The impact of an admission to ICU before stem cell transplantation (SCT) on post-SCT outcome is not well established.
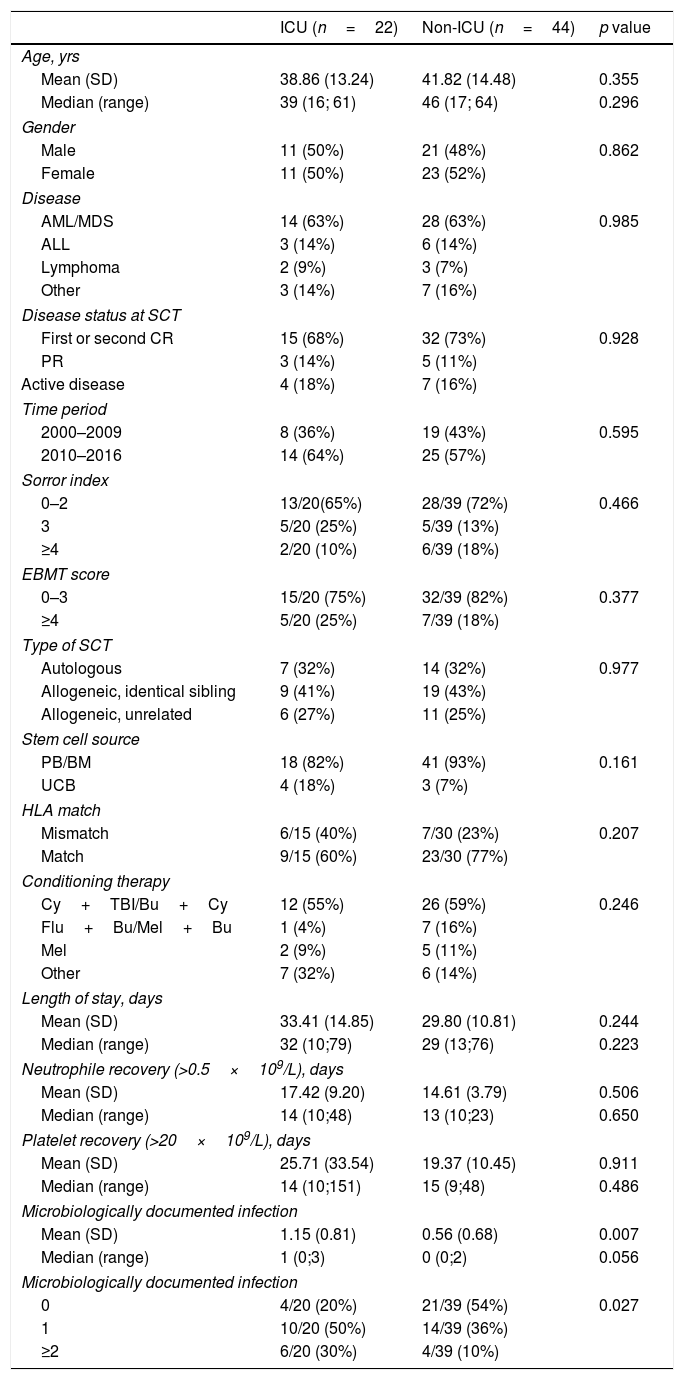
Patients and methodsWe reviewed the medical records of patients who had received a first SCT between 2000 and 2016 in our institution. The outcome of 22 patients who required ICU admission during chemotherapy prior to SCT (ICU group) was compared with 44 matched patients (1:2) who did not need it (NO-ICU group).
