Multiple sclerosis (MS) is a chronic and progressive condition in which physical, cognitive, and emotional abilities fluctuate over time. Early-stage patients may require educational resources and emotional support, while advanced-stage patients may benefit from symptom-tracking tools or caregiver support. Patients with MS can benefit significantly from mobile health (mHealth) applications to manage their condition (Heesen et al., 2023). These mHealth applications offer features such as symptom tracking, medication reminders, and mood monitoring, enabling patients to take a more active role in their care (Apolinário-Hagen et al., 2018). However, the adoption, sustainability, and integration of these tools within broader digital health ecosystems remain unclear. This study addresses the existing gaps by conducting a systematic evaluation of MS-specific mobile apps, focusing on their features, uptake, and value generation across stakeholder groups.
According to Jiang et al. (2018), mobile phone-based interventions have demonstrated their potential to improve medication adherence, which is critical for managing MS, while adherence supported by innovative interventions remains a cornerstone of managing MS, reduce relapses and improve quality of life (Onamade, 2018). Telemedicine has shown promising results in enhancing patient satisfaction and facilitating self-management among MS patients. While telemedicine has not significantly reduced relapse rates, it has supported medication adherence and overall well-being (Ahmed et al., 2023). However, despite the growing potential, research on how such tools are adopted and sustained in real-world practice or how they generate value within the broader health ecosystem remains limited. This study seeks to address this gap through a systematic analysis of MS-specific mobile apps, exploring their features, adoption patterns, and implications for stakeholders.
A cross-sectional observational study conducted by Mokhberdezfuli et al. (2021) confirmed that patients with MS who used a mobile app to track symptoms reported improved quality of life, with reduced fatigue, compared to those who did not use such tools. Additionally, apps facilitate effective communication between patients and healthcare professionals, enabling more personalized and timely interventions (Donevant et al., 2018). Amatya et al. (2019) reported that mHealth interventions improve medication adherence, reduce relapse rates, and enhance overall well-being in patients with MS. The ease of access and multifunctionality of such apps make them valuable tools for supporting self-management and improving outcomes in patients with MS.
According to the World Health Organization (WHO) (Organization et al., 2021), self-care health interventions can be categorized into several domains: individual agency (e.g., promoting self-care awareness), health information seeking (e.g., education for informed decision-making), social and community support (e.g., peer mentorship and counseling), personal health tracking (e.g., maintaining home-based records of health and diagnostic data), self-diagnosis (e.g., self-testing for health conditions), self-management (e.g., self-medication or treatment), and individuals’ integration with health systems. Given these categories, eHealth stands to benefit significantly from a comprehensive set of criteria to describe and evaluate smartphone applications effectively.
Despite the potential capabilities of mobile applications for MS, research on the usability and utility of such applications or on evaluations demonstrating their efficacy in improving health outcomes for patients with MS or their clinical effectiveness remains limited (Giunti et al., 2018b; Heesen et al., 2023; Marziniak et al., 2018; Salimzadeh et al., 2019). Furthermore, their use within the healthcare system requires complex validation processes (Zayas-García & Cano-de-la Cuerda, 2018).
IQVIA statistics, reported by the Medical Device Network in 2021, revealed >350,000 digital health applications available. However, application quality varies, and the report recommends careful consumer selection. Most downloads come from 110 dominant apps, accounting for almost 50 %, while 83 % of the apps contribute fewer than 1 %. Additionally, digital health bloomed in 2020, but app growth has slowed since 2017, rising only 10.3 %. This decline is attributed to the removal of poorly performing or outdated apps owing to high update costs and inactivity–51 % had fewer than 100 downloads, and 61 % were never updated. Disease-specific apps, such as those for MS, are gaining popularity, although the extent to which mHealth apps are utilized by MS patients remains underexplored (Marrie et al., 2019). A 2018 review (Marziniak et al., 2018) highlighted the growth of eHealth technologies for MS, including tools for screening, monitoring, treatment, and education. However, another review of 30 unique mHealth apps (Giunti et al., 2018a) revealed that they failed to meet the requirements of patients suffering from MS.
Therefore, this study aims to address these gaps by conducting a systematic review of mobile applications specifically designed for MS to evaluate their characteristics and quality. To guide this analysis, the study adopts the conceptual framework developed by Ribault et al. (2024), which explores six dimensions of app evaluation: context, stakeholder participation, features and requirements, development processes, implementation, and evaluation. This framework facilitates a holistic understanding of how digital tools operate within health ecosystems and supports an examination of longevity, update frequency, user popularity, and ratings. Accordingly, this study adopts an ecosystem perspective that considers the interdependent roles of patients, healthcare professionals, developers, and pharmaceutical actors in shaping value creation processes around mobile MS applications.
Methodologically, this study applies a qualitative, multi-method approach aligned with the framework proposed by Ribault. The research design integrates three complementary components: (1) a market review of 31 MS-related applications available in Spain, (2) semi-structured interviews with key ecosystem stakeholders—including clinicians, developers, and institutional representatives—and (3) a patient survey assessing adoption levels and perceived usefulness. This triangulated strategy enables a contextualized exploration of both supply-side development and demand-side engagement.
The research questions explored in this study include:
1. RQ1 How does the ecosystem of mobile applications for MS create value for stakeholders, including patients, caregivers, healthcare professionals, and developers?
2. RQ2 What is the level of digital adoption among patients with MS, and how does it influence the market for MS-related mobile health apps?
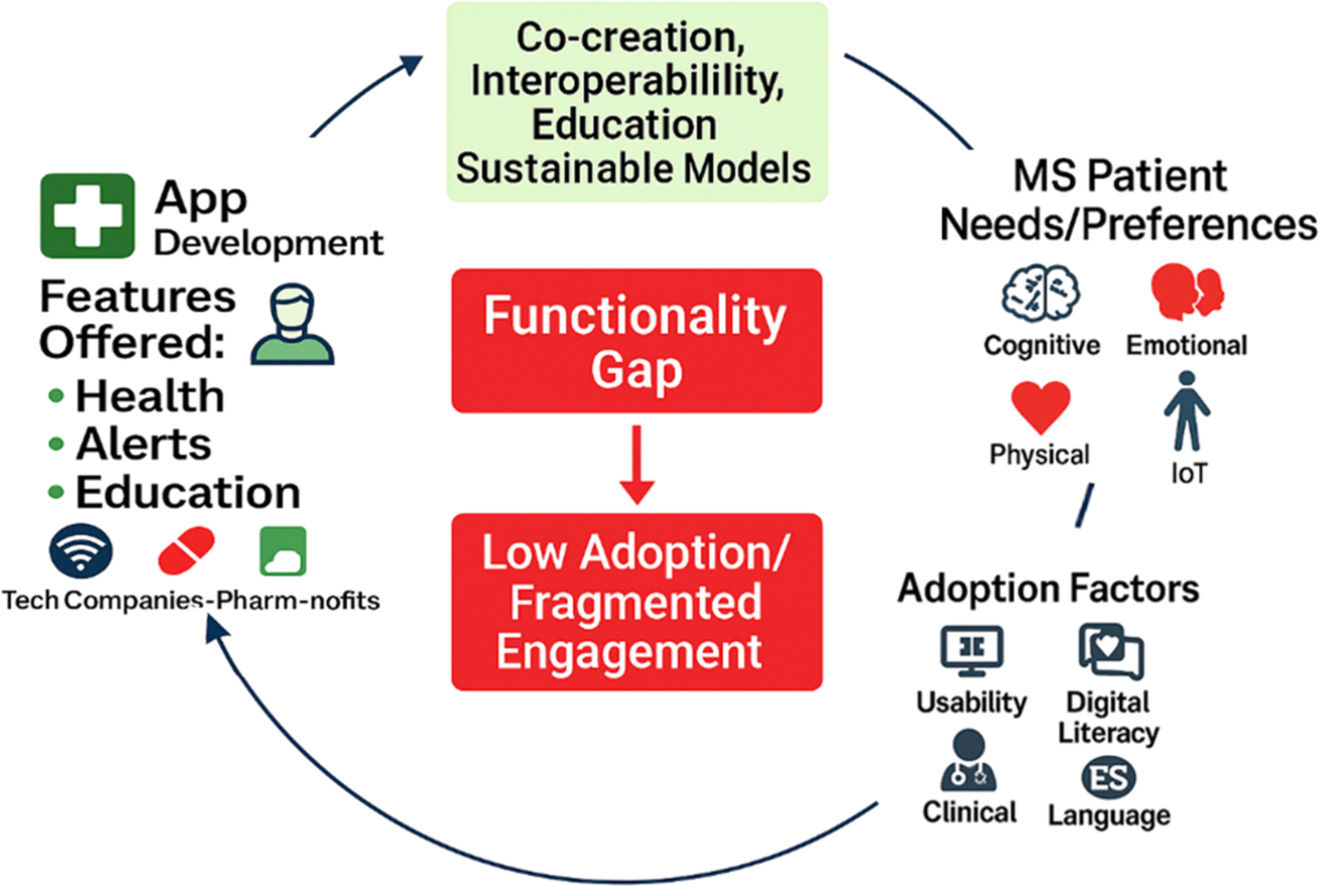
The findings reveal significant heterogeneity in the availability, functionality, and adoption of MS-related applications in Spain. Most tools remain underutilized despite being free and accessible, partly due to language limitations, lack of differentiation, and misalignment with clinical practices. The stakeholder interviews highlight structural barriers to implementation—particularly hospital-level data governance—while patient responses underscore usability gaps, low perceived added value, and limited integration into care routines. Collectively, the results emphasize the requirement for more coordinated, value-driven development strategies that consider the ecosystemic interaction between technological, institutional, and experiential factors.
