Lung transplantation (LT) has been considered an alternative therapeutic approach in terminal patients. However, this process in COPD is not controversy-free. This paper aimed to analyse 30-day mortality (PM) patterns and their risk factors in COPD patients undergoing LT.
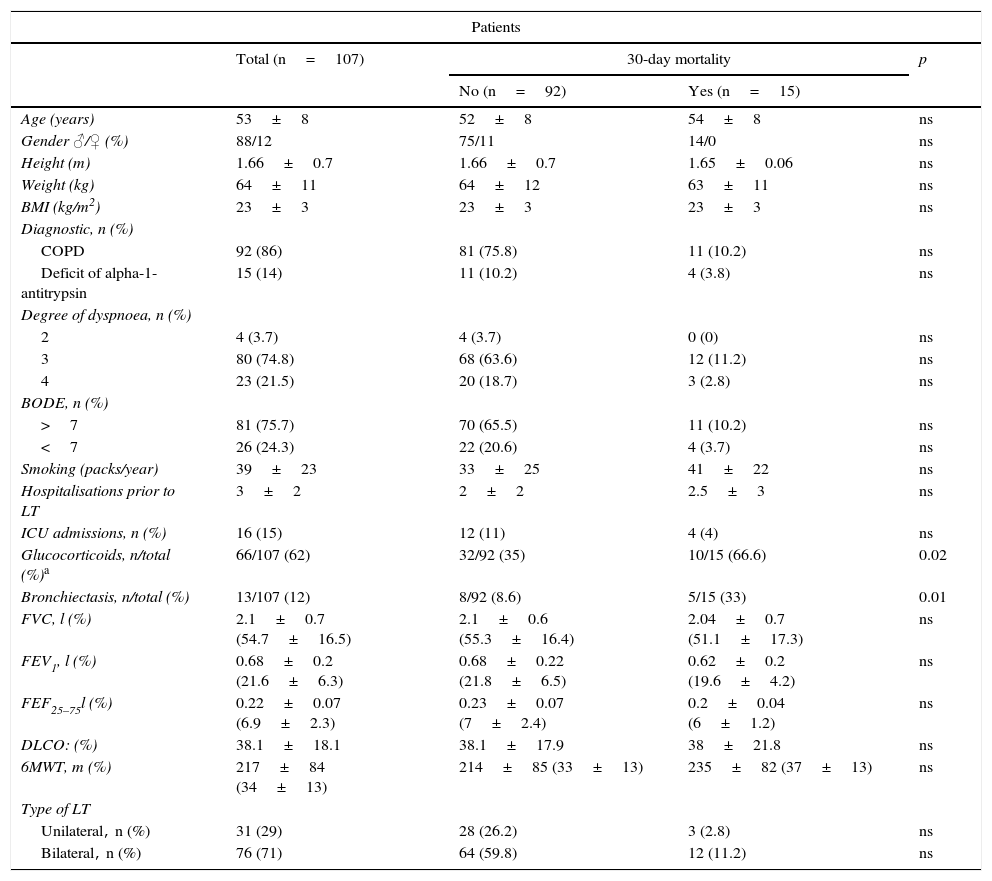
Patients and methodA retrospective cohort with 107 COPD patients, transplanted at the University La Fe Valencia, Spain, treated from January 1991 to December 2008. Demographics values, degree of dyspnoea, diagnosis, BODE index, single versus bilateral LT, cardio-pulmonary bypass, donor age, steroid dependence, presence of bronchiectasis, retrograde perfusion, transfusion of blood products, and PaO2/FiO2 were analysed. Continuous variables were expressed as mean±SD and categorical variables as absolute frequency and percentage. A Cox regression model was used for multivariate analysis.
