To analyse the differences in the cardio-metabolic profile of patients with primary aldosteronism (PA) and autonomous cortisol secretion (ACS) matched by age and sex.
MethodsCase-control study; cases of PA without associated ACS and as controls patients with ACS (dexamethasone suppression test ≥1.8 μg/dL in the absence of specific hypercortisolism clinical data), matched by age and sex. Comorbidities of hypertension, diabetes, obesity, dyslipidaemia, chronic kidney failure, and cardiovascular and cerebrovascular events were analysed, as well as their degree of control.
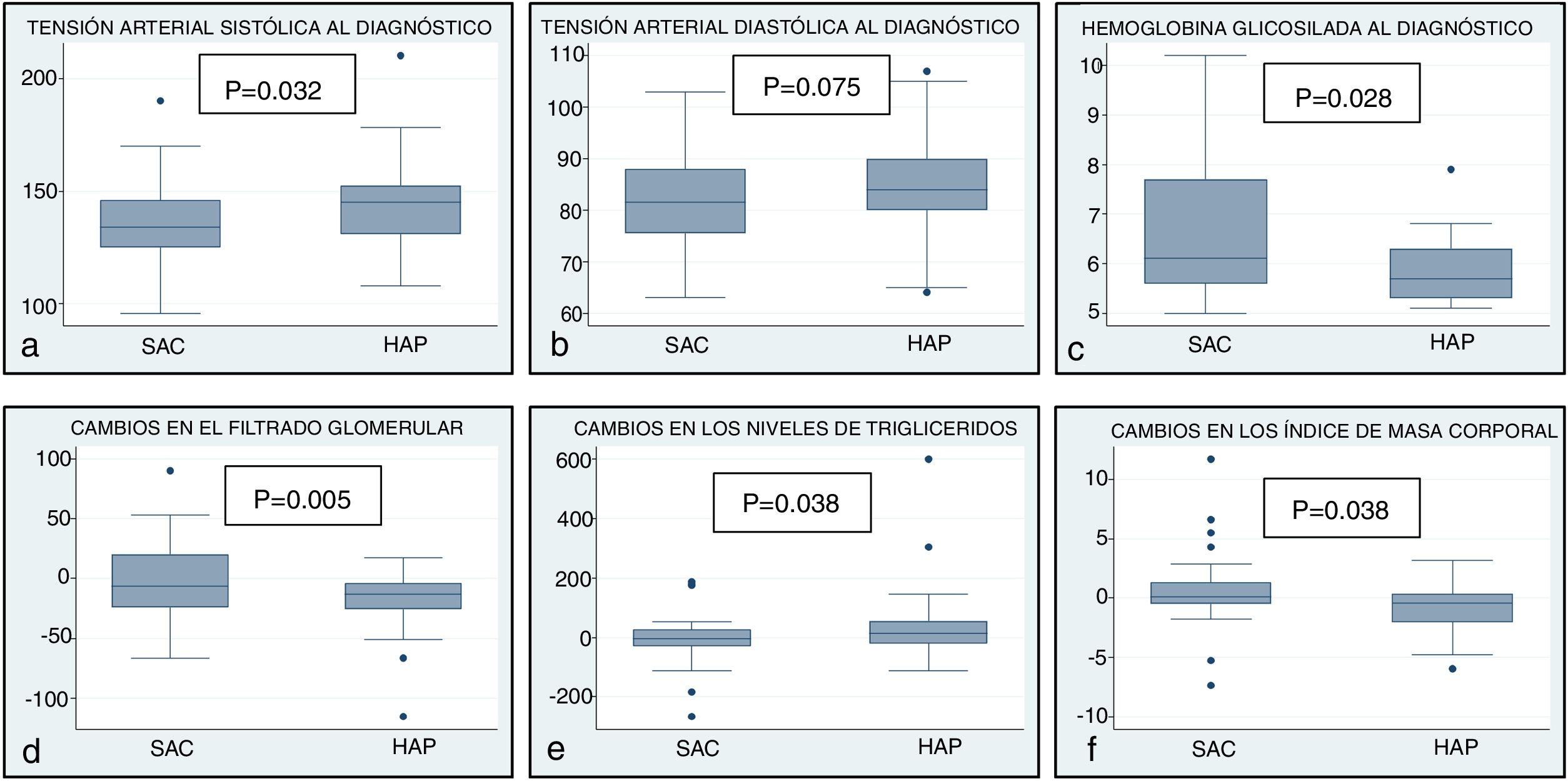
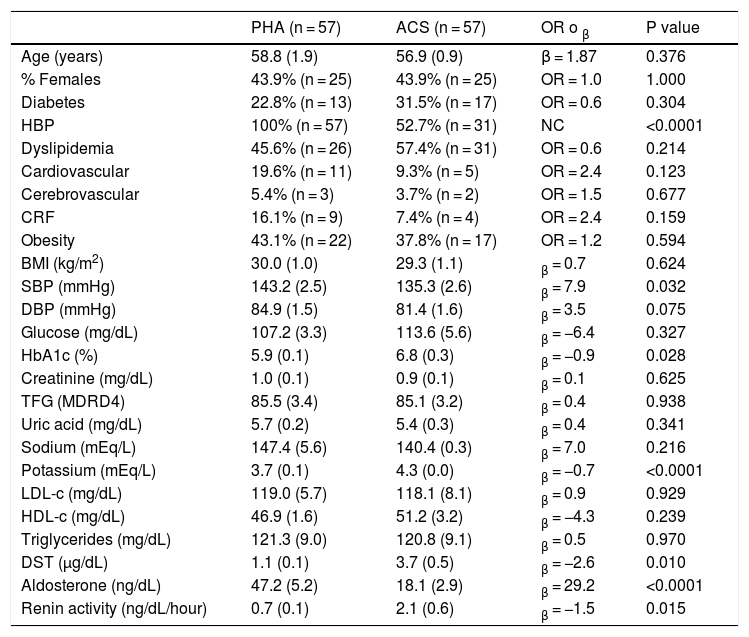
Results57 patients with PA and 57 with ACS were included. On diagnosis, in addition to a higher prevalence of hypertension in the PA patients (100 vs. 52.7%, p < .0001) and higher systolic blood pressure levels (143.2 (2.5) vs. 135.3 (2.6) mmHg, p = .032) than in the ACS patients, no other differences were detected in the prevalence of other cardio-metabolic comorbidities. Nevertheless, the patients with ACS had higher HbA1c levels (p = .028) than the PA patients.
