Pulmonary thromboembolism (PTE) is a very common condition with high mortality. Although some scales include heart failure (HF) as a risk factor of PTE, none of them have assessed the contribution of the different kinds of HF, i.e. with reduced or preserved left ventricular ejection fraction (LVEF) to the in-hospital outcome of patients admitted with PTE.
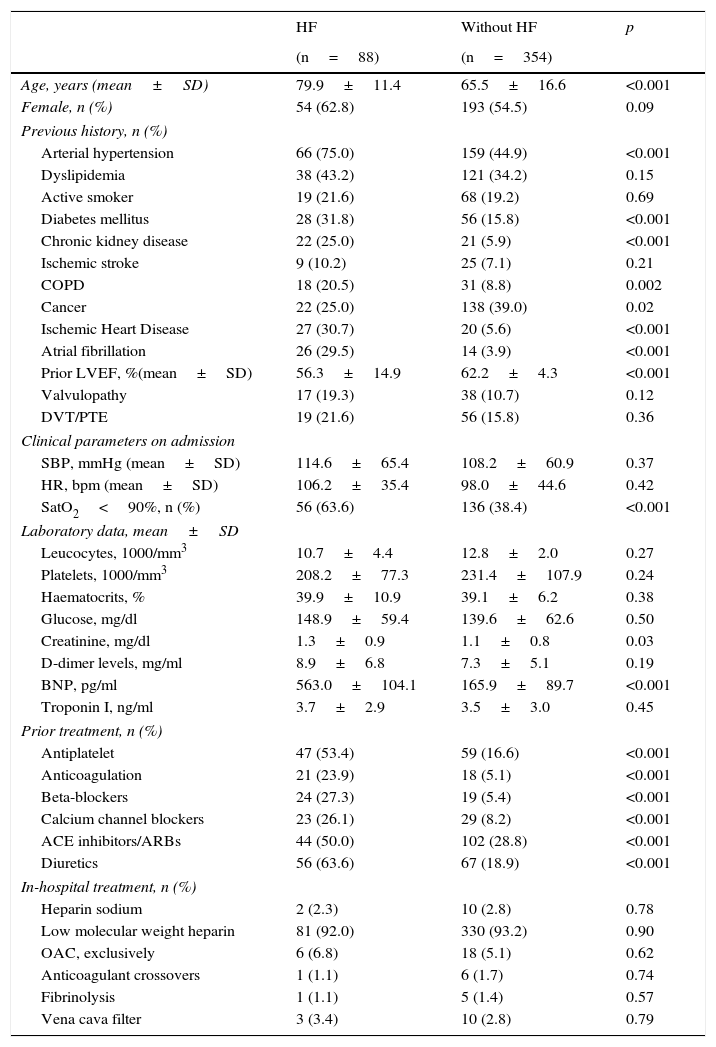
Patients and methodA retrospective study assessing a cohort of patients consecutively admitted to hospital with a PTE from 2012 to 2014. Baseline epidemiological characteristics, treatment during admission and prognostic variables during hospitalization were analyzed. Primary endpoint was defined as hospital mortality for any cause.
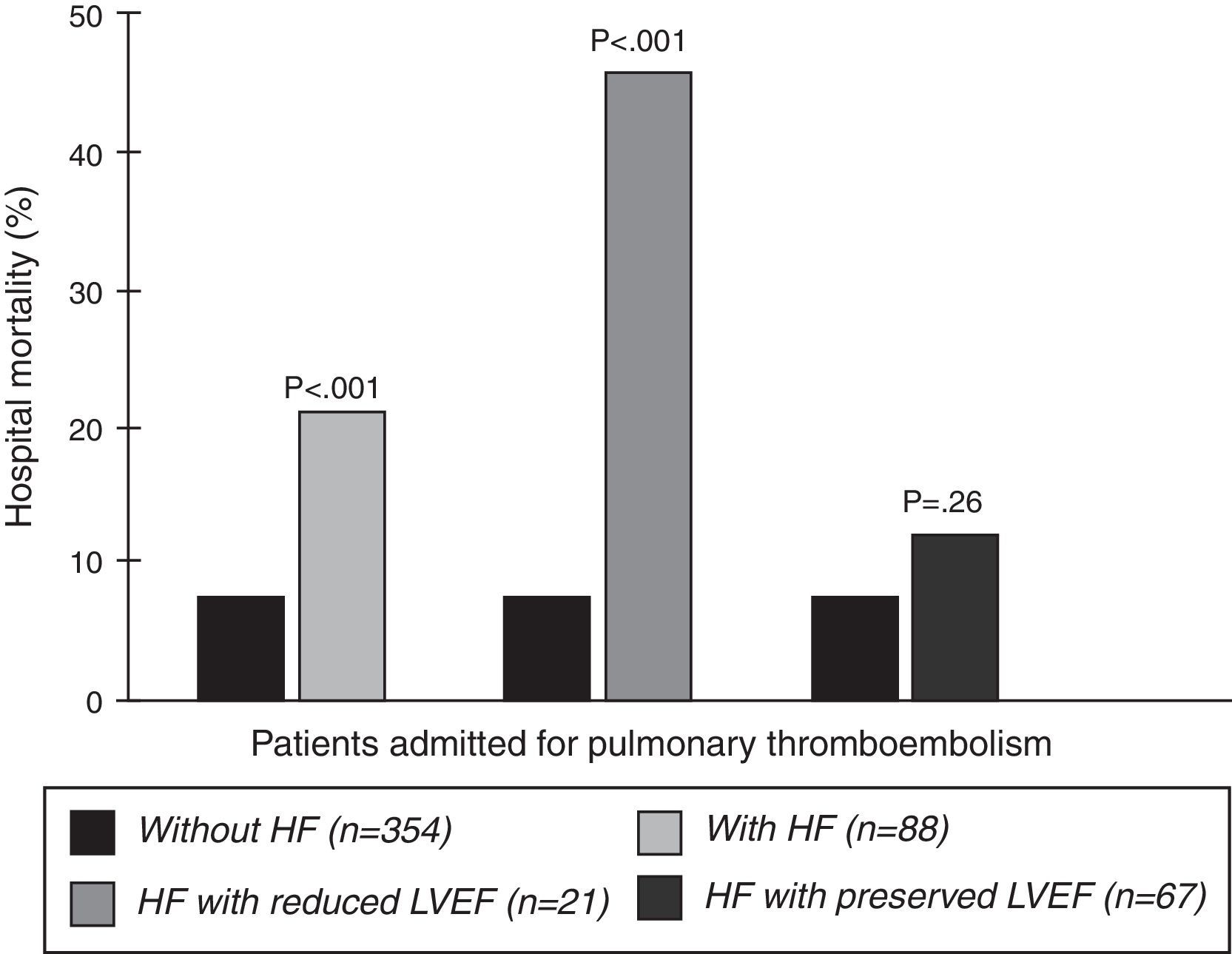
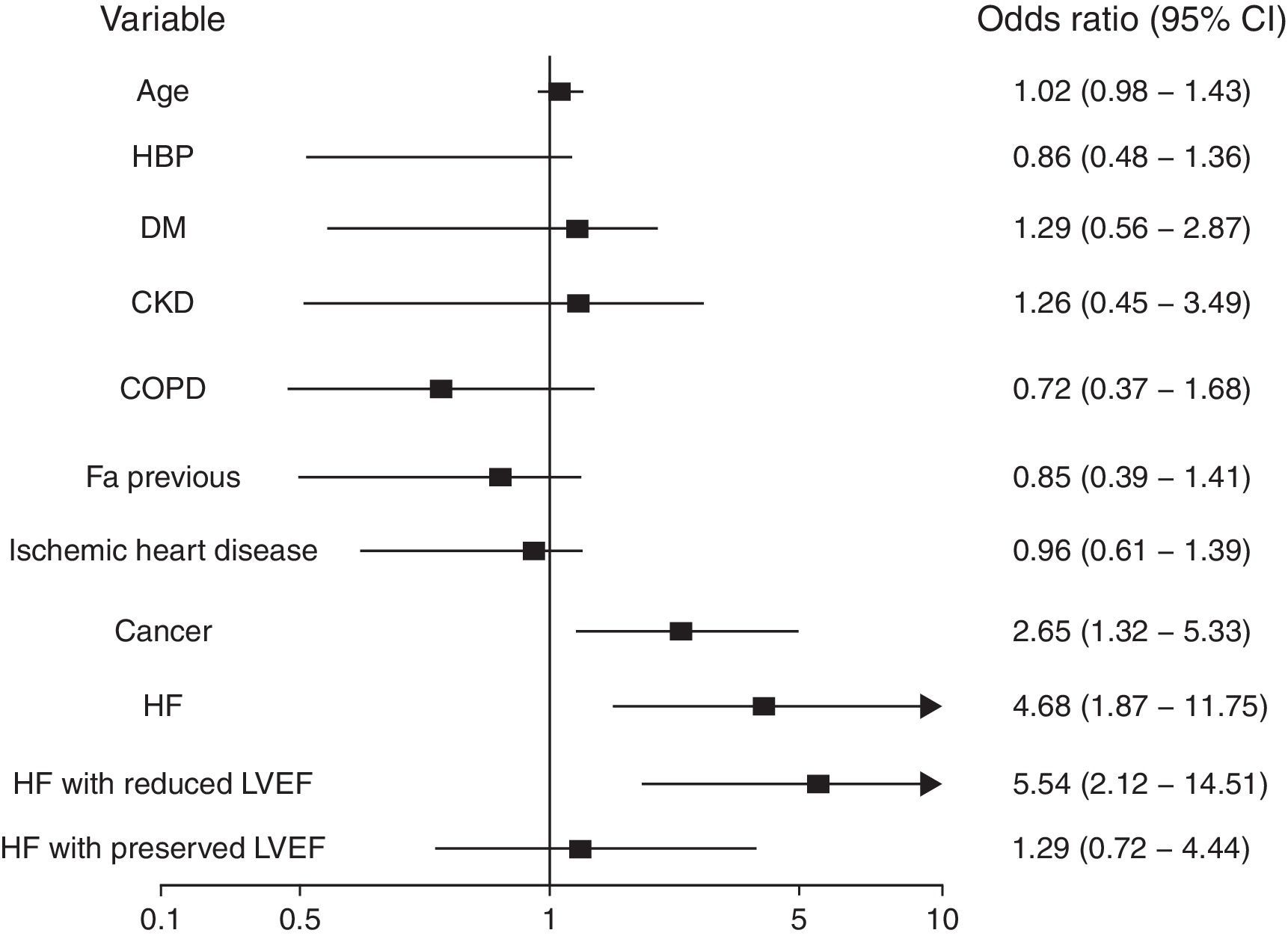
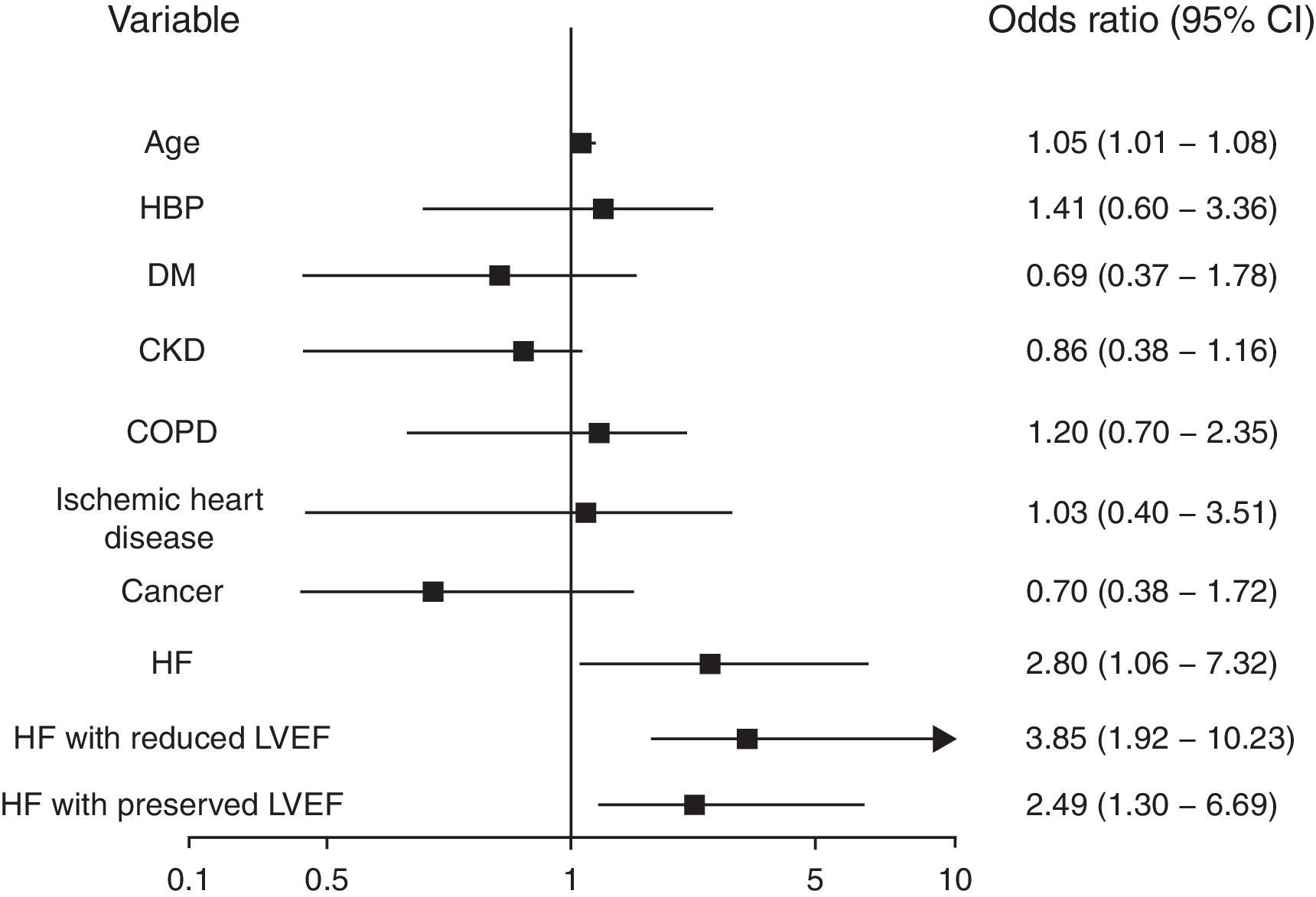
