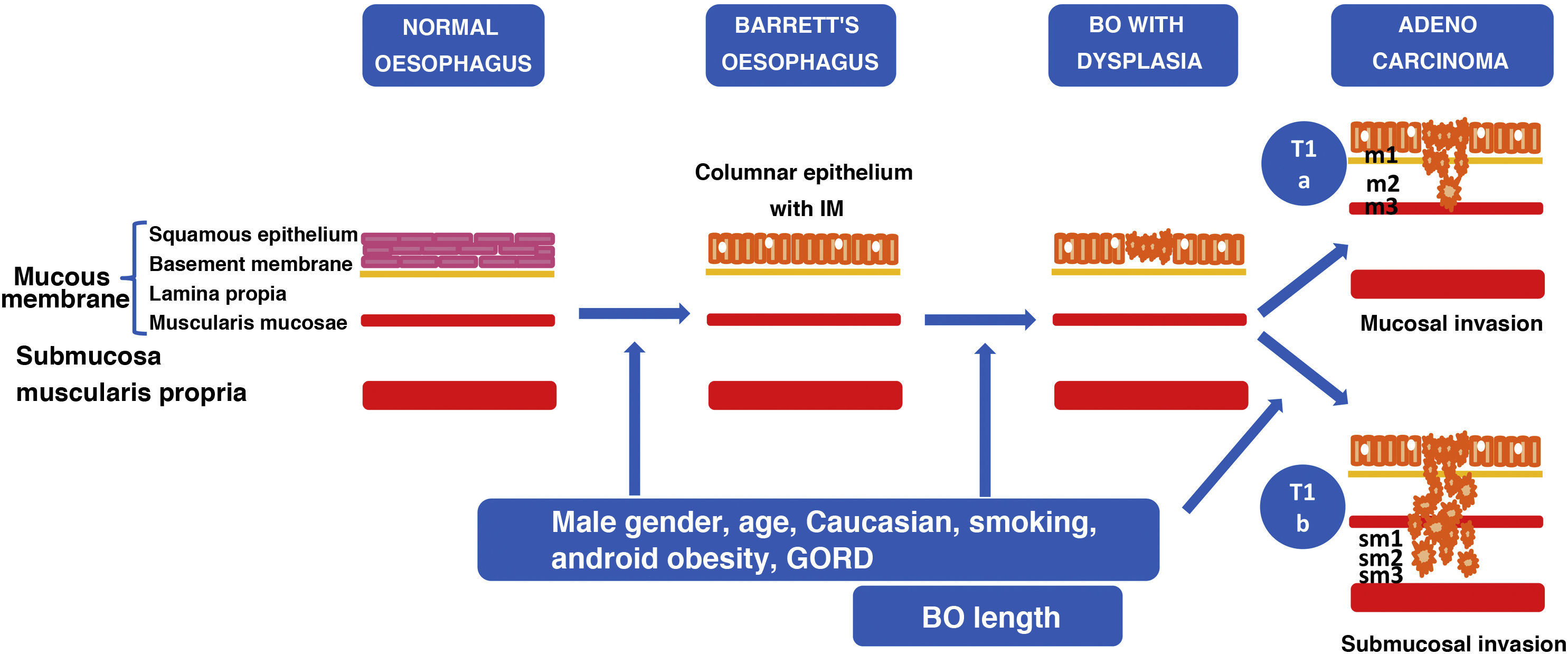
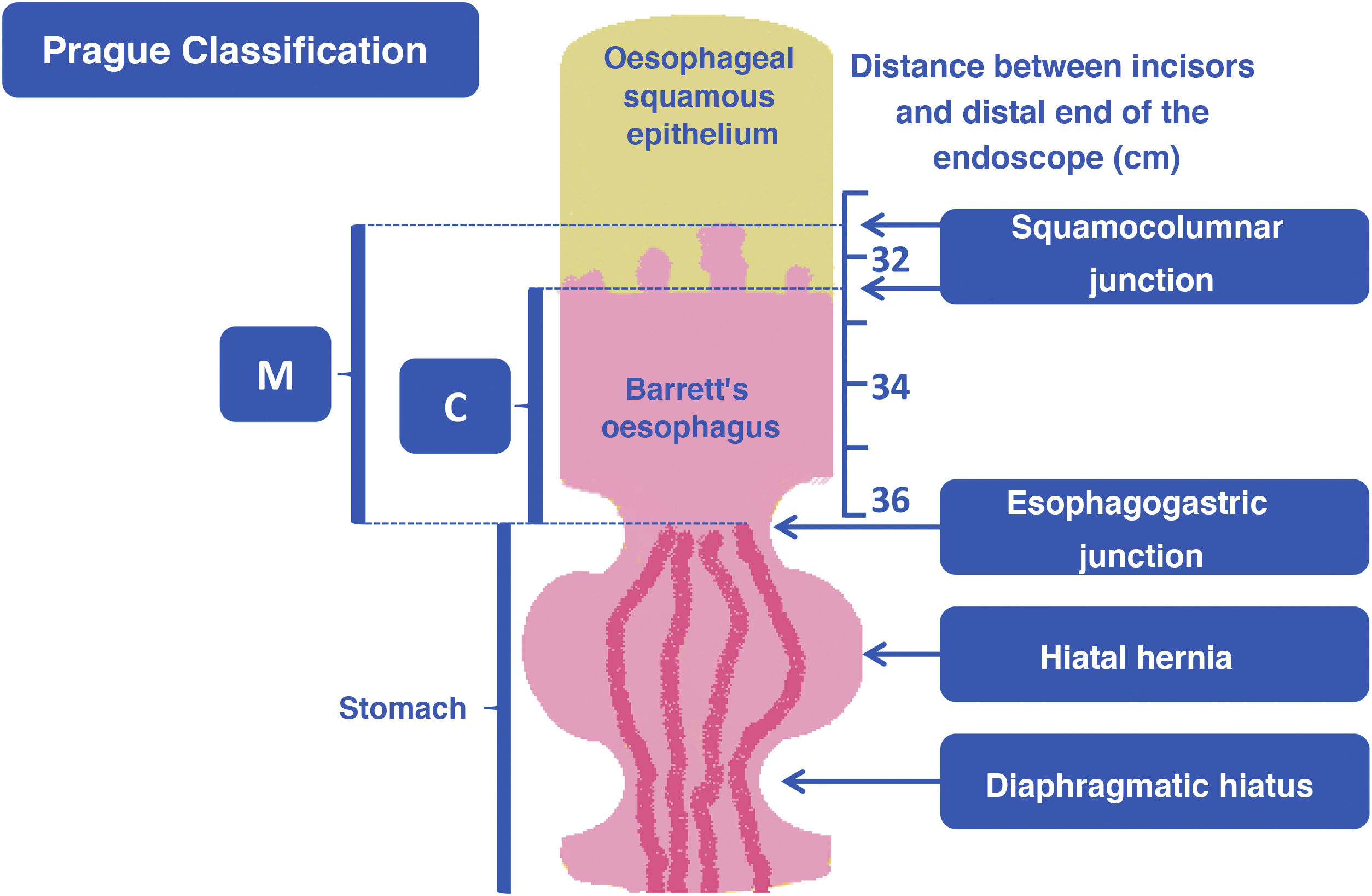
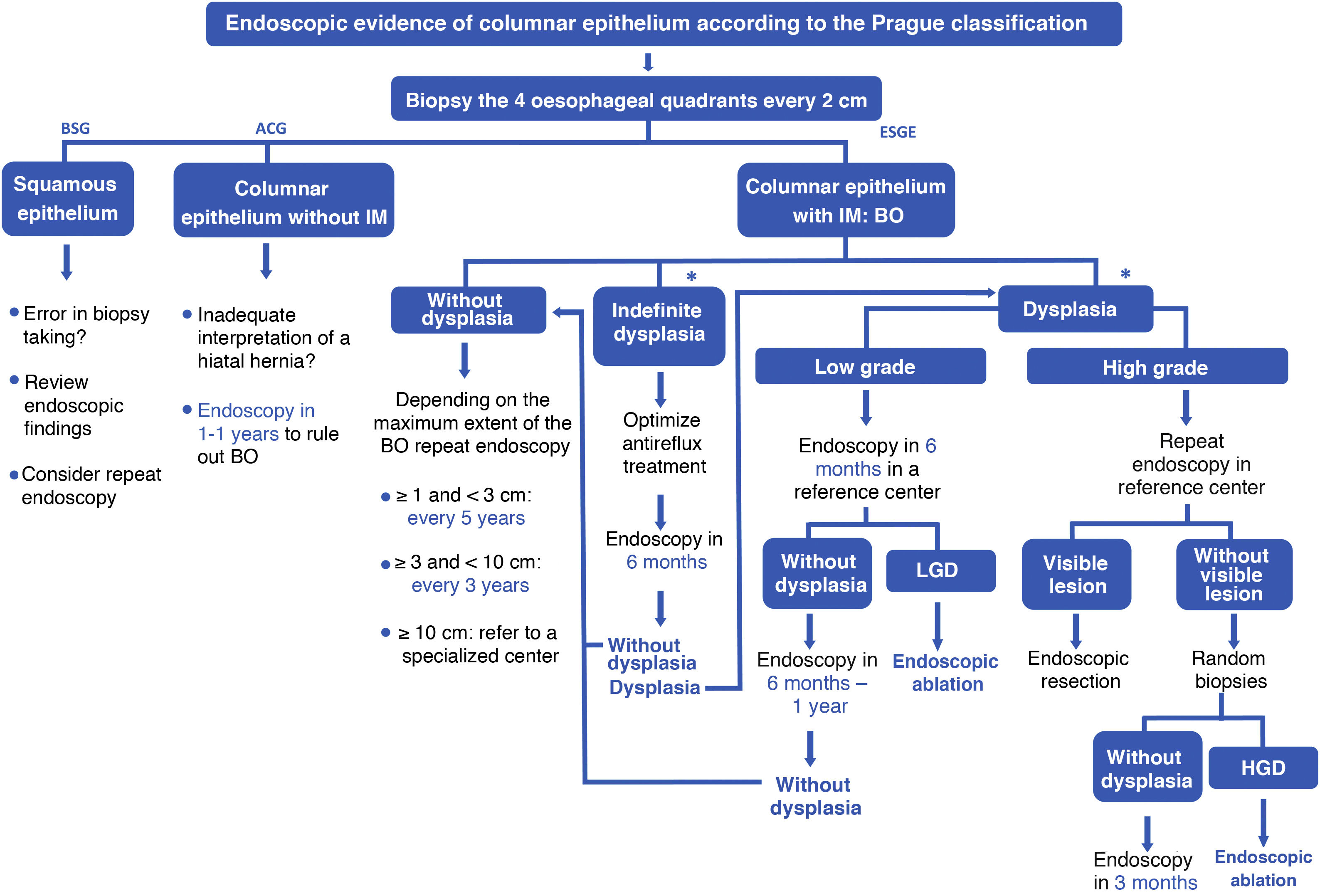
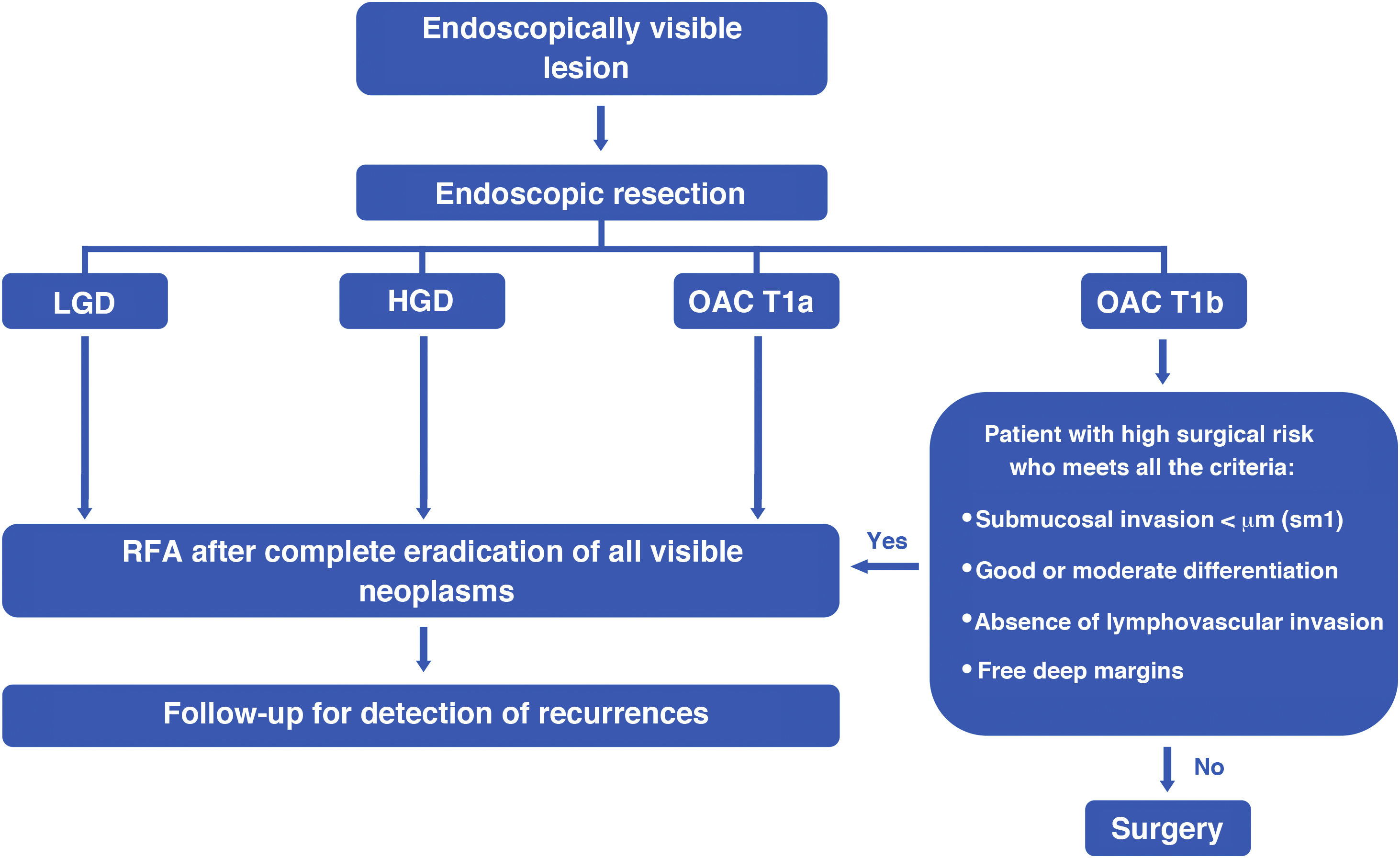
The main clinical relevance of Barrett’s esophagus (BE), a result of chronic exposure to gastroesophageal reflux, is its potential progression to esophageal adenocarcinoma (EAC). Although screening for BE is not recommended in the general population, after diagnosis of BE, a surveillance strategy for early detection of dysplasia or