After the introduction of antiretroviral therapy, a decrease in AIDS defining cancers (ADCs) is observed, while non-AIDS-defining cancers (NADCs) have increased in HIV-infected patients (HIP). We have little information about the prognosis and associated risk factors. We studied survival and its relationship with immunodeficiency after the diagnosis of ADC or NADC.
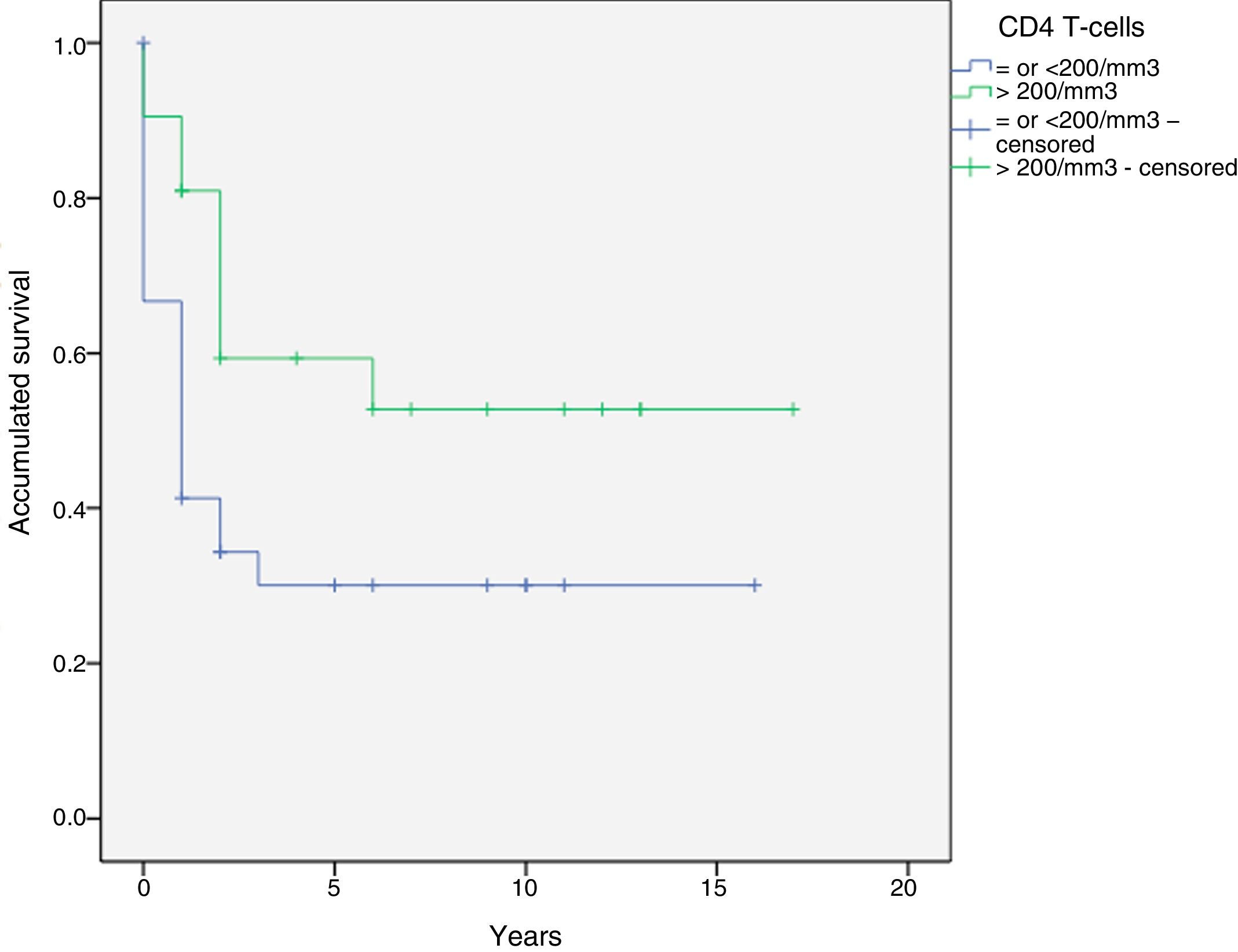
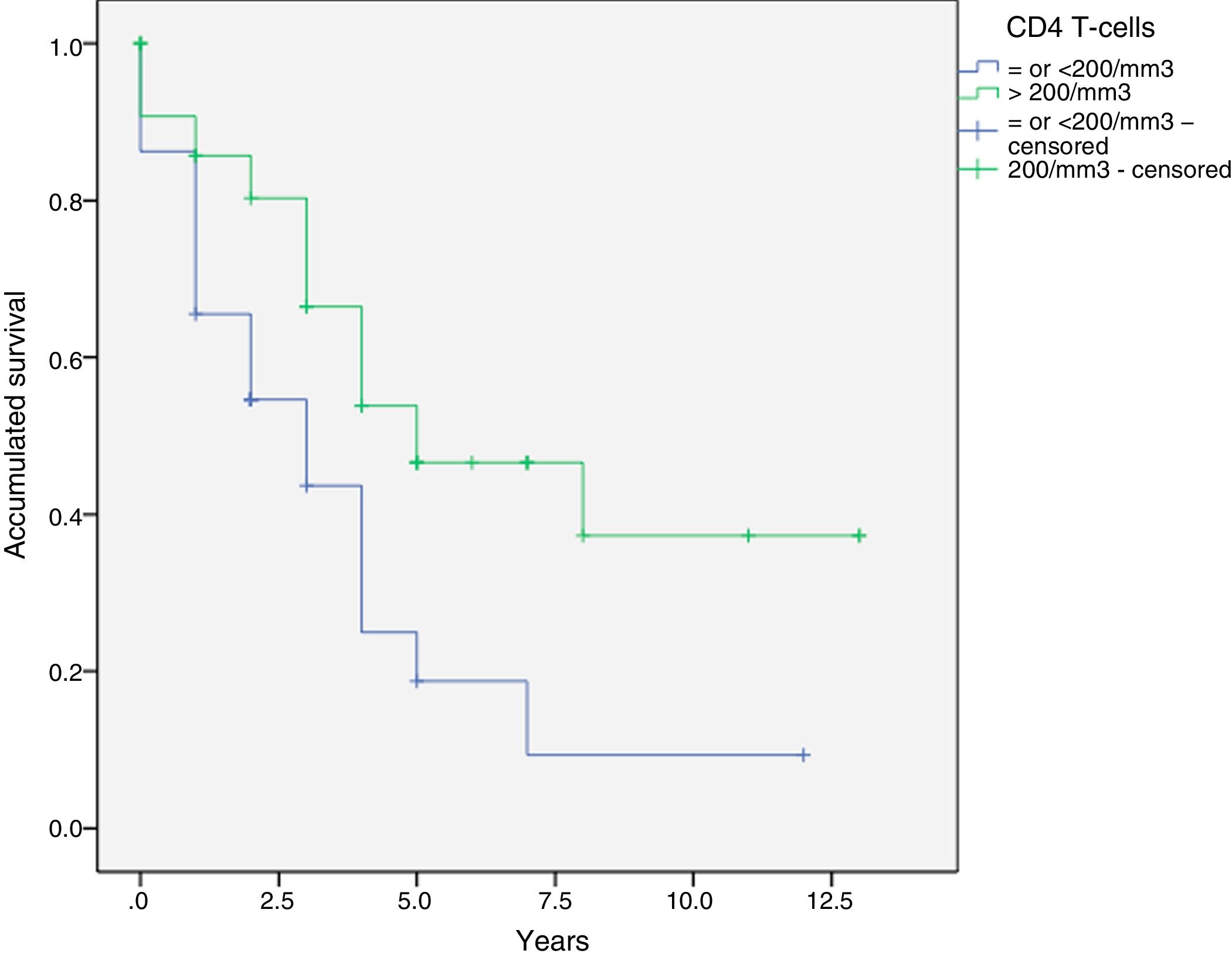
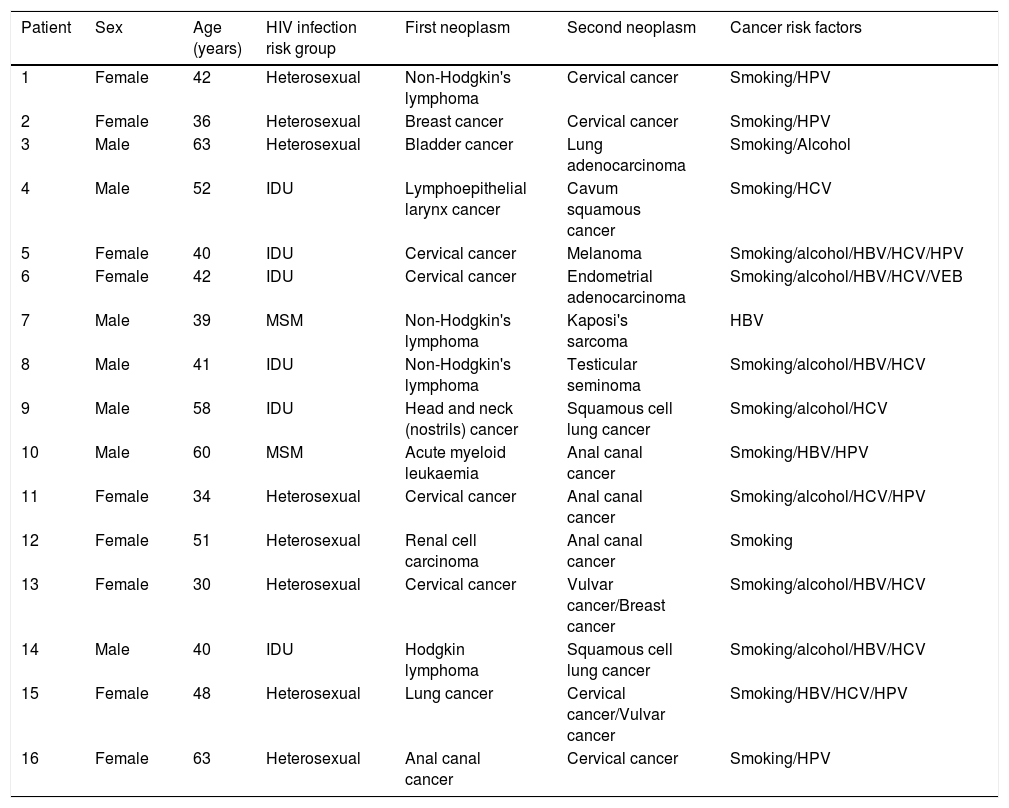
MethodsObservational, retrospective study of 788 HIP of whom 133 developed a malignancy between 2000–2016. Malignancies were divided into ADCs or NADCs and degree of immunodeficiency according to the CD4 T lymphocyte count > or <!--=200-->mm–3. Survival was estimated according to the Kaplan Meier method, multivariate COX regression analysis and compared with the log-rank test.