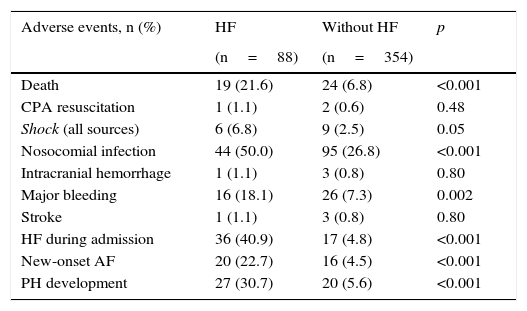
ResultsA total of 442 patients with PTE were included (88 with prior HF). Patients with a history of HF were older, more frequently had hypertension, diabetes mellitus, chronic kidney or pulmonary disease, cancer, and coronary artery disease, and showed less LVEF (p<.001). Hospital mortality was significantly higher in patients with prior HF (21.6 vs. 6.8%, p<.001). Multivariate analysis found that HF with reduced LVEF but not HF with preserved LVEF resulted as an independent risk factor (respectively OR 5.54; 95% CI 2.12–14.51 and OR 129; 95% CI 0.72–4.44).
ConclusionsPatients with prior HF admitted to hospital with PTE should be considered a high-risk population, since they present high in-hospital mortality. In our cohort, patients with prior HF and reduced LVEF presented a poorer prognosis than those with preserved LVEF.