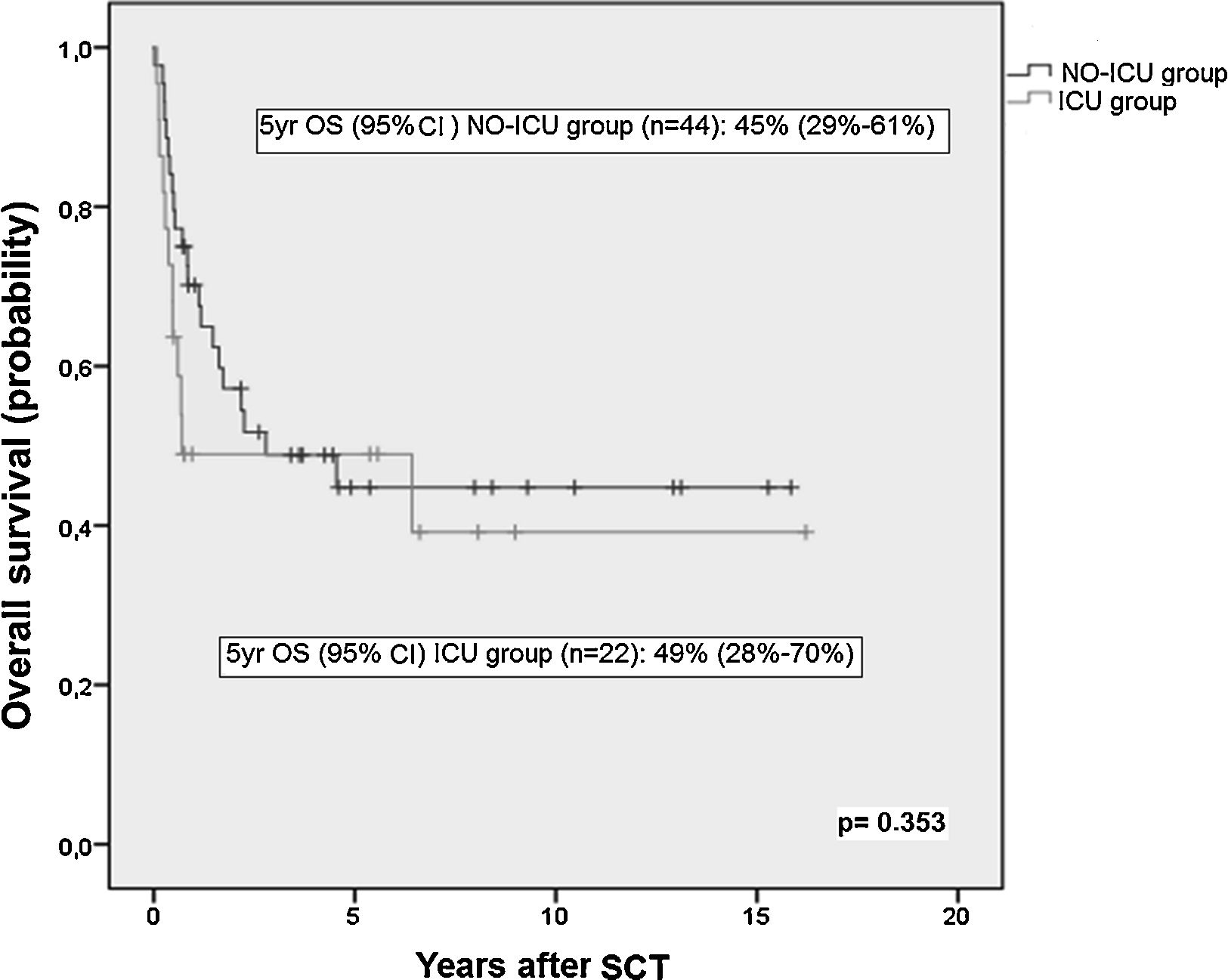
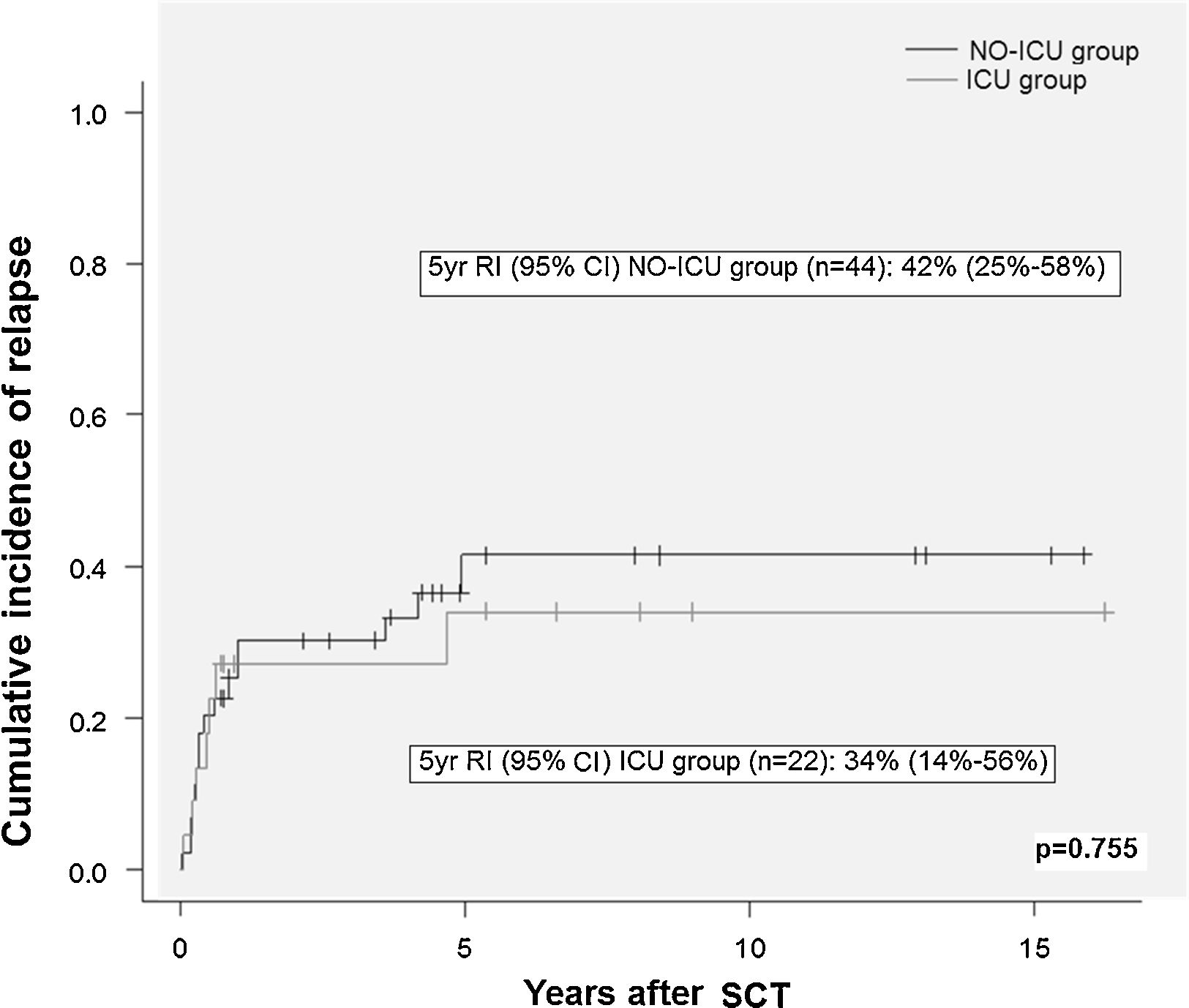
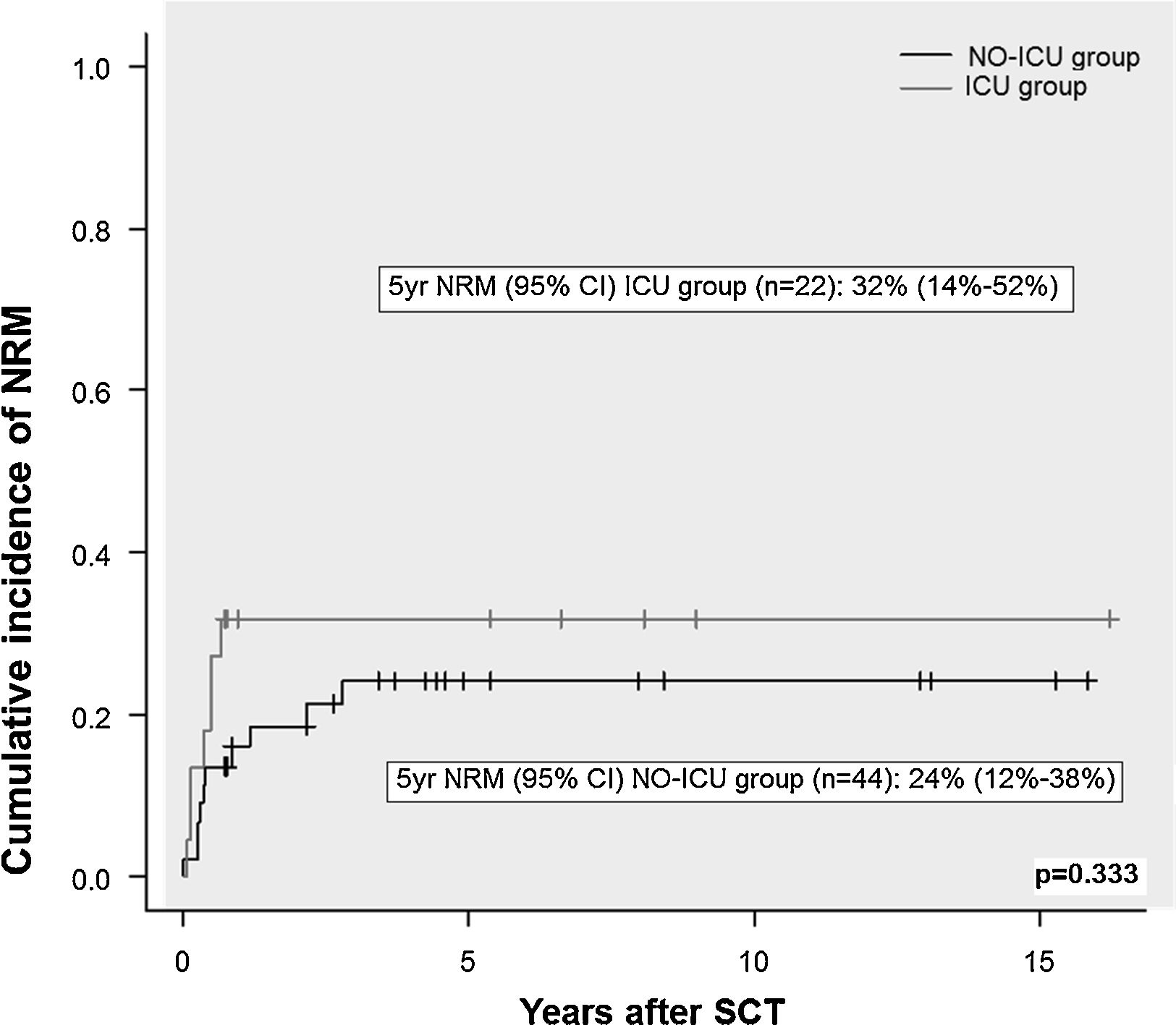
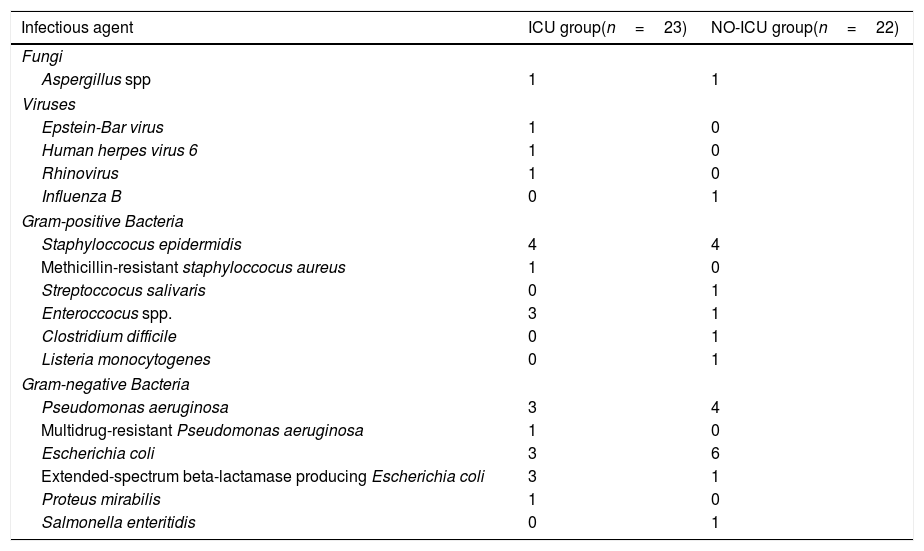
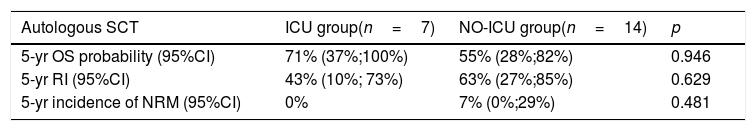
ResultsThere were no differences in transplant complications, in time to neutrophil and platelet recovery or in the length of hospital stay during SCT between the ICU and NO-ICU groups. However, microbiologically documented infections were more common in the ICU group (16/20) than in the NO-ICU group (18/39) (p=.027). The 5-yr overall survival probability (CI 95%) was 49% (28–70%) in the ICU vs. 45% (29–61%) in the NO-ICU group (p=.353), while the 5-yr incidence of non-relapse mortality was 32% (14–52%) and 