An inverse relationship has been described between blood pressure and the prognosis in heart failure (HF). The characteristics of this relationship are not well unknown. The objective of this study was to determine if this relationship is maintained in a non-selected cohort of patients with HF and if it can be modified by treatment.
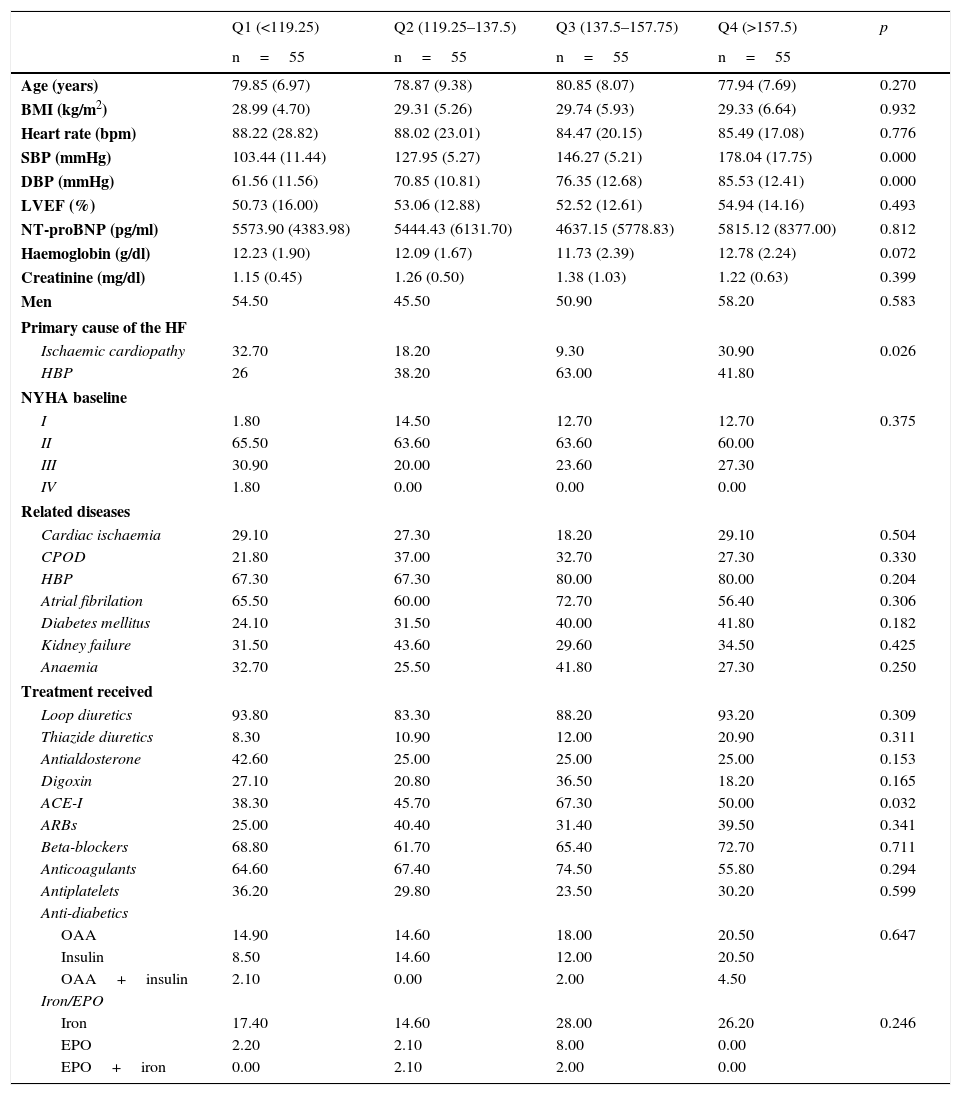
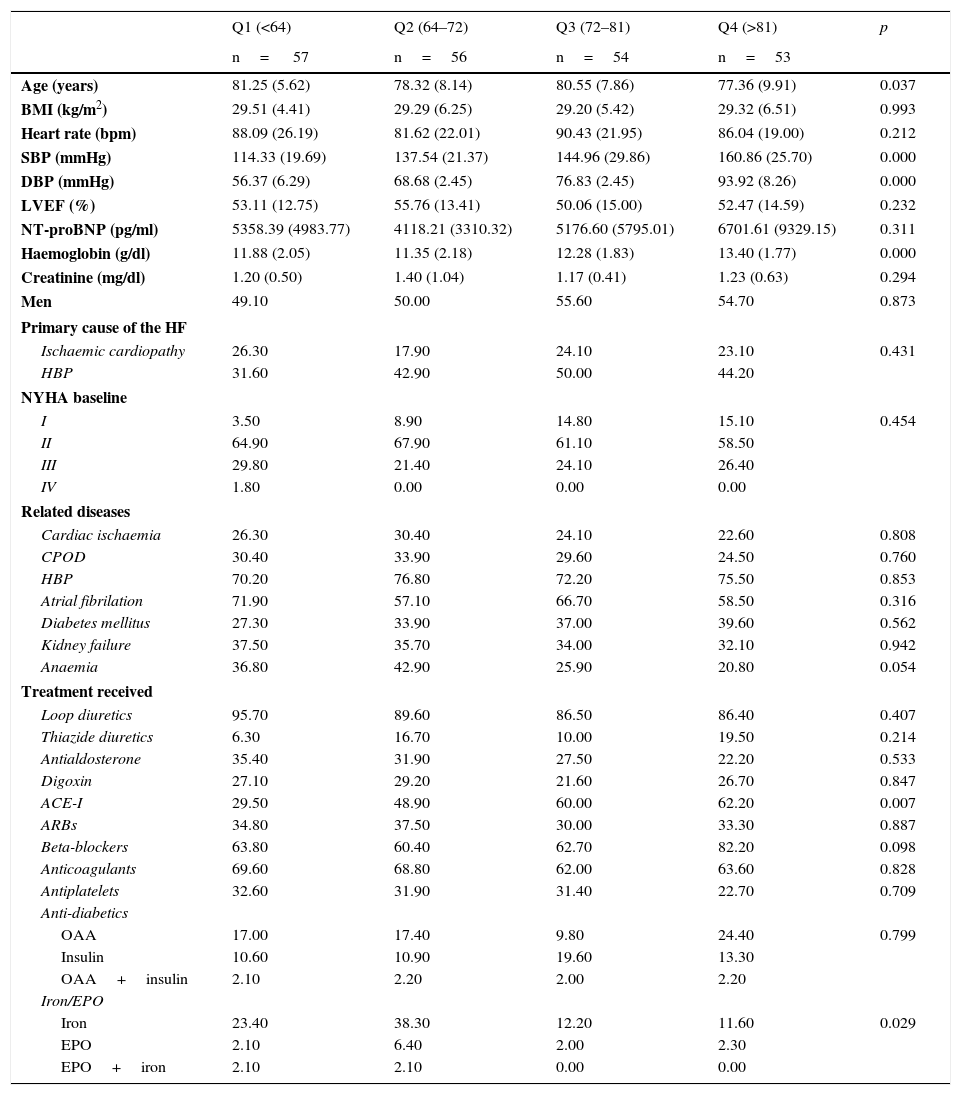
Material and methodsProspective study of cohorts including patients hospitalised for decompensated HF in Internal Medicine departments and followed as outpatients in a monographic consultation. Patients were classified according to their levels of systolic (SBP) and diastolic blood pressure (DBP). Clinical characteristics, all-cause mortality and readmissions after the first, third and sixth month of follow-up were analysed.
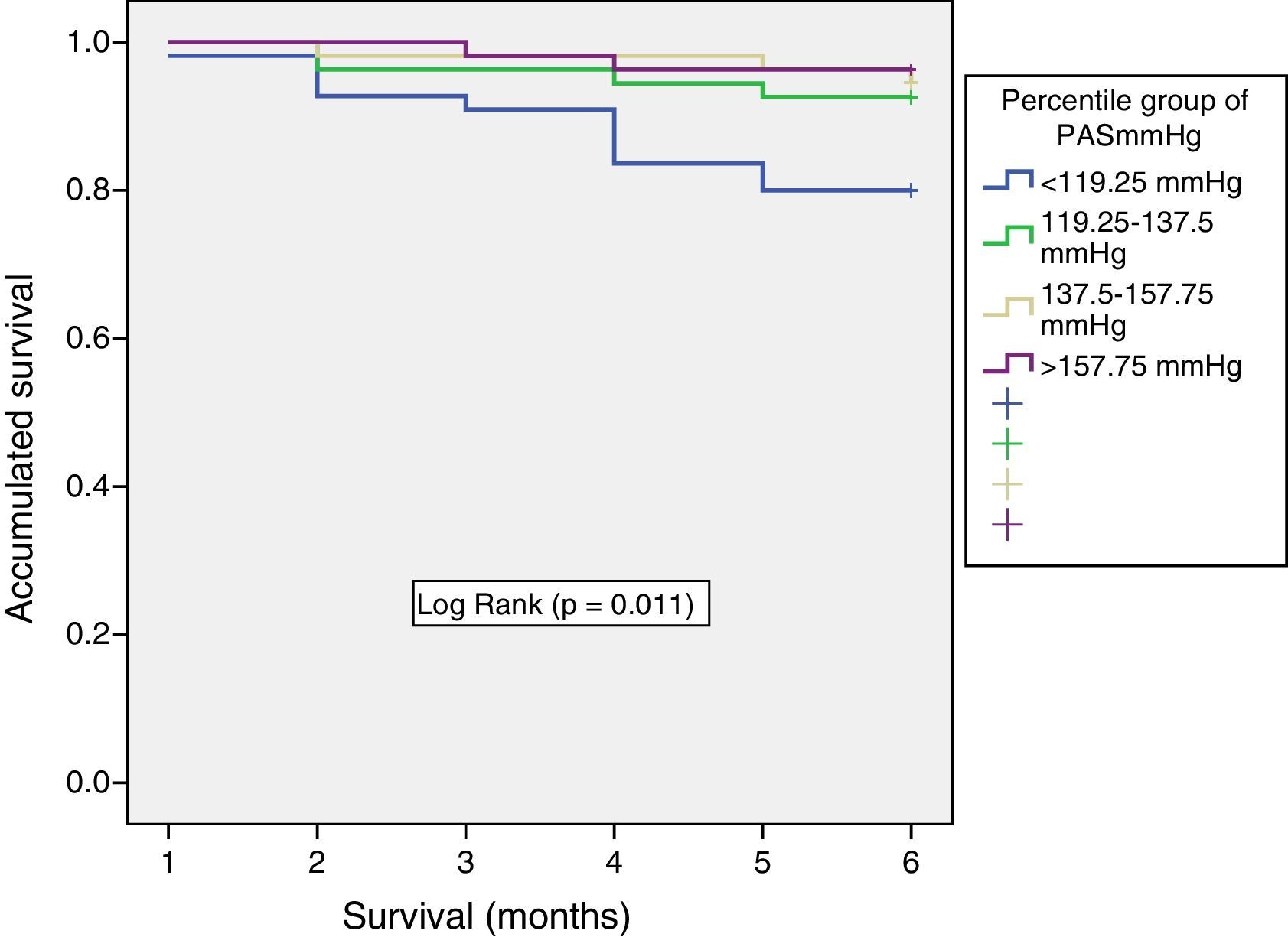