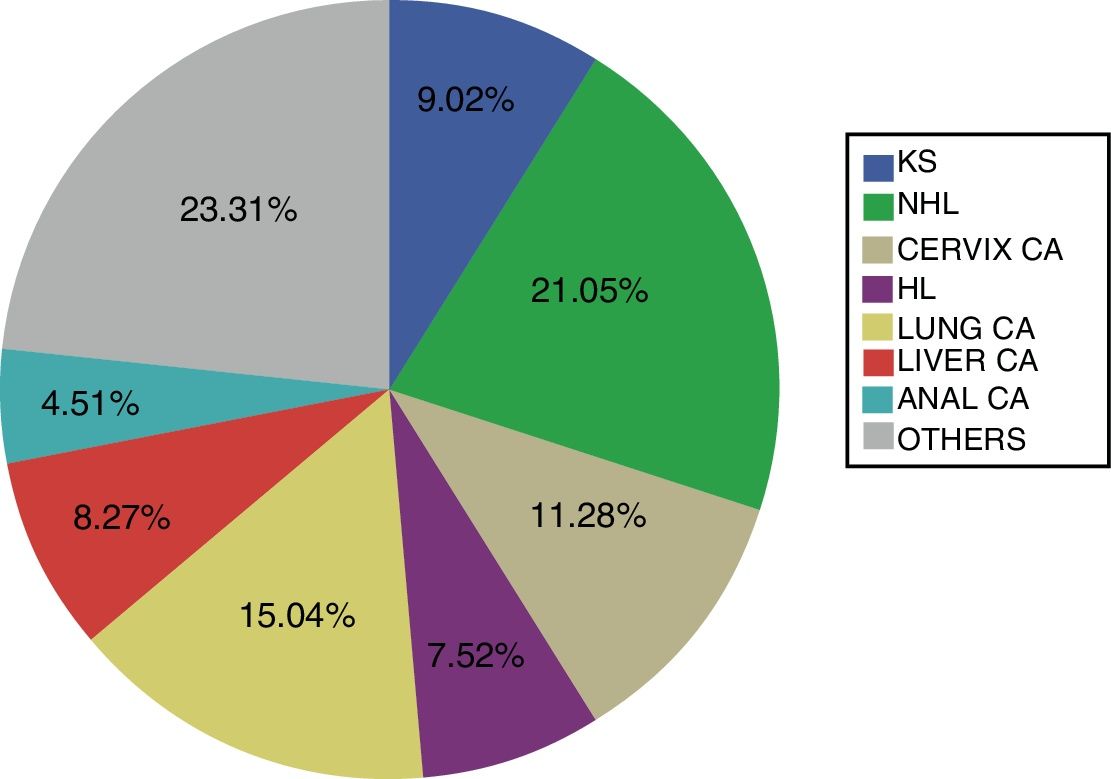
Results149 malignancies were diagnosed in 133 HIP: 41.4% ADCs and 58.6 NADCs. The most frequent tumour was NHL (21.1%), followed by lung carcinoma (15%). HCV was positive in 50.4% and 65.4% were smokers. Thirty-nine point one percent had a CD4 T lymphocyte count <!--=-->200/mm3, being 60% in the case of ADCs while in NADCs it was 38.5%. CD4 T lymphocyte count <!--=200-->mm–3 is significantly associated with lower survival after diagnosis of ADCs(p=0.031) and NADCs (p=0.005).
ConclusionsThe most frequent types of tumours in HIP differ from those in the general population, probably due to oncogenic risk factors. CD4 T lymphocyte count <!--=200-->mm–3 is a risk factor related to worse prognosis after NADC or ADC diagnosis.