The remainder of this paper is organized as follows: Section 2 introduces the conceptual framework. Section 3 describes the multi-method research design. Section 4 presents the empirical findings from the application review, stakeholder interviews, and patient survey. Section 5 discusses the results in relation to the research hypotheses and outlines the managerial implications. Finally, Section 6 concludes this study with a summary of contributions, limitations, and directions for future research.
Literature reviewBusiness models in digital platform ecosystemsThe application of platform ecosystem models in healthcare represents an emerging trend, driven by the rapid advancement of digital technologies and the proliferation of data (Chibuike et al., 2024). Inspired by natural ecosystems, the concept of a business ecosystem highlights the interactions and relationships among various stakeholders, including enterprises, agents, suppliers, competitors, governments, and other participants (Dhungana et al., 2013). Within the healthcare sector, such ecosystems offer the potential to facilitate innovative solutions and significant improvements by strengthening coordination and enabling more effective use of data across partners (Chen et al., 2024). Similar to biological ecosystems, platform business ecosystems are inherently complex and interdependent, requiring a delicate balance between competition and cooperation for effective functioning (Chen et al., 2024). Numerous scholars have underscored the need for further research on digital business models and the influence of digitalization on value creation, recommending an ecosystem perspective in such analyses (Burström et al., 2021; Kohtamäki et al., 2019; Plekhanov et al., 2023).
Traditional firm-centric business models are increasingly inadequate for addressing the complexities and interdependencies of modern innovation ecosystems (Iivari et al., 2016). This limitation is particularly pronounced as digital technologies continue to reshape competitive dynamics across industries, including healthcare (Spadaro et al., 2021). A critical determinant of success in healthcare ecosystems lies in the viability and sustainability of their business models, which should align with the interconnected and dynamic nature of such platforms (Broekhuizen et al., 2021). Cross-organizational platforms designed to enable the exchange of patient data exemplify this challenge, as they are required to overcome technical barriers and inherent difficulties of achieving long-term sustainability and effectiveness. Moreover, several such initiatives have failed to deliver the expected benefits, although digital transformation has become a priority for managers and features prominently on leadership agendas (Warner & Wäger, 2019). This digital paradox arises because technological superiority does not solely guarantee success (Stoumpos et al., 2023; Vial, 2021). Further research into ecosystem business models is essential to understand how companies can collaboratively create, capture, and sustain value in the digital age (Burström et al., 2024; Madanaguli et al., 2023; Palmié et al., 2022). This highlights the need to investigate how mobile app ecosystems for MS create value for diverse stakeholders, as patients, healthcare professionals, and developers, as integral participants.
While artificial intelligence (AI)-driven business models create competitive advantages, the mechanisms behind these advantages remain largely unexplored and warrant further empirical investigation (Jorzik et al., 2024). The advancement of digital technologies has unlocked new possibilities for establishing open exchange relationships with stakeholders, positioning the ecosystem of companies as a driving force for AI-driven business model innovation by enabling value co-creation with customers and fostering collaboration among stakeholders (Warner & Wäger, 2019). In the case of MS-based mobile apps, competitive advantage has shifted from individual apps and their developers to the broader business ecosystem, which includes patients, caregivers, healthcare professionals, and developers as integral participants, along with medical device manufacturers, public health organizations, insurers and payers, pharmaceutical companies, and academic institutions and researchers. Understanding how this ecosystem generates value across such a wide range of participants is essential for addressing RQ1.
Successful digital transformation depends not only on technological advancements but also on strong managerial capabilities and the ability to design, develop, and implement digital business model innovation (Vial, 2021). Practitioners of ecosystem innovation emphasize the importance of redefining business models by identifying and capitalizing on novel value points that can be created, controlled, and monetized within a network of interconnected stakeholders (Trischler & Li-Ying, 2023). In the healthcare sector, particularly within the context of eHealth, redefining business models underscores the critical need to combine cutting-edge technologies with robust managerial strategies to ensure the success and scalability of platform-based ecosystems (Spadaro et al., 2021). This relevance is particularly pronounced for mobile health apps targeting MS patients, where the level of digital adoption significantly influences market dynamics and shapes the scalability of such platforms.
Parallel to the growing academic interest in platform-based ecosystems within healthcare (Burström et al., 2021; Spadaro et al., 2021), recent studies have emphasized the need to move beyond purely technological approaches toward models that prioritize value co-creation, collaboration, and sustainability over the long term. Nevertheless, despite these conceptual advances, empirical evidence remains limited regarding how such ecosystem-based business models operate in disease-specific contexts such as MS, particularly from the perspective of patients, healthcare professionals, and developers as active participants. This gap reinforces the relevance of adopting an ecosystem perspective to elucidate value creation processes in digital health environments.
To synthesize the most relevant contributions and highlight the themes relevant to this study, Table 1 presents a summary of key literature on ecosystem-based business models in eHealth platforms. The selected research illustrates current perspectives on stakeholder roles, value distribution, and the structural and managerial challenges that remain unresolved in the context of digital health ecosystems.
Ecosystem-Based Business Models in eHealth Platforms.
| Author(s) / Year | Ecosystem Focus | Key Contribution | Gaps / Challenges Identified |
|---|---|---|---|
| Chibuike et al. (2024) | Platform ecosystems in healthcare | Analyzes interdependencies and value flows among healthcare actors | Limited disease-specific implementation guidance |
| Chen et al. (2024) | Shared infrastructures for health data | Emphasizes cross-actor coordination and data governance in healthcare ecosystems | Requires robust and sustainable governance models |
| Plekhanov et al. (2023) | Digital transformation in healthcare | Advocates for ecosystem-oriented business model innovation | Needs empirical application to chronic care and app ecosystems |
| Burström et al. (2021, 2024) | Digital service ecosystems in health | Explores value creation and stakeholder engagement in digital health | Calls for greater integration of patient experience and voice |
| Spadaro et al. (2021) | Platform scalability and management in eHealth | Highlights importance of managerial capabilities beyond technology | Lacks empirical validation of digital adoption factors |
| Broekhuizen et al. (2021) | Data-sharing platforms in healthcare | Discusses viability and sustainability of cross-organizational platforms | Emphasizes frequent underperformance in digital health outcomes |
| Trischler and Li-Ying (2023) | Co-innovation and value appropriation in health ecosystems | Focuses on co-creation and user-centered value capture in eHealth | Understudied in chronic disease contexts like MS |
Accordingly, (Section MS self-management applications: characteristics and adoption) focuses on mobile health applications for MS, examining how their functionalities and adoption patterns relate to the broader principles of ecosystem value creation and patient-centered innovation.
MS self-management applications: characteristics and adoptionThe growing prevalence of smartphones and tablets has established mobile applications as a powerful tool for empowering and engaging high-demand, high-cost patients in managing their own health (Damanabi et al., 2022; Salimzadeh et al., 2019). mHealth applications incorporate numerous functionalities, such as recording, storing, and sharing patient information with healthcare providers; self-monitoring health status; managing lifestyles; and providing access to the latest research, news, and practical tips on health, nutrition, and fitness. Such apps improve treatment adherence, raise awareness, help monitor daily activities, manage medications, symptoms, and mood, among other functions (Marziniak et al., 2018; Salimzadeh et al., 2019). However, despite these advances, no existing mobile application for patients with MS offers a holistic and integrative solution that unifies all the diverse features into a single platform (Ruzic & Sanford, 2018).
A recent evaluation of self-care interventions via eHealth apps revealed significant shortcomings in the quality and reliability of available tools (Mueller et al., 2019). Among 100 reviewed apps, only 20 % utilized evidence-based information, with healthcare professionals deeming approximately 32 % useful; 52 % were considered misleading, and 11 % potentially harmful. These findings underscore a critical gap in the advancement and evaluation of digital health tools, where the absence of standardized frameworks undermines the confidence of both patients and healthcare professionals (Ribaut et al., 2024). This gap limits the adoption of effective solutions and complicates efforts to ensure their safe integration into health management ecosystems.
From the perspective of service providers, the adoption of such technologies can lead to a more efficient use of clinic resources, enable continuous monitoring of interventions, track adverse events, and optimize therapy in ways that traditional face-to-face approaches cannot achieve (Marziniak et al., 2018; Özden et al., 2024. However, despite the growing number of apps designed to support MS symptom monitoring and disease tracking, few have undergone rigorous evaluation in published studies. Although the field of eHealth continues to expand rapidly, no consensus exists on how to define and evaluate the quality of such apps, further complicating their adoption and integration into clinical practices (Ribaut et al., 2024; Stach et al., 2020).