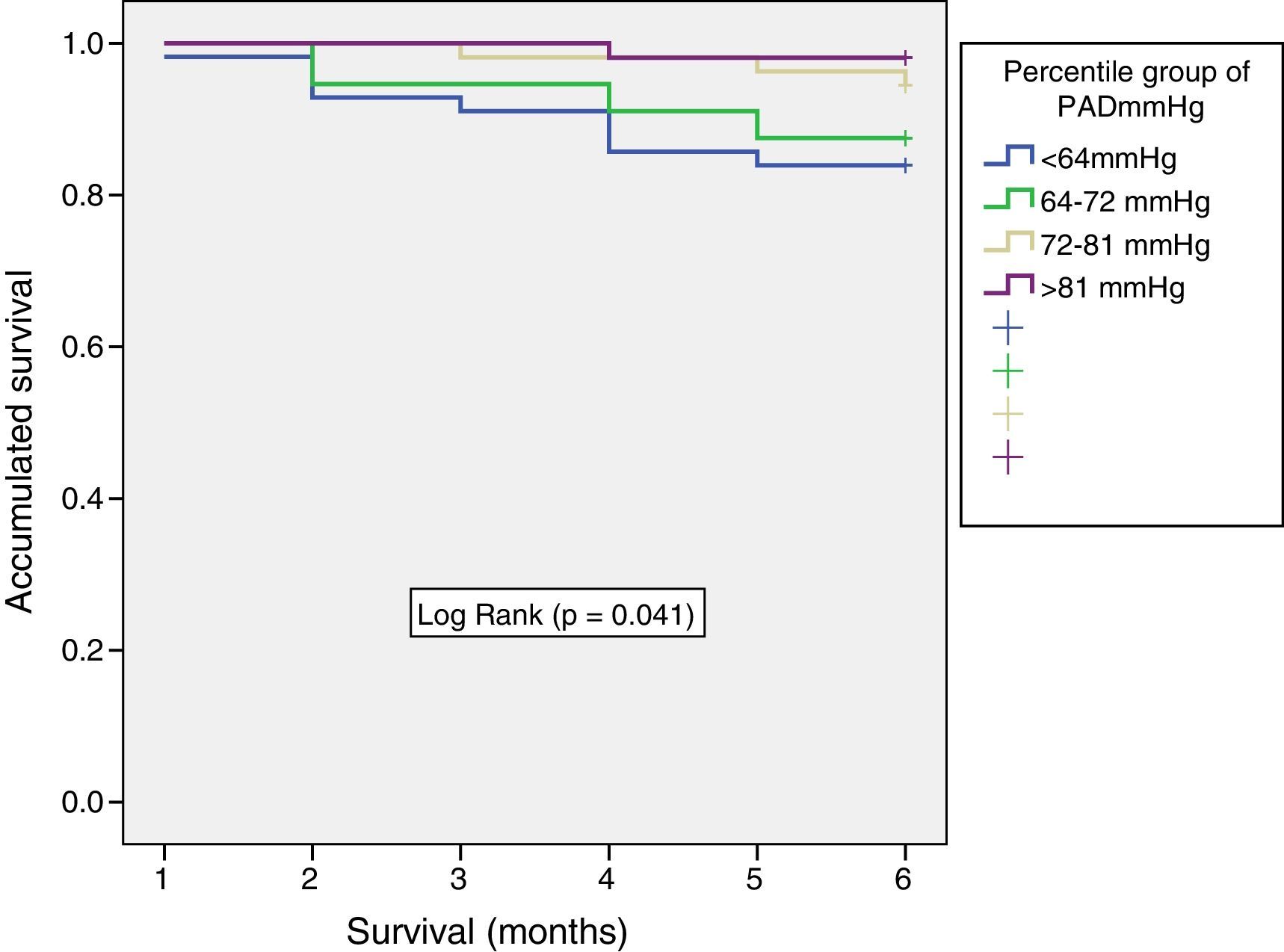
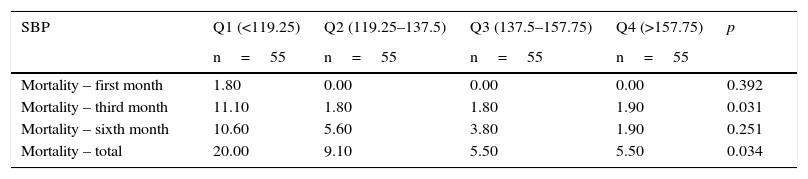
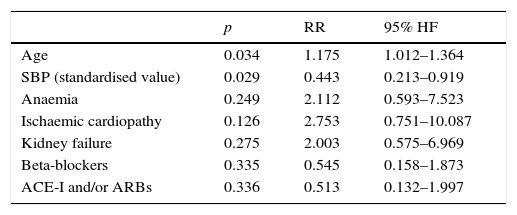
ResultsTwo hundred and twenty-one patients were included after their admission to the hospital for acute HF. Mean patient age was 79.5 years (SD 8.09); 115 patients were male. No significant differences between SBP quartiles and basal characteristics were found. Patients with lower SBP (Q1) had higher mortality rates (20%, p<0.05). No significant differences between mortality/readmissions and DBP were found. However, the Kaplan–Meier analysis showed higher all-cause mortality rates for the group of patients with lower SBP and DBP (log-rank=0.011 and 0.041, respectively). The pharmacological treatment did not differ significantly between both study groups.