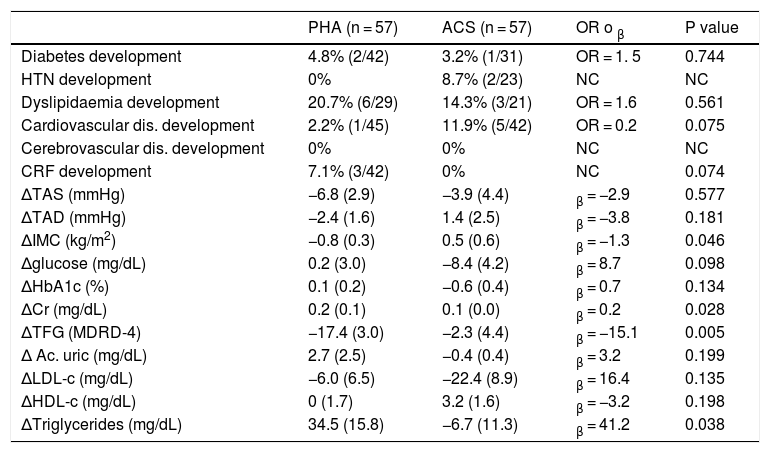
After a median follow-up of 2.25 years, the patients with PA presented a greater deterioration in kidney function (Average decrease in glomerular filtration rate (MDRD-4) −17.4 (3.0) vs. −2.3 (4.4) mL/min/1.73 m2, p = .005) and lipid profile (Δtriglycerides of 34.5 (15.8) vs. −6.7 (11.3) mg/dL, p = .038) than the ACS patients.
ConclusionsDespite the higher prevalence of hypertension in the patients with PA than in the patients with ACS matched by age and sex, no differences were detected in the prevalence of other cardio-metabolic comorbidities. However, the PA patients showed a greater deterioration in kidney function and lipid profile throughout the follow-up than the ACS patients.
Analizar las diferencias en el perfil cardiometabólico de los pacientes con hiperaldosteronismo primario (HAP) y secreción autónoma de cortisol (SAC), emparejados por edad y sexo.
MétodosEstudio de casos y controles; casos de HAP sin SAC asociada y como controles, pacientes con SAC (test de supresión de dexametasona ≥1.8 μg/dL en ausencia de datos específicos de hipercortisolismo), emparejados por edad y sexo. Se analizaron las comorbilidades HTA, diabetes, obesidad, dislipemia, insuficiencia renal crónica y eventos cardiovasculares y cerebrovasculares, así como su grado de control.
ResultadosSe incluyeron 57 pacientes con HAP y 57 con SAC. Al diagnóstico, aparte de una mayor prevalencia de HTA en los pacientes con HAP (100 vs. 52,7%, p < 0,0001) y niveles más altos de TAS (143,2 [2,5] vs. 135,3 [2,6] mmHg, p = 0,032) que en SAC, no se detectaron diferencias en la prevalencia de otras comorbilidades. No obstante, los pacientes con SAC presentaban cifras más elevadas de HbA1c (p = 0,028).
Tras una mediana de seguimiento de 2,25 años, los pacientes con HAP presentaron un mayor deterioro de la función renal (descenso medio del filtrado glomerular [MDRD-4] −17,4 [3] vs. −2,3 [4,4] mL/min/1,73 m2, p = 0,005) y del perfil lipídico (Δtriglicéridos de 34,5 [15,8] vs. −6,7 [11,3] mg/dL, p = 0,038) que los SAC.
ConclusionesA pesar la mayor prevalencia de HTA en los pacientes con HAP que con SAC, emparejados por edad y sexo, no se detectaron diferencias en la prevalencia de otras comorbilidades cardiometabólicas. No obstante, los HAP presentaron un mayor deterioro de la función renal y del perfil lipídico a lo largo del seguimiento que el grupo de SAC.