El tromboembolismo pulmonar (TEP) es una entidad frecuente con una elevada morbimortalidad. Aunque algunas escalas consideran la insuficiencia cardiaca (IC) como factor de riesgo de TEP, ninguna ha analizado la contribución del tipo de IC, con fracción de eyección del ventrículo izquierdo (FEVI) reducida y preservada, al pronóstico intrahospitalario de los pacientes ingresados con un episodio de TEP.
Pacientes y métodoEstudio de cohortes retrospectivo que incluyó pacientes hospitalizados por TEP de manera consecutiva durante el período comprendido entre 2012-2014. Se analizaron las características epidemiológicas basales, el tratamiento durante su ingreso, así como variables pronósticas durante su estancia hospitalaria. Se definió como objetivo primario la mortalidad intrahospitalaria por cualquier causa.
ResultadosSe incluyeron 442 pacientes con TEP (88 con historia de IC). Los pacientes con antecedente de IC resultaron ser mayores, con mayor porcentaje de hipertensos y diabéticos, mayor presencia de enfermedad renal crónica, pulmonar u oncológica y cardiopatía isquémica, y con menor FEVI (p<0,001). La mortalidad intrahospitalaria fue significativamente mayor en el grupo con historia previa de IC (21,6 frente a 6,8%, p<0,001). En el análisis multivariante, únicamente la IC con FEVI reducida se mostró como factor de riesgo independiente (OR 5,54; IC 95% 2,12-14,51), no así la IC con FEVI preservada (OR 1,29; IC 95% 0,72-4,44).
ConclusionesLos pacientes con antecedentes de IC ingresados con un TEP deben ser considerados como una población de alto riesgo, presentando una elevada morbimortalidad intrahospitalaria. Dentro de este grupo, son aquellos con IC y FEVI reducida los que presentan un peor pronóstico.