Considering the importance of the aforementioned capabilities in the management of MS, mobile apps designed for self-management can serve as personalized tools to better support patients (Gee et al., 2015; Heesen et al., 2023). Such applications provide a multidimensional platform that:
- •
empowers patients to manage their condition, enhances adherence to therapeutic and disease management strategies, and facilitates the collection of individualized data on MS progression (Damanabi et al., 2022; Marziniak et al., 2018; Salimzadeh et al., 2019); and
- •
provides healthcare professionals with valuable evidence to better support patients in optimizing self-management (Alexander et al., 2021; Apolinário-Hagen et al., 2018).
Despite these potential benefits, research on the usability and utility of MS-specific mobile apps remains limited, with only a few reports addressing patient perspectives (Heesen et al., 2023; Klimova, 2018; Zayas-García & Cano-de-la Cuerda, 2018) and specialist perspectives (Greiner et al., 2015).
Recent studies on mobile applications for MS have identified several limitations, including inadequate functionality (Giunti et al., 2018a, Giunti et al., 2017), a mismatch between supply and demand (Giunti et al., 2018a), unmet self-management requirements (Ruzic & Sanford, 2018), a lack of collaboration between patients and healthcare providers in development (Gromisch et al., 2021), and a gap between MS self-management requirements and available applications (Cohen, 2018; Vacchi et al., 2024). A 2018 review highlighted this problem by revealing that only 8 out of 681 smartphone apps designed to support medication adherence (1.2 %) had documented evidence of effectiveness (Ahmed et al., 2018). This evidence is a critical consideration for healthcare systems when certifying and reimbursing such technologies. Mobile applications offer opportunities for easy access and scalability, but the limited evaluation evidence presents a critical barrier. Thus, both patients and healthcare professionals face difficulties in identifying and recommending high-quality applications (Nebeker et al., 2020).
Table 2 summarizes recent studies evaluating mobile applications for MS, emphasizing methodological characteristics. A majority of existing studies focus on single-stakeholder perspectives—mainly patients—and employ either usability assessments or exploratory thematic analysis. Few studies adopt triangulated methods or use structured conceptual frameworks for app evaluation. This gap underscores the need for a more comprehensive methodology, as adopted in this study.
Summary of Methodological Approaches and Ecosystem Gaps in Prior MS App Evaluation Studies.
| Author(s) / Year | Focus / Study Aim | Methodology | Findings & Limitations: | Implications & Gaps |
|---|---|---|---|---|
| Greiner et al. (2015) | To evaluate patient and physician views on MSdialog, a digital PRO diary for MS management. | Mixed-methods study: online survey and 6-week pilot with patients and HCPs; combined quantitative and qualitative feedback | MSdialog improved usability, communication, and data sharing, with high patient satisfaction and HCP support. However, findings are limited by short duration, small, incentivized sample, and restricted feature access. | Limited long-term data and lack of clinician experience reduce generalizability. Future research should involve diverse populations, integrate apps into clinical workflows, and assess effects on outcomes and adherence. |
| Giunti et al. (2018) | To assess how features in MS mobile apps meet the reported needs of persons with MS. | Scoping review assessing 581 apps from Google Play and iTunes; 30 MS-specific apps were analyzed. | Most apps focused on disease management, education, and data visualization. Limitations include lack of quality assessment, restriction to English/Spanish apps from US/Spain stores, and absence of stakeholder engagement or clinical perspective. | Highlights lack of patient-centered design and limited professional involvement. Recommends co-design, improved content validation, and expanded features |
| Marziniak et al. (2018) | To review digital and remote communication tools for MS management, focusing on clinical uses, benefits, and limitations. | Narrative review of 28 eHealth tools for MS, categorized by function, using literature and expert input. | eHealth tools enhance access, self-management, and monitoring, with promising apps like MSdialog. Accepted by patients and professionals, but evidence is limited to early-phase studies, with unclear long-term impact and cost-effectiveness. | Limited phase 3 trials and screening tools, with barriers like cost, literacy, and data overload. Future research should develop integrated, equitable, user-centered platforms and conduct large-scale controlled trials. |
| Salimzadeh et al. (2019) | To identify and characterize mobile apps for multiple sclerosis (MS), with a focus on self-management features. | Systematic search of app stores (Nov 2017); 1042 apps screened; 27 MS self-management apps analyzed. | About 26 % of MS apps support self-management with symptom tracking, medication reminders, and report sharing. App quality varies. Study limits: English-only apps, description-based review | Highlights the lack of comprehensive self-management apps. Recommends development of evidence-based, user-centered tools with broader language support and usability evaluation and calls for long-term integration strategies. |
| Alexander et al. (2021) | To identify validated wearable technologies for MS outcome monitoring and assess their suitability for clinical trial use. | Scoping review (PRISMA-ScR) identifying 35 unique wearable solutions via database and citation searches | Most wearables tracked gait/activity, with limited attention to cognition or fatigue. Apps varied in quality. Many lacked validations, were commercially restricted, and showed usability or compatibility issues, limiting generalizability. | There’s no consensus on optimal wearables. Many lack validation and overlook outcomes like fatigue or mood. Future research should develop multi-domain tools and standardize evaluation and validation criteria. |
| Gromisch et al. (2021) | To review the frequency, uses, and barriers of mHealth use among persons with MS. | Systematic review (2010–2019) of 59 studies analyzing mHealth use, barriers, and design considerations | mHealth supports symptom tracking and interventions, but barriers include cognitive and physical impairments. Emphasizes user-centered design. Limitations include English-only scope, lack of meta-analysis, and no assessment of app quality or cost. | Many apps lack usability and efficacy data, with minimal involvement of MS patients in development. Future research should address digital literacy, accessibility, and promote user-centered design with patient participation. |
| Damanabi et al. (2022) | To explore the self-management needs of people with MS to inform the development of a mobile application. | Qualitative study with 12 MS patients; semi-structured interviews analyzed using content analysis and MAXQDA | Identified seven self-management domains with emphasis on personalized, culturally relevant, and emotionally supportive content. Findings are limited by small, gender-skewed samples and exclusive focus on patient perspectives. | The study excludes caregiver and clinician perspectives, limiting generalizability. Future research should involve multiple stakeholders, include diverse populations, and support participatory design and testing of MS apps. |
Although some narrative reviews, such as those by Cohen (2018) and Marziniak et al. (2018), discuss the relevance of healthcare professionals and systemic integration in the adoption of MS-related digital tools, they do so only from a conceptual perspective. Such studies refer to stakeholders, including clinicians or system developers, as contextual actors or future targets of integration strategies. However, they do not collect empirical data directly from such agents. Consequently, the current literature remains predominantly focused on patients, with limited consideration of the broader ecosystem in which these applications are designed, implemented, and evaluated. This lack of empirical, multi-actor approaches creates a methodological and conceptual gap in understanding how value is co-created across stakeholder groups, particularly within clinical practice.
Unlike the existing research (summarized in Table 2), this study incorporates a structured conceptual framework (Ribaut et al., 2024), validated evaluation criteria (e.g., MARS), and triangulation across stakeholders, thereby addressing methodological fragmentation and enhancing ecological validity. By explicitly including the perspectives of patients, clinicians, and technology developers, this study adopts both an ecosystemic and multi-method strategy that responds to current demands for more inclusive, sustainable, and context-aware digital health innovation.
Theoretical background and applicationsBuilding upon the conceptualization of MS health applications as part of broader digital platform ecosystems (Section Business models in digital platform ecosystems) and the empirical gaps identified in current solutions (Section 2.2), this section articulates the theoretical background that supports the formulation of the study’s hypotheses. Instead of treating apps as isolated digital tools, they are analyzed as embedded service platforms within a health innovation ecosystem, where value emerges through ongoing interactions among patients, clinicians, developers, and other stakeholders (Spadaro et al., 2021; Vial, 2021). This approach emphasizes the co-constructed nature of value, which is not generated by the app in isolation but through coordinated exchanges across actors in the digital health ecosystem, aligning with requirements for more inclusive and participatory models of value co-creation in eHealth (Burström et al., 2024; Heesen et al., 2023).
Although digital health ecosystems have evolved at breakneck speed, the available evidence suggests that MS mobile apps do not provide sustained value to all stakeholders they aim to engage (including patients, caregivers, clinicians, and developers). Numerous studies have identified a common set of functionalities offered by these applications, including symptom reporting, medication reminders, and health data tracking (Damanabi et al., 2022; Giunti et al., 2018b).
Limited real-world application is caused by the isolated state of these functionalities and the lack of meaningful coherence integrated into clinical practice or patient routines (Gromisch et al., 2021; Heesen et al., 2023). Evidence suggests that the most crucial functionalities for patients, such as tools for self-management, physical therapy, personal monitoring, and emotional support, are unevenly covered or executed in ways that fail to account for user diversity and the evolving requirements of self-management (Marziniak et al., 2018; Ribaut et al., 2024).