24% (12–38%) (p=.333), respectively. Six patients (27%) in the ICU group and 8 (18%) in the NO-ICU group required admission to the ICU during or after the SCT procedure (p=.293). Twelve (54%) patients in the ICU and 22 (50%) in the NO-ICU group died, the causes of death were similar in both groups.
ConclusionOur results show that admission to the ICU prior to SCT does not have a negative impact on patient outcomes following SCT and should not be considered as an exclusion criterion for SCT.
No se conoce con exactitud el impacto de la necesidad de ingreso previo en una unidad de cuidados intensivos (UCI) en la supervivencia postrasplante de progenitores hematopoyéticos (TPH).
Pacientes y métodosSe revisaron los archivos de pacientes que habían recibido un TPH entre el 2000 y 2016 en una única institución. El resultado del TPH en 22 pacientes que habían precisado de ingreso en una UCI durante las quimioterapias administradas previas al TPH (grupo UCI) se comparó con el de 44 pacientes controles (1:2) trasplantados que no habían precisado ingreso previo en UCI (grupo NO-UCI).
ResultadosNo hallamos diferencias en las complicaciones post-TPH, en el tiempo de injerto de neutrófilos o de plaquetas, ni tampoco en la duración del ingreso hospitalario entre el grupo UCI y el grupo NO-UCI (p=0,353). Sin embargo, la incidencia de infecciones documentadas microbiológicamente fue mayor en el grupo UCI (16/20) que en el NO-UCI. La probabilidad de supervivencia a 5 años (IC95%) fue del 49% (28-70%) para el grupo UCI vs. el 45% (29-61%) para el grupo NO-UCI (p=0,353), mientras que la mortalidad relacionada con el TPH a los 5 años fue del 32% (14-52%) y 24% (12-38%) (p=0,333), respectivamente. Seis pacientes (27%) en el grupo UCI y 8 (18%) en el grupo NO-UCI precisaron ingreso en UCI durante o después del proceso de TPH (p=0,293). Doce pacientes (54%) en el grupo UCI y 22 (50%) en el NO-UCI fallecieron, y las causas de muerte fueron similares en ambos grupos.
ConclusiónEl ingreso en UCI no tiene necesariamente un impacto negativo en los resultados de un TPH posterior en pacientes hematológicos y no debería ser criterio de exclusión para dicho procedimiento.