Tras la introducción del tratamiento antirretroviral se objetiva una disminución de los tumores definitorios de sida (TDS), mientras que los tumores no definitorios de sida (TNDS) han aumentado en pacientes infectados por VIH (PIV). Disponemos de poca información sobre el pronóstico y factores de riesgo asociados. Hemos estudiado la supervivencia y su relación con la inmunodeficiencia tras el diagnóstico de TDS o TNDS.
Materiales y métodosEstudio observacional, retrospectivo, sobre 788 PIV de los que 133 desarrollaron una neoplasia maligna entre 2000-2016. Las neoplasias se dividieron en TDS o TNDS y el grado de inmunodeficiencia según el recuento de linfocitos T CD4 >o </=200/mm3. La supervivencia se calculó según el método de Kaplan-Meier, el análisis multivariante de regresión de COX y se comparó con el test de log-rank.
ResultadosSe diagnosticaron 149 neoplasias en 133 PIV: 41,4% TDS y 58,6 TNDS. El linfoma no Hodgkin (21,1%) fue el más frecuente, seguido por el carcinoma de pulmón (15%). Se objetivó prueba del VHC positiva en el 50,4% y eran fumadores el 65,4%. El 39,1% presentaban recuento de linfocitos T CD4 </=200/mm3, siendo el 60% en el caso de los TDS mientras que en TNDS eran un 38,5%. La cifra de linfocitos T CD4 </=200/mm3 está significativamente asociada a una menor supervivencia tras el diagnóstico de TDS(p=0,031) y TNDS(p=0,005).
ConclusionesLos tipos de tumores más frecuentes en los PIV difieren de los de la población general, probablemente por factores de riesgo oncogénico. El recuento de linfocitos T CD4 </=200/mm3 es un factor de riesgo relacionado con peor pronóstico tras el diagnóstico de TDS y TNDS.