This misalignment between app functionalities and stakeholder expectations reflects deeper structural forces in the app economy, where value creation remains narrowly conceived in terms of clinical adherence rather than more inclusive patient activation. Consequently, the first hypothesis is formulated to address the first research question (RQ1) by assessing whether available apps effectively translate stakeholder demands into value-added services across the ecosystem.
H1: The value perceived by patients in MS mobile applications depends on features supporting self-management, cognitive engagement, and the extent to which these features align with coordinated value propositions across the digital health ecosystem (including clinicians, caregivers, and developers).
Additionally, value creation cannot be attained without user adoption, the primary driver of ecosystem sustainability. While patient uptake is a critical component, adoption at scale also requires coordinated engagement from other ecosystem actors, including healthcare providers, caregivers, and system integrators Although recent studies have reported high interest of patients with MS in the adoption of digital health technologies, particularly those offering advanced features such as IoT integration or cognitive monitoring (Alexander et al., 2021; Cohen, 2018), actual adoption rates remain low. Various challenges have been described in the literature, including poor usability, insufficient language support, and suboptimal integration with healthcare professionals (Marrie et al., 2019; Zayas-García & Cano-de-la Cuerda, 2018). Furthermore, heterogeneity in evidence suggests a digital divide, in which patients express willingness to use digital apps, but this intention is not matched by digital literacy or technical accessibility, specifically among certain population groups (Mueller et al., 2019). Additionally, adoption barriers may be amplified when apps fail to embed seamlessly into clinical workflows, patient–caregiver dynamics, or institutional infrastructures, thereby limiting the emergence of sustained, shared value within the broader ecosystem. This leads to the second hypothesis, addressed in RQ2: how adoption rates influence the value and market dynamics of MS health applications.
H2: Low adoption rates among Spanish patients with MS persist despite high interest, due to usability and literacy gaps, and are further shaped by systemic misalignments between app functionalities and broader ecosystem integration (e.g., lack of clinical interoperability or care coordination).
Collectively, the two hypotheses guide the dual analysis of the MS app ecosystem: first by examining how effectively current solutions meet stakeholder value propositions, and second, by exploring the real-world adoption patterns that ultimately determine their success or obsolescence.
To accurately evaluate these hypotheses, a robust conceptual framework is required—one that captures the design and functionality of mobile apps, along with their embeddedness in the broader ecosystem of healthcare service delivery. These demands go beyond traditional performance metrics, requiring frameworks that explicitly account for user involvement, value co-creation, and real-world deployment.
The existing literature on the evaluation of mobile health apps reflects a fragmented setting. Earlier frameworks have typically focused on usability, design heuristics, or independent performance metrics, without considering the intricacies of health ecosystems or the requirements of diverse stakeholders (Mueller et al., 2019). For example, certain models focus on evidence-based content or compliance facilitation (Ahmed et al., 2018), while others emphasize user experience or app store ratings (Giunti et al., 2018b). Such perspectives overlook structural components such as development processes, stakeholder participation, or real-world deployment, which are essential for understanding how value is created and sustained within complex healthcare environments (Spadaro et al., 2021). With increased calls for comprehensive, stakeholder-focused app evaluation (Burström et al., 2024; Heesen et al., 2023), academics have begun to argue for models that include dimensions such as co-creation, lifecycle upkeep, integration with clinical workflows, and trust-building.
Most existing evaluation approaches focus on isolated aspects such as usability, evidence-based content, or app ratings. However, these perspectives often overlook the ecosystemic nature of digital health platforms, including structural misalignments between developer priorities and stakeholder needs. Responding to recent demands for more comprehensive evaluation models (Burström et al., 2024; Heesen et al., 2023), this study adopts a framework capable of bridging these conceptual and methodological gaps.
To address existing limitations, this study applies the framework proposed by Ribault et al. (2024) to systematically evaluate MS-specific applications. Each of the six proposed dimensions—context, stakeholder participation, features and requirements, development processes, implementation, and evaluation—serves as a reference point for structuring the analysis and ensuring comparability across cases. The framework aligns with the objectives of this study, as it allows the systematic analysis of how MS mobile apps create value (RQ1) and how patterns of digital adoption can be better understood (RQ2).
Stakeholder participation and development activities provide a formalized viewpoint from which fragmentation and misalignment within current offerings can be assessed. Additionally, the framework enables triangulation of app characteristics with patient survey data, the main methodological component of this study, through flexible yet stringent categories that support both qualitative and quantitative integration. Accordingly, Ribaut et al.’s framework not only bridges conceptual gaps identified in previous literature but also offers methodological value and clarity in evaluating the current ecosystem of MS mobile apps. Thus, beyond its practical utility, the framework reinforces the ecosystem perspective and stakeholder-oriented logic that underpin the theoretical foundation of this study.
MethodsAccording to Section 1, a methodology is required to evaluate MS-related applications. The methodological approach used in this study draws on the structured framework introduced by Ribaut et al. (2024), which delineates six key evaluation dimensions for eHealth interventions. While the framework is relatively recent, it consolidates dimensions already applied independently in prior validated tools, offering a structured and scientifically grounded model suitable for replicable evaluation. To ensure rigor and comparability with validated tools, the proposed evaluation criteria are cross-referenced with the Mobile App Rating Scale (MARS) developed by Stoyanov et al. (2015), which is widely recognized for assessing the quality of mobile health applications in terms of engagement, functionality, aesthetics, and precision of information. Furthermore, the preferred reporting items for systematic reviews and meta-analysis (PRISMA-S) standards (Rethlefsen et al., 2021) are adopted to guide the systematic identification and screening of MS-related applications. MARS has been widely adopted in the literature to evaluate mHealth applications across chronic diseases, including diabetes, asthma, and mental health, establishing it as a scientifically validated methodology (Stoyanov et al., 2015). PRISMA-S has become a gold standard in systematic review reporting and has been used extensively in eHealth application reviews, ensuring the replicability and transparency of search strategies (Rethlefsen et al., 2021). Finally, ecosystem-based triangulation, including survey data from patients with MS in Spain (Tabuenca et al.), provides an empirical basis for assessing the relevance and applicability of the identified app characteristics, confirming both methodological reliability and contextual validity. Triangulation of data sources—including app store content, survey responses, and literature-derived criteria—is a widely accepted practice in mixed-methods health research, enhancing internal validity and contextual reliability.
The methodology adopted in this study is structured into three main stages, followed by two integrative actions: reflective diagnosis and principle distillation. These stages are summarized in Fig. 1 and described further.
Systematic Review of Mobile Applications (Step 1): This first step involves a comprehensive and structured review of mobile applications designed for individuals with MS. The step comprises three sub-steps:
- •
Identification of existing criteria for evaluating eHealth apps based on peer-reviewed literature and established evaluation tools such as MARS and the AGREE-II framework.
- •
Development of a conceptual framework rooted in the six dimensions proposed by Ribaut et al. (2024): context, stakeholder participation, requirements and features, development process, implementation, and evaluation.
- •
Construction of a detailed set of evaluation criteria that integrates theoretical insights with app-specific functionalities, enabling a consistent and replicable assessment of app characteristics.
Ecosystem-Based Triangulation (Step 2): The second methodological step integrates a multi-perspective analysis of the eHealth app ecosystem, combining both quantitative and qualitative sources. First, patient perspectives are captured through a national survey conducted in Spain, using instruments informed by validated frameworks (uMARS, MAUQ, PAM-13), as detailed by Tabuenca et al. (submitted). The survey design is developed in collaboration with healthcare providers and patient associations. The survey instrument used in this study has been developed and deployed as part of a larger research initiative led by Tabuenca et al., with all the methodological details, such as question formulation, recruitment procedures, and ethical approvals, included in their original publication. Although the questionnaire is not a direct replication of any validated instrument, its structure and item content are aligned with established survey tools commonly applied in mHealth and chronic disease self-management research. Specifically, the survey design draws conceptual parallels with the User version of MARS (uMARS) developed by Stoyanov et al. (2015), which evaluates subjective app quality and user experience; the Patient Activation Measure (PAM-13), widely adopted in self-care and engagement research; and the mHealth App Usability Questionnaire (MAUQ) introduced by Zhou et al. (2019), which focuses on usability metrics in chronic health contexts. These alignments enhance content validity and support the relevance of the constructs for analyzing digital health adoption and app use among patients with MS. Additionally, case-based analyses are conducted with key ecosystem stakeholders, including neurologists, digital health technology providers, and representatives from pharmaceutical companies. These case studies follow an exploratory qualitative methodology, involving document review, semi-structured interviews, and scenario-based discussions. The interview guide is informed by the Open Innovation Project Canvas for SMEs (Steen & Vanhaverbeke, 2018), which provides a structured foundation for formulating role-sensitive questions on value propositions, stakeholder dynamics, revenue models, and strategic positioning. The case method is selected owing to the lack of large, structured samples in these stakeholder groups, and is intended to capture contextual, organizational, and strategic insights on app deployment and value perception.
