We aimed to explore the impact of the time interval between symptoms and diagnosis on post-operative infective endocarditis (IE) survival.
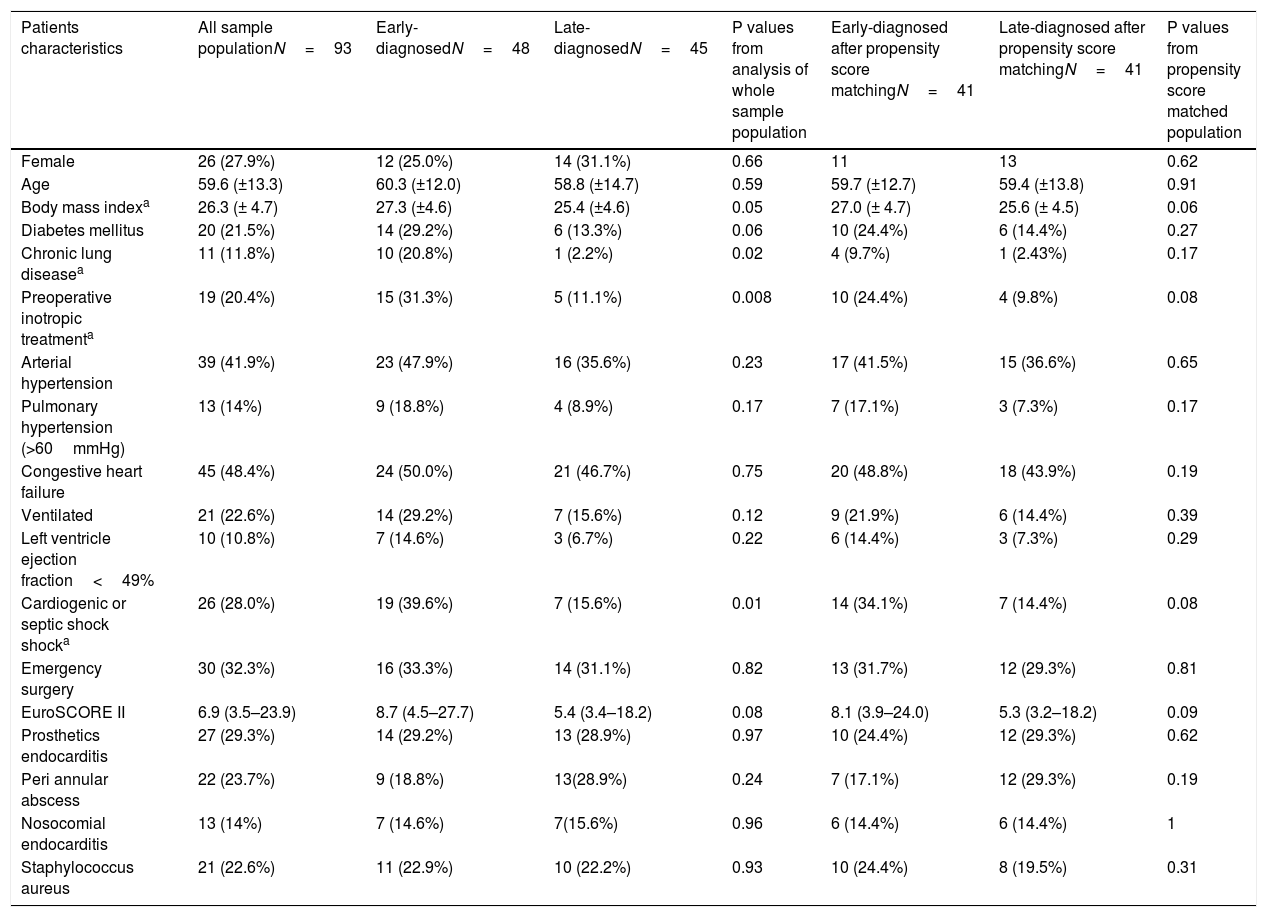
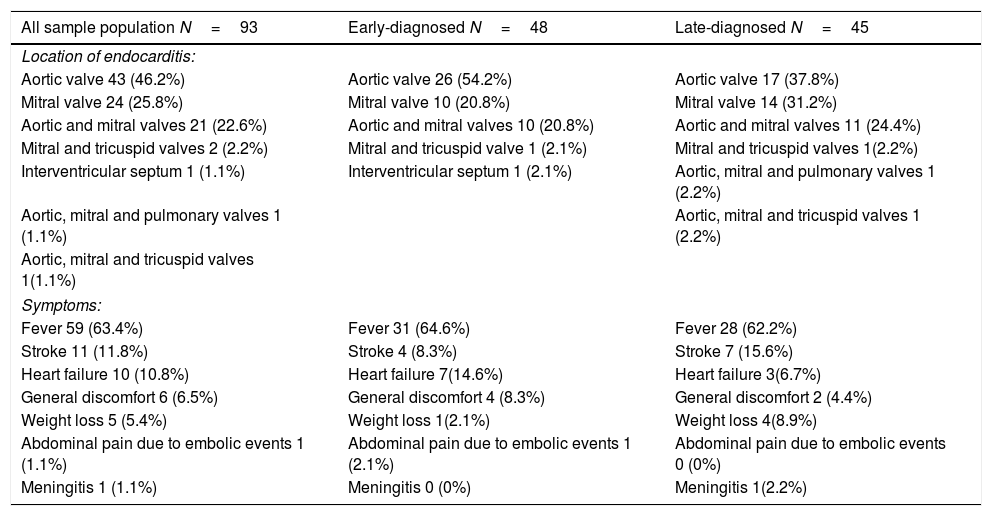
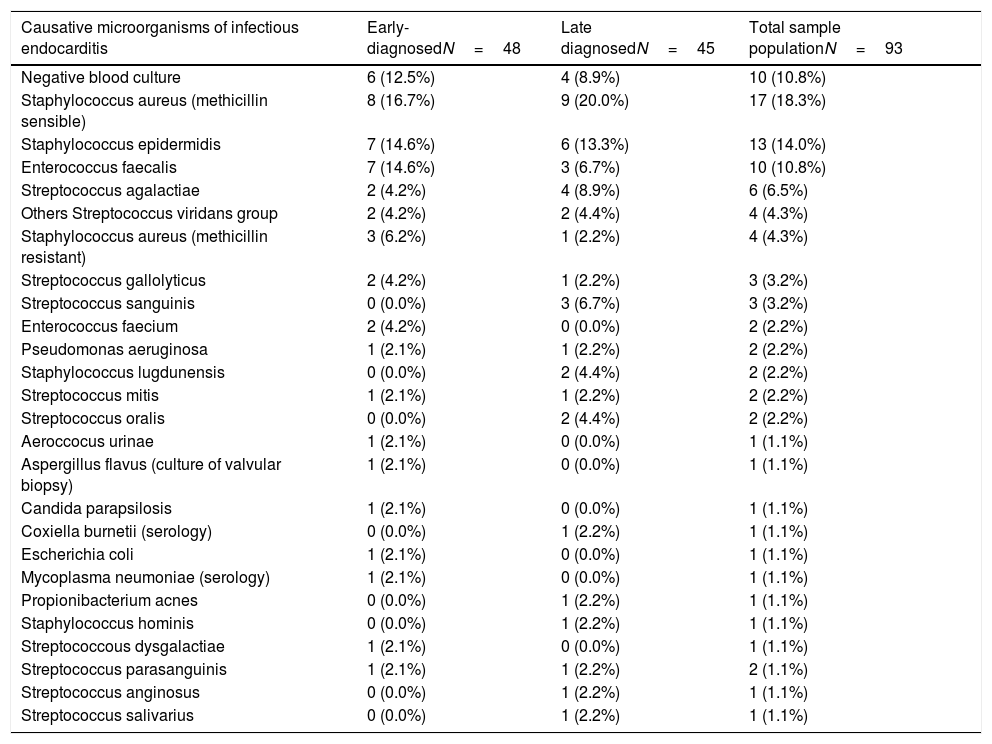
MethodsFrom 2014 to 2019, data from 93 consecutive patients undergoing cardiac surgery due to left-sided±right-sided IE were prospectively recorded in our specific electronic database.
Patients were classified into 2 groups according to time interval between first clinical symptoms and definitive endocarditis diagnosis: patients with early diagnosis (≤8 days) and patients with late diagnosis (>8 days). Follow-up was 100% complete, and follow-up mean time was 471 days.
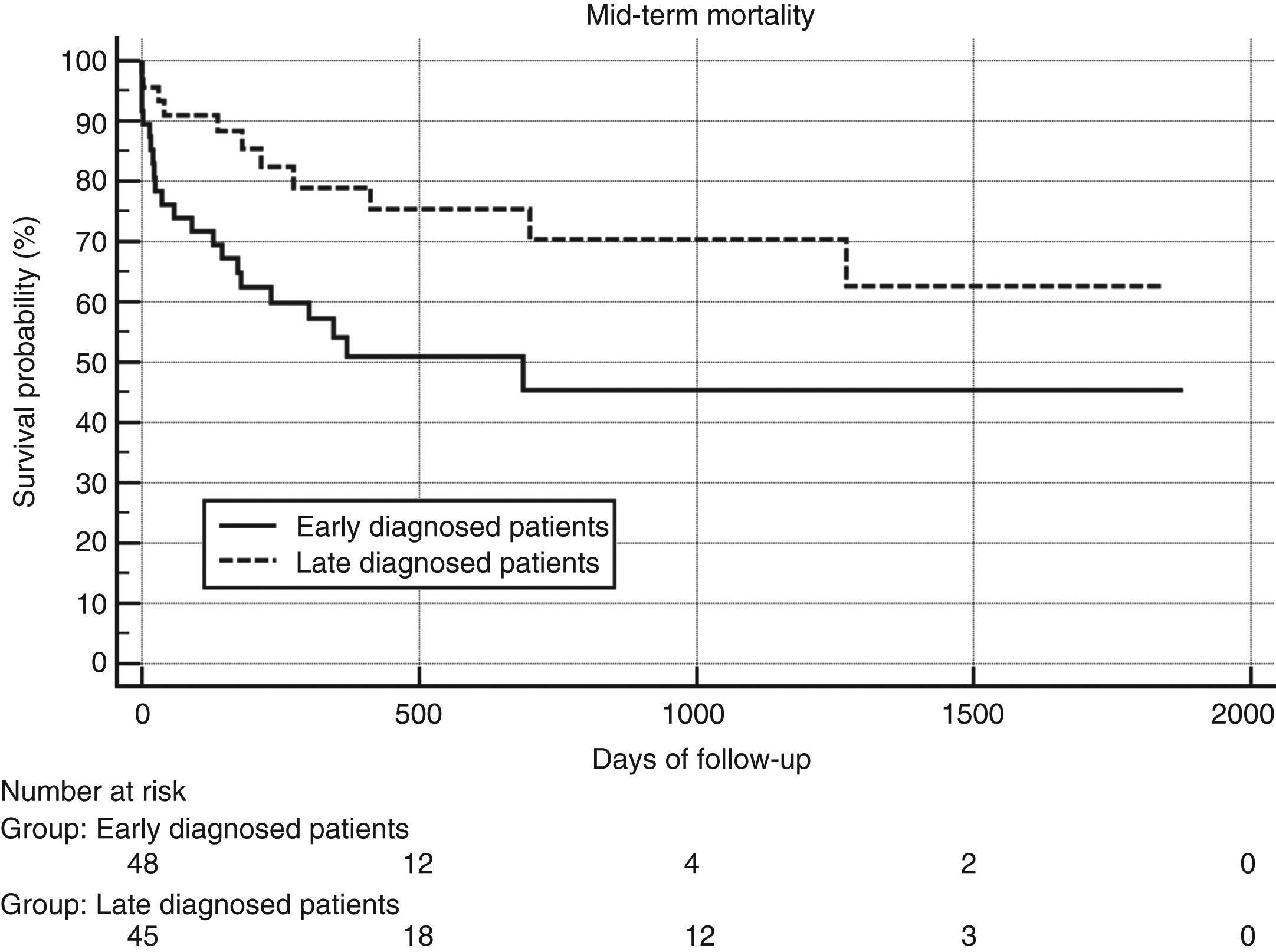
ResultsAmong the 93 patients undergoing cardiac surgery due to definite left-sided IE, 48 (51.6%) had early-diagnosed IE whereas 45 (48.4%) presented with a late-diagnosed IE. Unadjusted and propensity score adjusted mid-term survival Kaplan–Meier analysis showed significantly worse survival of patients belonging to the early-diagnosis group (p .019 and .049 respectively). Multivariable Cox regression analysis identified only one predictor of mid-term mortality: EuroSCORE II (Hazard ratio 1.03, 95% CI 1.01–1.05, p .0008).