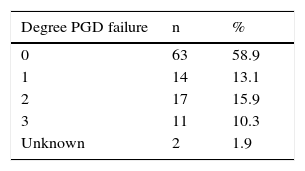
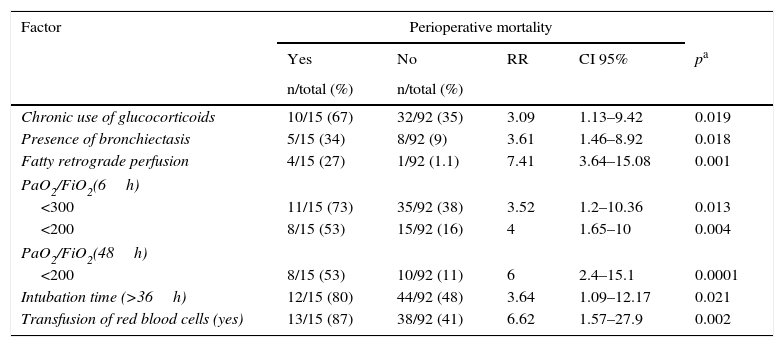
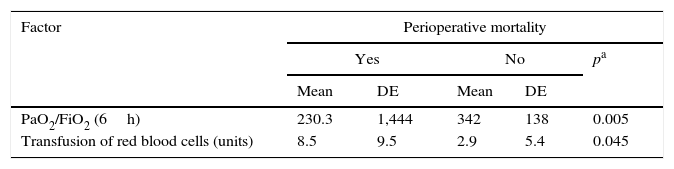
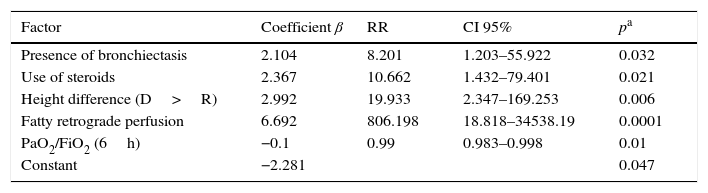
ResultsNinety-four men and 13 women of a mean age of 52.58±8.05 years were transplanted. Of all patients, 75% obtained a BODE score above 7. There were 76 bilateral LT. PM was established at 14%. Main causes of death were infection (53.3%) and surgical complications (33.3%). Presence of bronchiectasis and chronic use of corticosteroids, donor/recipient difference in size and presence of fat in retrograde perfusion fluid were important risk factors for PM. Moreover, PaO2/FiO2 ratio at 6h was a protective factor for the event, thus a higher ratio value, lowered the risk of PM.
ConclusionsLT is a procedure with a high PM rate. Use of corticosteroids, the presence of bronchiectasis and fat emboli in the retrograde reperfusion, and PaO2/FiO2 significantly determine PM.
El trasplante pulmonar (TP) es una alternativa terapéutica en pacientes con EPOC en fase terminal. Nuestro objetivo es analizar la mortalidad perioperatoria (30 días) (MP) y los factores de riesgo que la condicionan en pacientes con EPOC sometidos a TP.
Pacientes y métodoCohorte retrospectiva de 107 pacientes con EPOC trasplantados en el Hospital Universitario La Fe (1991-2008). Los datos demográficos, el grado de disnea, el diagnóstico, el índice BODE, el tipo de trasplante, la circulación extracorpórea, la edad del donante, la dependencia de glucocorticoides, la presencia de bronquiectasias, la reperfusión retrógrada, la transfusión de hemoderivados y la relación PaO2/FiO2 fueron analizadas. Las variables continuas se expresaron como media±DE y las categóricas, con frecuencias absolutas y porcentajes. El análisis multivariante se realizó mediante el modelo de regresión de Cox.
ResultadosSe trasplantaron 94 hombres y 13 mujeres con una edad media de 52,58±8,05 años. El 75% de los pacientes tuvieron un BODE≥7. Se realizaron 76 procedimientos bipulmonares. La MP fue del 14%. Las causas de muerte fueron las infecciones (53,3%) y las complicaciones quirúrgicas (33,3%). La presencia de bronquiectasias, el uso de glucocorticoides, la diferencia de talla entre receptor/donante y la presencia de émbolos grasos en la reperfusión retrógrada fueron factores de riesgo para la MP. La relación de PaO2/FiO2 a las 6h fue un factor protector para la MP.
ConclusionesEl TP es un procedimiento con una elevada tasa de MP. El uso previo de glucocorticoides, la presencia de bronquiectasias y de émbolos grasos en la reperfusión retrógrada, así como la PaO2/FiO2 condicionaron la MP.