Analytical Matching and Taxonomy Building (Step 3): In this step, data from the systematic app review are cross-referenced with patient feedback to identify alignment and gaps between app features and user expectations. Subsequently, a hierarchical taxonomy of application types and associated value propositions is constructed, enabling the classification of apps based on their functional scope—such as assessment, education, treatment scaffolding, and gamification—and their degree of alignment with core stakeholder needs.
Reflective Diagnosis: This integrative step synthesizes insights from patient data and stakeholder case studies, facilitating the identification of alignment or gaps between app offerings and stakeholder expectations across the ecosystem. These include mismatches in feature design, evidence-based content, interoperability, and engagement models.
Principle Distillation: Finally, the findings are translated into guiding principles yp inform future design and evaluation practices for MS-related digital health tools. These principles emphasize stakeholder-centric design, real-world applicability, interoperability, and long-term sustainability.
Selection of appsTo perform a comprehensive and clear review of the MS applications available in the main mobile phone stores, it is essential to follow the PRISMA-S guidelines. PRISMA-S provides a methodological framework for the identification, selection, and examination of relevant references that ensure both rigor and reproducibility (Rethlefsen et al., 2021).
Once the scope of the research is defined—including the types of MS applications relevant for analysis, such as self-management, symptom tracking, and communication support—the search strategy and inclusion/exclusion criteria are further developed. A comprehensive search in the Google Play Store and Apple App Store has been conducted using relevant keywords such as "multiple sclerosis", "MS self-management", "MS symptoms," and related terms. Since triangulation with information from Spanish-speaking patients with MS is adopted, the search strategy includes apps available in Spanish or English but accessible from Spain. This approach ensures transparency and allows replication of the search process by other researchers (Page et al., 2021).
The selection of mobile apps follows a systematic search strategy aligned with PRISMA-S guidelines. Searches are conducted in both the Apple App Store and Google Play Store using the keyword “multiple sclerosis” in English and Spanish. Apps are included if they meet the following criteria: (1) targeted individuals with MS or their caregivers; (2) provide disease-related information, symptom tracking, treatment support, or community features; (3) are available for free or under a freemium model; and (4) are accessible for download in Spain. Exclusion criteria include apps not specifically designed for MS (e.g., general neurology apps), non-functional or outdated apps, and duplicates across platforms. The final sample is cross-checked independently by two researchers to ensure consistency.
To expand the dataset, an additional search is performed using a large language model (LLM). A similar query is submitted to the LLM to increase the number of detected applications and obtain supplementary classification details. An independent researcher conducts a validation search to ensure the completeness and precision of the compiled list. This external check ensures the reliability and comprehensiveness of the dataset derived from the initial platform searches and the LLM results.
This multistep methodology integrates platform-based searches, advanced LLM-assisted exploration, and independent verification, ensuring a robust and comprehensive approach to cross-platform application classification.
Once the comprehensive list of applications is compiled, a refinement or screening process is conducted to align with the research objectives. Applications designed specifically for disseminating information at events or exhibitions are excluded, as they do not align with the objectives of the study.
Similarly, apps designed exclusively for physicians are excluded from the dataset, along with those targeting conditions broader than MS. Applications unavailable in Spain are excluded, ensuring that the research remains focused on tools providing functionalities to support patient self-management and directly align with the core objectives of understanding applications that empower patients to manage their health independently.
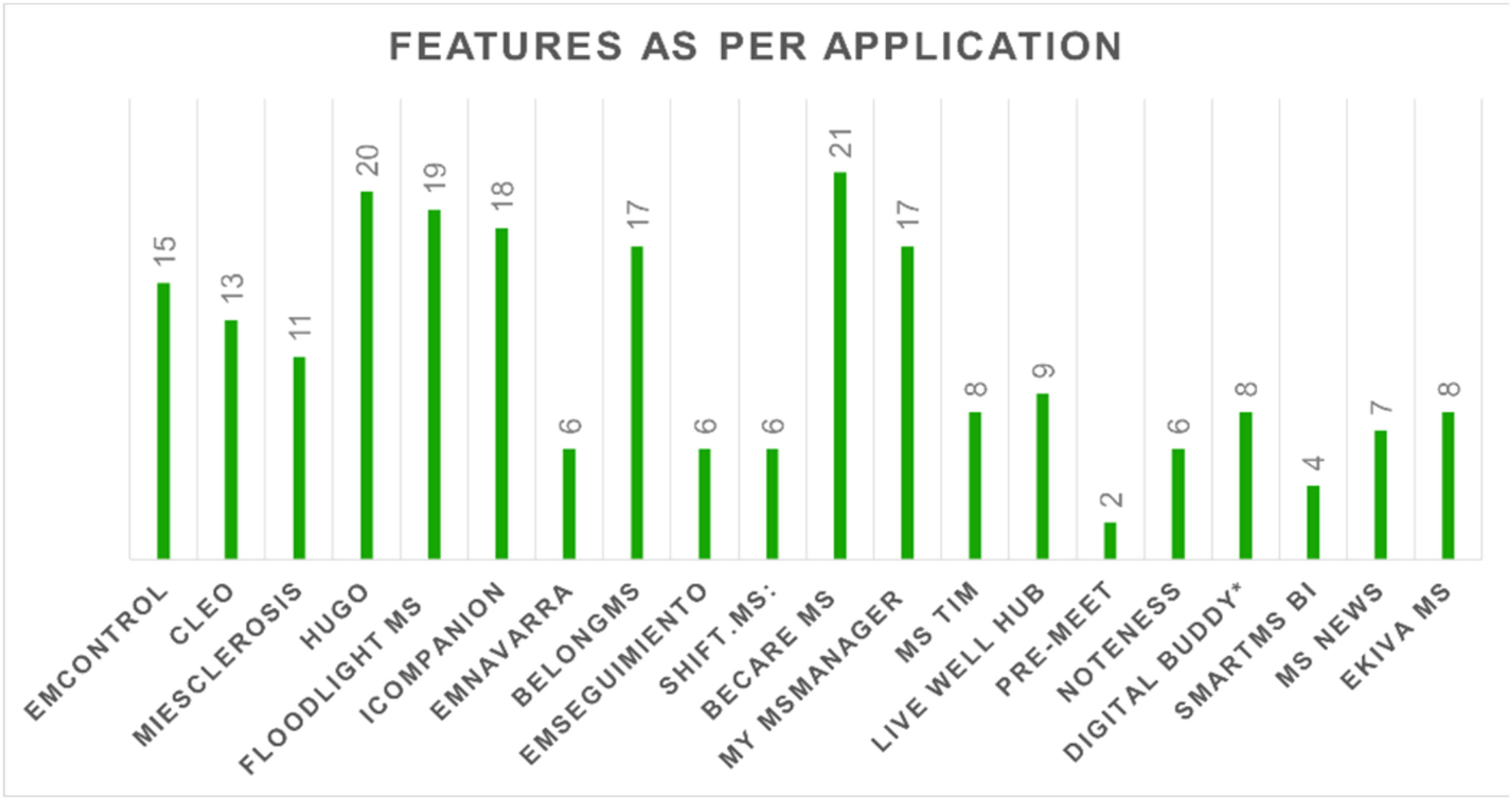
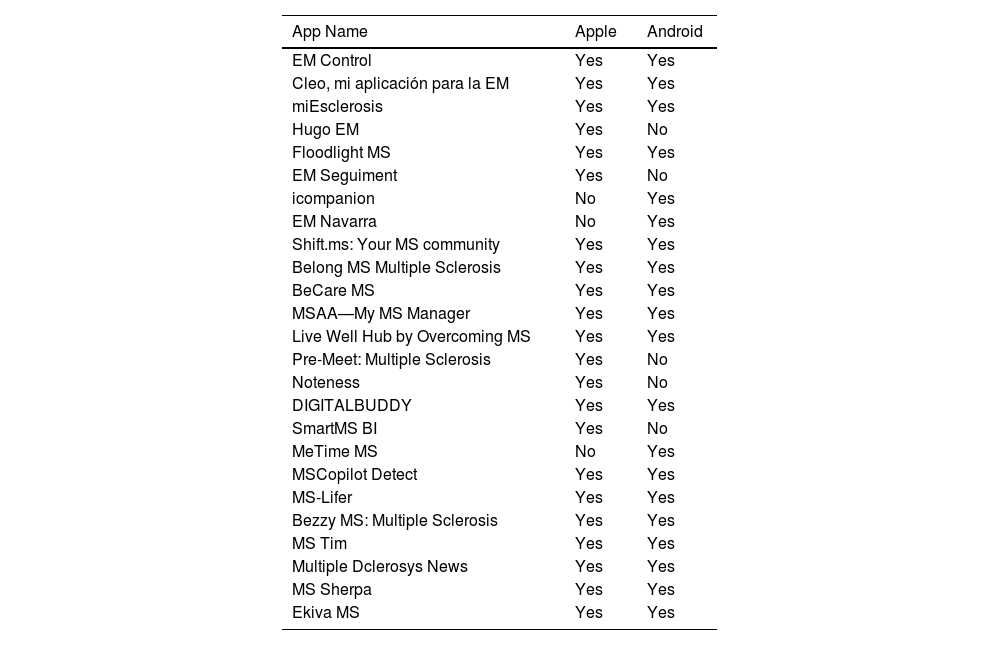
The process is visually summarized in Fig. 2. Of the 31 applications initially identified, 25 meet the eligibility criteria and are included for feature-based assessment. These criteria require apps to identify patients with MS, provide relevant support functionalities, and be accessible in Spain. Five apps requiring exclusive access codes are excluded. For the retained application, several features are individually collected, including self-management functions, data collection capabilities, app store classification category, availability in the Apple App Store, user scores for iOS and Android, support languages, developer, URL, and functional descriptions. The final list of applications analyzed is presented in Table 3.
