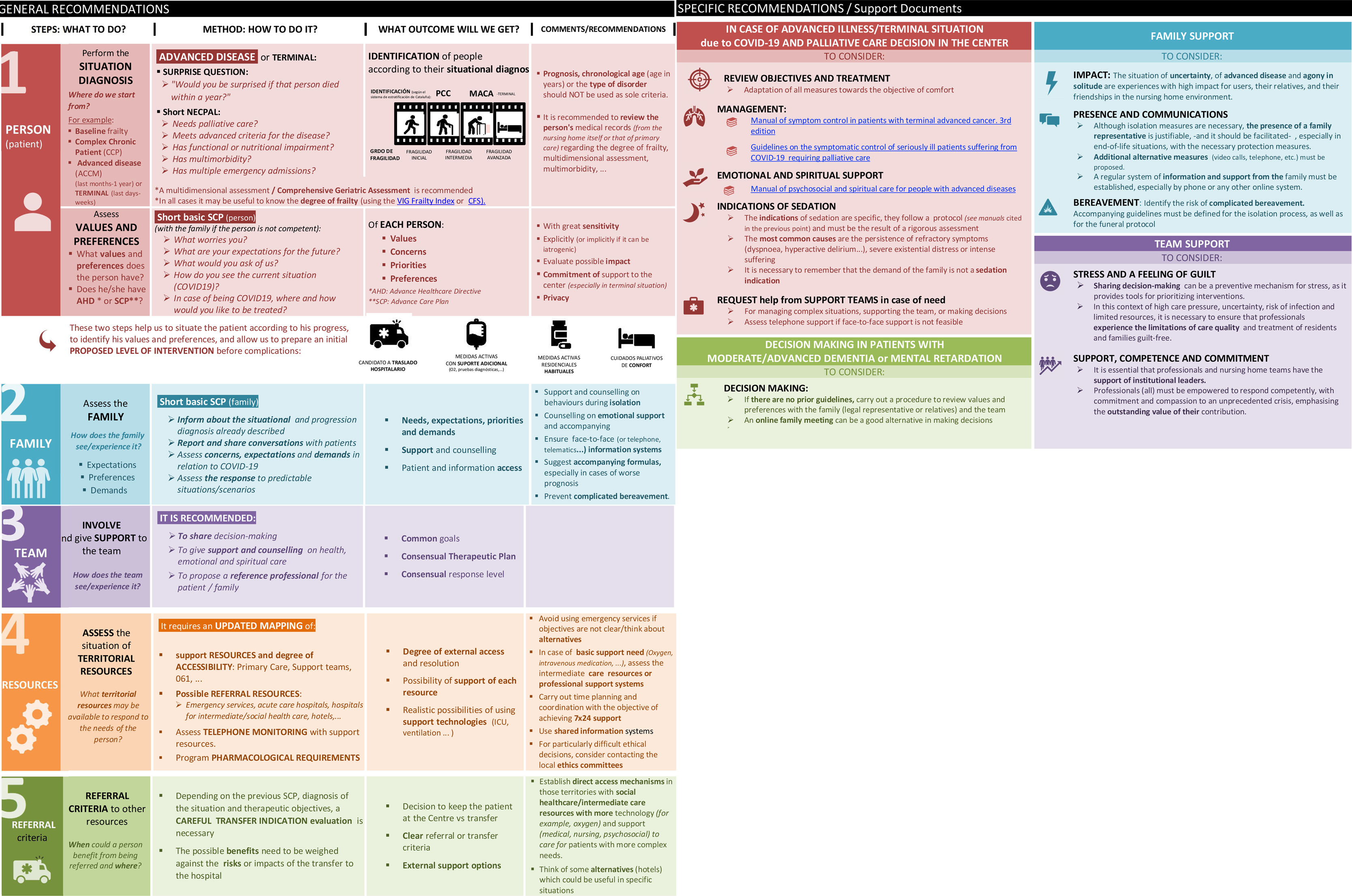
a) General recommendations5 assessment and intervention steps were identified (person, family, team, territory resources and referral criteria), for which the following were described: 1) the steps (what to do); 2) the method (how to do it); 3) the expected outcome, and 4) a series of related practical recommendations (comments) (Fig. 1).
The assessment of the person included the diagnosis of the previous situation - which should go far beyond the chronological age of the person5 – as well as the identification of their values and preferences. In the section on the family, the need to examine their values, preferences and expectations was also highlighted; in the section on the team, the need to encourage their participation was identified, as well as their support in the assessment and decision making. In the analysis of territorial resources, the need to identify available external resources was highlighted, as well as the need for the intervention of support teams or admission criteria and intervention in the external resources.