neoplasia is needed. The gold standard for diagnosis and surveillance is high-definition oral endoscopy with random biopsies. In addition, any visible lesion should be completely resected, which will be considered curative in the presence of low grade dysplasia (LGD), high-grade dysplasia (HGD) or EAC confined to the mucosa (T1a), followed by eradication of residual BE by endoscopic ablation. In the absence of a visible lesion, radiofrequency ablation should be performed to eradicate BE with LGD, HGD or intramucosal EAC.
La principal relevancia clínica del esófago de Barrett (EB), resultado de la exposición crónica al reflujo gastroesofágico, es su potencial progresión a adenocarcinoma esofágico (ACE). Aunque no se recomienda el cribado de EB en la población general, tras su diagnóstico es beneficiosa una estrategia de seguimiento para la detección precoz de displasia o neoplasia. El patrón oro para el diagnóstico y seguimiento es la endoscopia oral de alta definición con toma de biopsias aleatorias. Además, toda lesión visible debe resecarse de forma completa preferentemente mediante resección endoscópica mucosa, que se considerará curativa en presencia de displasia de bajo grado (DBG), displasia de alto grado (DAG) o ACE confinado a la mucosa (T1a), tras lo cual se debe erradicar el EB residual mediante ablación endoscópica. En ausencia de lesión visible, la ablación por radiofrecuencia es el tratamiento de elección para erradicar el EB con DBG, DAG o ACE intramucoso.