Finalized List of Selected Apps.
Regarding platform availability, 75 % of apps are accessible on Android and 90 % on iOS, consistent with the patient device distribution reported in the survey (Section Ecosystem-Based Triangulation). Language availability was also assessed: while most apps are available in English, only 45 % include Spanish, potentially limiting accessibility for Spanish-speaking users. App store ratings average 4.5/5, although these are often based on a small number of reviews, limiting interpretability. Download counts (available only for Android) vary widely, with Cleo and Belong MS exceeding 100,000 downloads, while several others have fewer than 1000.
App features are identified and extracted from each store description and in-app functionalities using a standardized coding sheet developed during the systematic review. These features are inductively grouped into thematic categories reflecting value propositions, such as self-assessment, medication tracking, exercise guidance, educational support, and community interaction. The classification process is guided by previous literature on digital health value delivery models and validated frameworks, including MARS by Ribaut et al. (2024). A two-stage coding and refinement process is conducted by the research team to ensure consistency in category assignment. Disagreements are resolved through discussion, and overlapping features are mapped to multiple categories where relevant.
Ecosystem-Based triangulationThe second methodological block integrates a multi-perspective analysis of the eHealth app ecosystem, combining both quantitative and qualitative sources. This approach ensures a robust understanding of the digital health landscape for MS by drawing on patient experiences and the strategic perspectives of key stakeholders. A framework ensuring replicability and traceability for app assessment is currently being registered in PROSPERO (International Prospective Register of Systematic Reviews). All authors independently assess the applications, extracting relevant parameters. The Appraisal of Guidelines for Research and Evaluation-II (AGREE-II) instrument (Consortium et al., 2013), widely used in guideline development processes, is considered. While most included studies have not been designed to develop appraisal guidelines, the AGREE-II tool comprises 23 items across six domains: scope and purpose (3 items), stakeholder involvement (3 items), rigor of development (8 items), clarity of presentation (3 items), applicability (4 items), and editorial independence (2 items, addressing reporting of funding sources and competing interests). This instrument, along with the standardized feature set proposed by Salimzadeh et al. (2019), informs the adopted framework, ensures systematic categorization, and facilitates comparison of findings.
First, patient perspectives are captured through a national survey conducted in Spain, based on validated instruments (uMARS, MAUQ, PAM-13), as detailed by Tabuenca et al. cite_start. The survey instrument, developed and deployed as part of a larger research initiative by Tabuenca et al., conceptually aligns with established mHealth evaluation tools for chronic disease self-management, drawing conceptual parallels with uMARS by Stoyanov et al. (2015) for subjective app quality and user experience, PAM-13 for self-care and engagement, and the mHealth App Usability Questionnaire (MAUQ) by Zhou et al. (2019) for usability metrics in chronic health contexts. This alignment enhances the validity of the survey and confirms the relevance of its constructs to digital health adoption and app usage among patients with MS. The online structured questionnaire is specifically designed for patients with MS across Spain to understand their use of digital health technologies for condition management, focusing on mobile applications and wearable devices. This approach acknowledges the increasing popularity of mobile and wearable technologies in healthcare, offering insights into patient tool usage and perceived barriers to adoption. The survey is promoted through an active email campaign coordinated by Getafe University Hospital in Madrid and patient associations, including Asociación Española de Esclerosis Múltiple (AEDEM-COCEMFE), Fundación Esclerosis Múltiple Madrid (FEMM), and Esclerosis Múltiple España (EME), ensuring nationwide outreach. A three-month email campaign with periodic reminders maximizes response rates, with introductory emails clarifying research objectives to encourage participation. This recruitment strategy aims to secure substantial participation from the target population, with full design details available in a previous study (Tabuenca et al.). By triangulating reported behaviors and preferences, the patient perspective captured in this study offers richer insights for both practitioners and academics.
Notably, triangulation with observational sources is a relevant factor because the actions presented in the following subsection are conducted. The methodology has been illustrated in Fig. 3.
Conceptual view for Methodology. Adapted from Ribaut et al. (2024).
A total of 503 responses are collected from Spanish patients with MS through the online survey campaign. The sample includes 73.5 % women (n = 370) and 26.5 % men (n = 130), reflecting the known gender distribution of MS. Regarding technology, 69.3 % report using Android smartphones, 26.1 % use iOS devices, and 4.6 % own basic phones. The mean age of diagnosis is recorded as 35.9 years. App usage frequency varies considerably: mean weekly usage is 55.5 min (SD = 74.0), indicating high variance between low and high engagement users. Reported motivations for using digital tools include improved mobility, enhanced self-management, psychological support, and better communication with peers and professionals.
To complement the analysis of user-facing applications and incorporate multi-actor perspectives within the digital ecosystem of MS-related mHealth applications, a series of semi-structured interviews is conducted with key stakeholders involved in the development, prescription, and implementation of such tools. Stakeholders include developers, pharmaceutical representatives, hospital managers, and medical professionals (e.g., neurologists and general practitioners). Participants are selected through purposive sampling based on their relevance within the innovation and delivery ecosystem of MS applications.
Ethical approval for the study has been granted by the ethics committee of the university (project number: DYCDVEESSE-MG-DATOS-20,230,301), and informed consent was obtained from all participants prior to data collection.
Each interview is conducted for approximately 30 min via online conferencing platforms to ensure flexibility. The interviews follow an exploratory, semi-structured format, combining a common set of open-ended questions with tailored modules depending on the interviewee’s role, whether as a developer, institutional stakeholder, prescriber, or market intermediary. The interview guide is informed by the Open Innovation Project Canvas for SMEs (Steen & Vanhaverbeke, 2018), which provides a structured foundation for formulating role-sensitive questions in key domains such as value propositions, stakeholder dynamics, revenue models, and strategic positioning. This framework is particularly useful in capturing business model assumptions and perceived success factors from the perspective of non-user actors.
Simultaneously, the selection of interviewees is guided by Ribault et al. (2024), whose framework conceptualizes stakeholder salience within service ecosystems, as shown in Fig. 3. This perspective enables the identification of actors with critical functional or symbolic relevance across different stages of the app lifecycle, particularly those involved in development, adoption, and clinical recommendation, or business model definition and financial sustainability.
By integrating the perspectives of heterogeneous ecosystem participants, this study aims to mitigate single-perspective bias and reflect the real-world complexity and interdependencies in the MS app ecosystem. This multi-actor design aligns with the service-dominant logic by acknowledging that value is co-created not only at the point of application but also through distributed exchanges and resource integration across the healthcare and innovation landscape.
Analytical matching and taxonomy buildingIn this step, data from the systematic app review (Section Selection of Apps) are cross-referenced with patient-reported feedback and stakeholder insights (Section Ecosystem-Based Triangulation) to identify alignment issues or gaps between app features and user expectations. This process enables a deeper understanding of how the available functionalities meet the diverse and evolving requirements of patients with MS. A hierarchical taxonomy of application types and associated value propositions is developed. This taxonomy facilitates the classification of apps based on their functional scope, such as assessment, education, treatment scaffolding, and gamification, and their alignment with core stakeholder needs.