ConclusionThe association in the Kaplan–Meier analysis between “early-diagnosis group” and mortality suggests that this group of patients presents clinical characteristics of severity that, on the one hand, speed up the diagnostic process and on the other, converge in the determination of a higher euroSCORE II value, which is the only independent predictor of mid-term mortality according to our analysis.
Nuestro objetivo fue explorar el impacto del intervalo de tiempo entre los síntomas y el diagnóstico en la supervivencia postoperatoria de la endocarditis infecciosa (EI).
MétodosDe 2014 a 2019, los datos de 93 pacientes consecutivos intervenidos de cirugía cardíaca por EI definitiva izquierda±derecha se registraron prospectivamente en nuestra base de datos electrónica.
Los pacientes se clasificaron en 2 grupos según el intervalo de tiempo entre los primeros síntomas clínicos y el diagnóstico definitivo de endocarditis: pacientes con diagnóstico temprano (≤propensity score: 8 días) y pacientes con diagnóstico tardío (>propensity score: 8 días). El seguimiento fue del 100% completo, y el tiempo medio de seguimiento fue de 471 días.
ResultadosEntre los 93 pacientes que se sometieron a cirugía por EI definitiva del lado izquierdo, 48 (51,6%) tenían un diagnóstico temprano de EI, mientras que 45 (48,4%) presentaban un diagnóstico tardío de EI. El análisis de Kaplan-Meier no ajustado y el ajustado con propensity score mostró una supervivencia significativamente peor de los pacientes que pertenecen al grupo de diagnóstico temprano (p 0,019 y 0,049, respectivamente). El análisis de regresión de Cox multivariable identificó solo un predictor de mortalidad a medio plazo: EuroSCORE II (razón de riesgo: 1,03; IC 95%: 1,01-1,05; p 0,0008).
ConclusiónLa asociación en el análisis de Kaplan-Meier entre «diagnóstico temprano de EI» y mortalidad sugiere que este grupo de pacientes presenta características clínicas de gravedad que, por un lado aceleran el proceso diagnóstico, y por el otro confluyen en la determinación de un EuroSCORE II más alto, que sí es un predictor independiente de mortalidad.