ConclusionFor non-selected patients suffering HF, higher SBP upon the admission is associated with significantly lower all-cause mortality rates during follow-up. Pharmacological treatment of HF does not seem to influence this inverse relationship between SBP at admission and patient mortality.
Existe una relación inversa entre las cifras de presión arterial en las descompensaciones y el pronóstico de la insuficiencia cardiaca (IC). Las características de esta relación no son bien conocidas. El objetivo del estudio fue analizar si esta relación se mantiene en una cohorte no seleccionada de pacientes con IC y si el tratamiento la modifica.
Material y métodosEstudio prospectivo de cohortes de pacientes ingresados por IC descompensada en un servicio de Medicina Interna y seguidos ambulatoriamente en una consulta monográfica. Los pacientes fueron agrupados en función de la presión arterial sistólica (PAS) y diastólica (PAD); se analizaron las características clínicas, la mortalidad global y los reingresos al primer, tercer y sexto mes de seguimiento.
ResultadosSe incluyeron 221 pacientes tras un ingreso índice por IC. Media de edad: 79,5 años (DE 8,09); varones: 115. No hubo diferencias significativas en las características basales de los pacientes en función de los cuartiles de PAS. Los pacientes con menor PAS (Q1) tenían mayor mortalidad (20%, p<0,05). No se encontraron diferencias para la PAD. Sin embargo, el análisis de Kaplan-Meier mostró una mayor mortalidad global en los pacientes con menor PAS y PAD (log-rank=0,011 y 0,041, respectivamente). Las características del tratamiento farmacológico no diferían entre los grupos del estudio.
ConclusiónEn pacientes con IC no seleccionados, las cifras elevadas de PAS al ingreso se asocian con una menor mortalidad durante el seguimiento. El tratamiento farmacológico de la IC no parece influir en la relación inversa entre la PAS al ingreso y la mortalidad.