This information should provide the identification of criteria that facilitate the decision-making process, including the preferred place of care (nursing home with internal resources or additional external support, or referral to another facility).
b) Specific recommendationsIn this section, four worksheets were designed with a pragmatic approach, with the aim of responding to specific and prevalent situations: the first proposed palliative care measures in those cases where an advanced or terminal disease situation was identified without criteria for referral, and a proposal for care at the centre itself. The second worksheet outlined a series of recommendations for the support and assistance of the family, with criteria for support, presence, and bereavement support. They were complemented with recommendations for the care and decision-making of people with dementia, as well as measures to support the team for the prevention of stress, burnout, compassion fatigue or guilt (Fig. 1).
Consensus process with scientific societies and organizationsThe preliminary document was submitted for review and acceptance by the 12 scientific societies, 5 bioethics entities or their chairmen, as well as 15 organizations -including professional associations, employers' associations, research and administration groups— (Table 1), who also made valuable contributions, finally obtaining a definitive consensus (Fig. 1).
DiscussionFaced with the current COVID-19 pandemic, ethical and clinical decisions in nursing-homes are the core element on which to build quality, people-centred and equitable care. In this context, specific recommendations are essential to guide professionals in the difficult decision-making process, a fact that can ultimately help reduce collateral damage.5,14
This document describes and organises a process that begins with the individualised assessment of the residents (and their needs and preferences), incorporating the family and the team as key players, as well as an evaluation of the territorial resources and their accessibility and referral criteria.
Despite the limitations derived from the scarce specific literature on decision-making in a nursing home environment in the current COVID-19 pandemic, as well as the numerous entities and professionals participating in this work, the methodological design in three stages has made it possible to develop a broad consensus in less than two weeks. There is no precedent in the published literature for a document of this nature, with such a broad consensus and with such a pragmatic and field-oriented approach. Most of the articles reviewed either focus on very specific aspects (epidemiology,7 clinical features,4 organizational aspects,7 palliative care,11,12 individual opinions,5 for example) or are published by working groups or isolated scientific societies.9,10
Decisions made in this uncertain present will, in the short and medium term, have a significant impact on patients, families and care professionals, which can sometimes be as or more devastating than the disease itself.15 May these recommendations shed light to help build a future that will hopefully be better and more collaborative.
Conflict of interestsThe authors declare no conflict of interest.
We wish to thank all the people and entities that have participated in this consensus. Also, our gratitude to all the professionals who, in a context of crisis, with limited internal and external resources, are doing everything possible to offer quality care to the users.
Professionals: Conxita Barbeta, Montse Blasco, Marc Antoni Broggi, Ester Busquets, Cristina Casanovas, Anna Casellas-Grau, Marta Chandre, Xavier Costa, Marina Geli, Alex Guarga, Angel Jover, Montse Llopis, Remedios Martín, Miquel Àngel Mas, Begoña Román, Pepa Romero, Sebastià Santaeugènia, Antoni Sisó, Núria Terribas
Organizations: Asociación de Bioética Fundamental y Clínica, Asociación Española de Enfermería en Cuidados Paliativos (AECPAL), Asociación Española de Planificación Compartida de la Atención (AEPCA), Associació Catalana de Recursos Assisencials (ACRA), Associació d'Infermeria Familiar i Comunitària de Catalunya (AIFiCC), Càtedra de Bioètica Universitat de Vic-UCC, Càtedra de Cures Pal·liatives - Universitat de Vic-UCC, Col·legi de Metges de Barcelona, Col·legi Oficial d’Infermeres i Infermers de Barcelona (COIB), Col·legi Oficial de Psicologia de Catalunya, Col·legi Oficial de Treball Social de Catalunya, Consell de Col·legis de Metges de Catalunya, Consorci de Salut i Social de Catalunya (CSSC), Federación de Asociaciones de Enfermería Comunitaria y Atención Primaria (FAECAP), Fundació Salut i Envelliment - Universitat Autònoma de Barcelona, Grup de Recerca en Cronicitat de la Catalunya Central (C3RG), Institut Borja de Bioètica. Universitat Ramon Llull, Institut Català de la Salut (ICS), Institut Català d’Oncologia, La Unió (Associació d’Entitats Sanitàries i Socials), Pla d’atenció Integrada Social i Sanitària (PAISS) - Generalitat de Catalunya, Servei Català de la Salut, Societat Catalana de Geriatria i Gerontologia (SCGG), Societat Catalana de Medicina Familiar i Comunitària (CAMFIC), Societat Catalana de Metges Generals i de Família (SEMG Cat), Societat Catalano-Balear de Cures Pal·liatives (SCBCP), Sociedad Española de Cuidados Paliativos (SECPAL), Sociedad Española de Medicina Familiar y Comunitaria (SEMFYC), Sociedad Española de Geriatría y Gerontología (SEGG), Sociedad Española de Medicina Geriátrica (SEMEG).
Please cite this article as: Amblàs-Novellas J, Gómez-Batiste X. Recomendaciones éticas y clínicas para la toma de decisiones en el entorno residencial en contexto de la crisis de COVID-19. Med Clin (Barc). 2020;155:356–359.
The professionals and organizations that have participated in the consensus recommendations are presented in Appendix A.