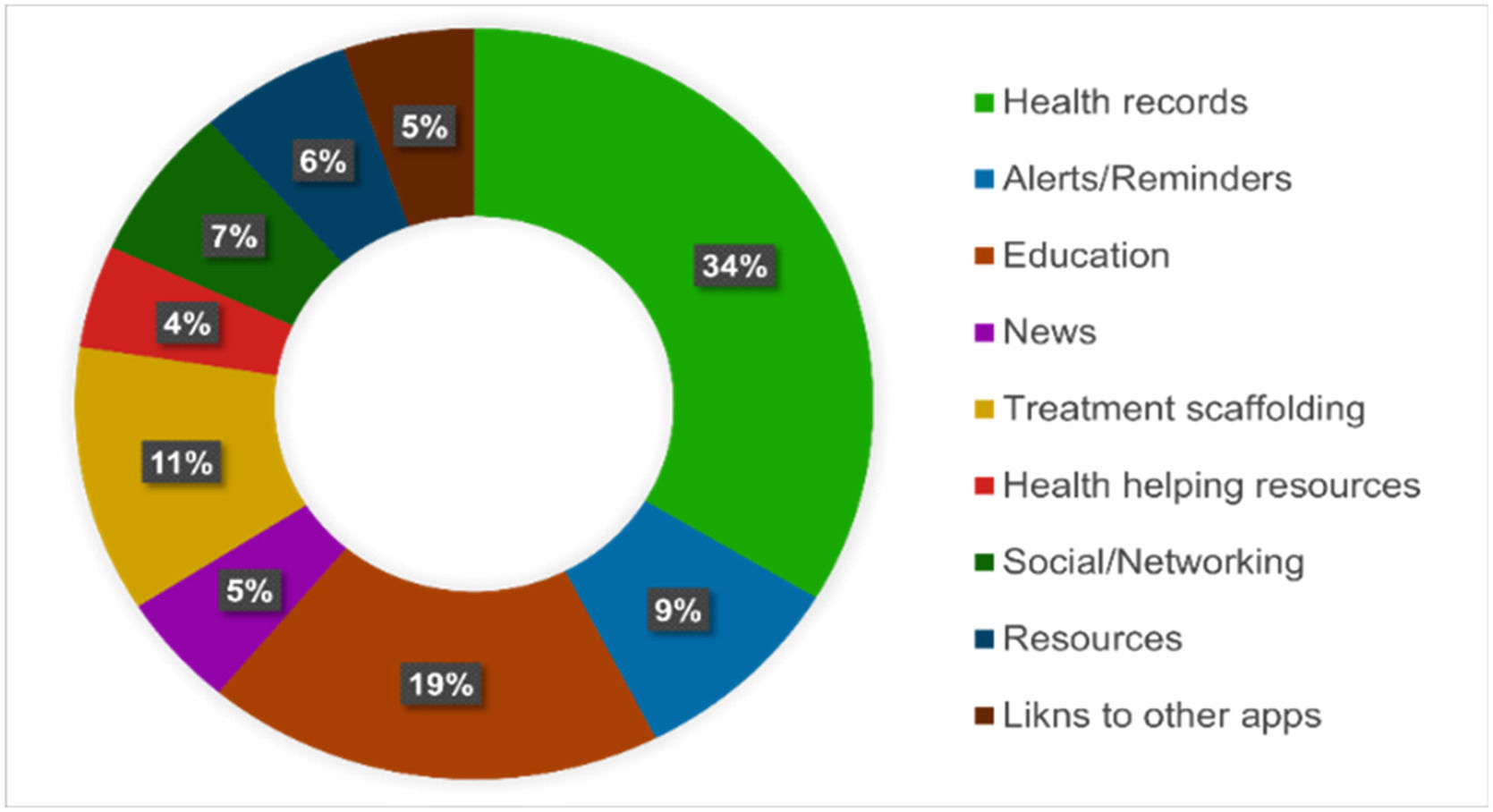
The main application classes identified in this taxonomy include assessment, informative, social/networking, treatment scaffolding, and gamification. Within the assessment category, the two core value propositions include health records and alerts/reminders. For the informative category, the focus lies on news and education. The social/networking category is characterized by the value proposition of “keep me in touch.” In the treatment scaffolding category, key value propositions include sharing reports and connecting with healthcare providers. Finally, the gamification category brings forth two different value propositions: access to resources and links to other vertical solutions or applications. This analytical matching and taxonomy-building process is illustrated in Fig. 3, which shows the interconnectedness of context, stakeholder involvement, requirements, and development in the eHealth app ecosystem.
ResultsAs discussed in (Section Selection of Apps), 20 apps are considered for full feature analysis. The apps are categorized using the framework proposed by Ribaut et al. (2024) and analyzed in terms of their value propositions. The obtained results address the primary objective of this study, which includes analyzing the value proposition and stakeholder alignment of MS-related mobile applications through a multi-step, ecosystem-informed evaluation framework. The structure of the results reflects the three methodological stages: app characterization, stakeholder perspective analysis, and taxonomy development.
Offered featuresAs introduced in Section 3, the features considered for this study have been organized according to the value proposal and presented in Table 4.
Features considered for this study.
When performing the analysis, the two main drivers are analyzed. First, we identify which value proposition the available applications primarily targeted. This distribution is represented by counting how many features correspond to each value proposition (Table 4). In Fig. 4, digital coaching and care management emerge as the most frequently represented functionalities, followed by physical training, cognitive training, and patient education. These results describe the observable presence of functionalities declared by app developers.
As shown in Fig. 5, most apps offer fewer than five functionalities, indicating a limited scope of support. Limited apps, such as Cleo and Emilyn, provide broader and more integrated offerings. This descriptive overview underscores the fragmented nature of current solutions. These observed distributions suggest a pattern: app development tends to emphasize functionalities that are technically easier to implement, such as reminders or general advice, while more demanding or personalized features (e.g., cognitive stimulation or emotional support) remain less common. This pattern may signal a disconnect between implementation convenience and patient-centered priorities, a theme further examined in (Section Demanded features).
Demanded featuresTo respond to the second objective from the patient perspective, findings from a national survey of Spanish patients with MS are integrated. The survey examines the types of mobile applications used by patients, their motivations for choosing their applications, the features they use most, and their overall assessment of the applications. This approach provides an overview of where digital health tools meet MS management and highlights possible lacunae or shortcomings in the available services.
The satisfaction related to the use of digital apps to monitor pathology has been reported in the questionnaire in the sample of Spanish patients with MS, comprising 503 patients, as discussed in (Section Ecosystem-Based Triangulation).
Complementing the patient data, case-based analyses are performed by involving healthcare professionals, pharmaceutical industry representatives, and digital health developers to capture broader ecosystem perspectives. Table 5 summarizes key insights derived from interviews with three core actor groups—technology developers, pharmaceutical firms, and clinical professionals—each playing a distinct role in the design, implementation, and use of MS-related digital tools.
Key Insights from Ecosystem Stakeholders Involved in MS App Initiatives.
The obtained qualitative findings reveal both structural and strategic constraints that influence the development, deployment, and clinical integration of such applications within real-world healthcare settings. The perspectives gathered from these stakeholders offer a valuable contrast to the expectations and experiences of patients, assisting in the contextualization of functional and emotional dimensions associated with mHealth technologies.
Patients with MS reported different reasons for using mobile applications in the management of their physical condition. Most identified the important role of these applications in simplifying life with improved mobility, increasing the quality of life, and helping to self-manage the condition. Several patients identified psychological benefits, implying motivation and encouragement offered by the tools, mainly toward changing or adopting healthier lifestyles.
Some patients commented that the apps helped them monitor their diseases because they owned facilities such as biosensors and digital calendars, which could assist in monitoring symptoms and scheduling appointments. Others lauded the apps because they helped bridge the gap between patients, making it easy to understand each other.
Cognitive and physical exercises through the apps are particularly commended for maintaining mental and physical activity, which the patients consider highly important for effective management.
Knowing the time patients spent on disease-specific applications is important in assessing their level of participation. The weekly usage shows whether these apps are integrated into the daily routine of patients and can serve as a key indicator of their potential impact on disease management.
The functionalities most valued by patients are presented in Fig. 6. According to survey responses, patients place particular importance on features that support cognitive stimulation, emotional well-being, and personalized physical activity. These preferences suggest a desire for apps that go beyond basic tracking or information provision.
While functionalities such as medication reminders and general disease education are appreciated, they rank lower, indicating that patients prefer tools that enhance autonomy and engagement with their health, especially in aspects that affect quality of life.
These results reflect user preferences and perceived value; patients consistently emphasized the importance of feeling monitored, supported, and motivated, dimensions that extend beyond functional utility into emotional and social support.
Insights from interviews with professionals and patient associations provide further context. While patients focus on empowerment and psychosocial support, other stakeholders view apps through the perspective of clinical monitoring or treatment adherence. This misalignment of expectations implies that current apps may underdeliver in areas most meaningful to users.
To fulfill the third objective, the reviewed app features and stakeholder expectations are synthesized into a structured taxonomy of value propositions. This taxonomy reflects the functional orientation of existing apps and highlights gaps in stakeholder alignment, particularly regarding clinical evidence, engagement mechanisms, and integration with care pathways.
For applications other than Cleo, reported usage is minimal and, therefore, insufficient to analyze similar patterns of use. Participants report a mean weekly usage (SD) of 55.5 (74.0) for dedicated mobile applications. The large value of SD underlines variability among users, with a few showing high engagement, whereas others used the apps rarely or not at all.
The most highly rated features by mobile app users in descending order include:
• Read articles on scientific advancements and understanding multiple sclerosis,
• Apps for physical exercise, such as guided therapeutic exercises,
• Self-diagnosis applications based on physical symptoms and sensations (e.g., pain, fatigue),
• Self-assessment apps based on mood and mental state (e.g., feeling depressed, happy),
• Apps for cognitive skills and memory training.
These functionalities, although in a different order, are the most valued by patients who reported not using dedicated apps. Conversely, the least valued features include:
• Storage for clinical test results and data,
• Campaigns for donations and fundraising for multiple sclerosis,
• Medication, appointment, and clinical event tracking.
These features may be rated lower as they are either perceived as redundant with other available tools or less relevant to the immediate challenges of managing MS.
Collectively, the obtained results reveal a persistent misalignment between the functional offerings of MS-related mobile apps and the evolving requirements and expectations of patients and other ecosystem actors. Despite a growing number of available apps, value creation remains fragmented, with only a few applications focused on real engagement, and features often falling short in terms of personalization, usability, and clinical integration. These findings suggest that any meaningful progress in this field is dependent not only on improving individual app functionalities but on rethinking how value is co-created across the digital health ecosystem.
DiscussionThis study is guided by the principle that digital health tools, particularly in the context of chronic diseases such as MS, must be considered as part of a broader service ecosystem, rather than as isolated technologies. The central insight emerging from the obtained results is that low adoption and uneven impact of MS-related apps are caused by structural misalignments among stakeholder expectations, app design, and system-level integration. Addressing this gap requires reframing evaluation and design practices around co-creation, stakeholder alignment, and long-term ecosystem sustainability (Saeedikiya et al., 2025). The findings of this study align with real-world examples in the Spanish MS-app ecosystem. As shown in Table 5, adoption and sustainability depend on technical features, institutional environments, and regulatory conditions.
Given the limited availability of structured datasets and representative sampling frames for stakeholders such as healthcare professionals, pharmaceutical industry representatives, and digital health technology providers, this study adopts a case-based qualitative approach to incorporate stakeholder perspectives. The case method is a well-established strategy for exploring complex, context-dependent phenomena where generalizable quantitative data are unavailable. Through purposive selection and guided interviews, this study captures key patterns, barriers, and strategic perspectives that shape the deployment and perceived value of mHealth applications for multiple sclerosis. While the proposed approach does not yield statistically generalizable findings, it contributes depth and contextual richness that complement the quantitative survey data collected from patients, thereby supporting a triangulated and ecosystem-informed interpretation of results.
Although the adopted methodology offers rigor in the form of empirically rooted frameworks and data triangulation, some limitations exist. First, the analysis of mHealth apps relies on publicly available app store metadata, which may be limited or biased, particularly in relation to download numbers, update frequency, and user ratings, which are skewed in nature. Second, survey triangulation data are based on self-reported information by Spanish patients with MS. The data may be subject to recall bias, social desirability bias, and potential non-representativeness of the overall MS population. These issues do not invalidate the findings of this study but support contextualizing results within methodological constraints. Future studies can utilize direct use metrics and blend in clinical data along with patient-reported experience.
Theoretical contributionMS is a highly individualized disease, with symptoms and progression rates varying widely among patients. Consequently, understanding the type of support that patients find comforting can provide valuable insights for healthcare providers and researchers to design more tailored and effective management strategies.
From the triangulation of findings—combining features identified in existing apps with patient feedback—several key points are deduced. In the following sub-sections, four app evaluation dimensions are discussed in detail (Fig. 3).
ContextThe development of mobile applications for MS has emerged as a key component in the personalized management of the disease, providing tools for symptom monitoring, treatment adherence, and patient education. However, the digital ecosystem in this field continues to face challenges in terms of accessibility, uptake, and clinical effectiveness.
In this study, a total of 31 MS-related applications are identified in the Spanish market. After applying the eligibility criteria, the number of applications is reduced to 26, of which six require an access code and cannot be analyzed: MeTime MS, MSCopilot Detect, MS-Lifer, Bezzy MS: Multiple Sclerosis, and MS Sherpa. Previous studies (Salimzadeh et al., 2019) have identified 164 applications at the international level. After applying eligibility filters, this number is reduced to 104, with 27 specifically focused on MS self-management. Although the number of selected applications in the Spanish market is comparable to those identified by Salimzadeh et al. (2019), survey results (Tabuenca et al.) indicate a low level of uptake among patients, which can be partially attributed to linguistic barriers. Only 45 % of the analyzed applications include Spanish as a language option, compared to 90 % that offer Spanish and/or English. This limitation can restrict accessibility and engagement among Spanish-speaking patients, potentially discouraging their use of these digital tools. Similar concerns about linguistic accessibility have been raised by Salimzadeh et al. (2019), who identify language availability as a relevant factor influencing the adoption of MS self-management applications.
The uptake of the applications in Spain, measured in terms of download numbers from the App Store, shows significant variation. Cleo and Belong MS each record approximately 100,000 downloads, whereas others, such as Floodlight and EMControl, barely surpass 1000 and 100 downloads, respectively. The absence of detailed data for several applications further suggests marginal usage in several cases. However, the available data do not allow for a precise assessment of real adoption levels. The Play Store only provides download figures in broad ranges (e.g., +5 K or +10 K), making the determination of the exact number of users challenging, particularly for applications with lower uptake rates where variations within these ranges could be significant. Additionally, the App Store does not provide any information on the number of downloads, further limiting the ability to gauge the actual reach of the applications across different platforms. The findings are particularly relevant given that survey data indicate that whilst most patients with MS in Spain (69.3 %) use Android smartphones, a significant proportion (26.1 %) use iPhones (Tabuenca et al.). Since the App Store does not provide download figures, the current statistics may not fully capture the uptake of MS-related applications among iOS users, potentially underestimating their overall reach. These platform-related discrepancies reflect broader structural misalignments in the digital health ecosystem, supporting the idea that adoption barriers are not solely user-dependent but arise from broader systemic misalignments, consistent with the assumptions of H2.
From a technological compatibility perspective, availability across different operating systems is critical for ensuring accessibility to digital solutions. In Spain, 75 % of the identified applications are run on Android devices, aligning with the predominance of this operating system in the country. The trend is consistent with the findings of Salimzadeh et al. (2019), where 75 % of the analyzed applications are accessible on Android, suggesting a correlation between the supply of applications and the distribution of mobile device usage in each region. However, despite the predominance of Android, iOS users are not at a disadvantage in terms of app availability, as 90 % of the identified applications are compatible with iPhones. Therefore, while Android remains the dominant platform among MS patients, accessibility to digital health solutions is generally well balanced across both operating systems. Consequently, persistent adoption gaps are unlikely to be explained by technological incompatibility alone. Instead, they emphasize other systemic barriers—such as functional misalignment, digital literacy challenges, or insufficient clinical integration—as proposed in H2.
A qualitative analysis of user reviews underscores another important aspect in evaluating the impact of these applications. Most MS-specific applications in Spanish have a low number of reviews, limiting the ability to accurately assess their perceived value and real utility. Cleo stands out as an exception, with 141 reviews on Google Play and 25 on the App Store, making it one of the few MS-related applications with a substantial number of user evaluations. This finding partially reflects those obtained by Ribaut et al. (2024), who observed that user engagement data in mHealth applications is often limited or unsystematically collected, hindering both the generation of design insights and the evaluation of experiential value throughout the app lifecycle.
From a quantitative perspective, applications available in Spain have an average rating of 4.5 out of 5 stars. However, this metric should be interpreted with caution, as its reliability is compromised by the low number of reviews in several cases. In the reference study by Salimzadeh et al. (2019), the average rating has 4 stars. However, the rating is based on a larger sample of applications with a greater number of user evaluations. This suggests that the higher ratings observed in Spain may be skewed due to the limited representativeness of the available reviews, potentially overstating the perceived quality of these applications (Ribaut et al., 2024). These distortions in perceived quality hinder an accurate understanding of experiential value to users, highlighting the need for more comprehensive and structured evaluation frameworks, as outlined in H1.
Finally, the economic accessibility model of these tools is another relevant aspect influencing their uptake. In the Spanish market, all analyzed applications are free, eliminating financial barriers to access but raising concerns about the sustainability of their development and updates. In a study by Salimzadeh et al. (2019), 94.2 % of applications were free, but those requiring payment had an average cost of $1.97. The absence of monetization models in Spain implies that the funding for the applications relies on alternative sources, such as grants, partnerships with healthcare institutions, or integrated advertising, which impact service quality and continuity. While Gromisch et al. (2021) included app pricing in their evaluation, they did not explicitly examine the relationship between monetization and sustainability. The lack of robust funding models reveals structural constraints that compromise both the continuity of value delivery (H1) and the systemic conditions necessary for sustained adoption (H2).
Simultaneously, AI integration is approached cautiously, addressing ethical risks such as bias in health assessments and decision-making without human oversight. Legal and regulatory challenges, particularly those related to data privacy, patient consent, and transparency, are central to maintaining trust in AI-driven healthcare systems (Santa Soriano & Valdés, 2021). Additionally, governments must balance transparency and regulation as AI systems increasingly surpass human clinicians in decision-making (Yu et al., 2018).
Collectively, the results discussed in this section support both H1 and H2. H1 is reinforced by the observation that the perceived value of MS applications is shaped by feature design and their integration into broader technological, financial, and regulatory ecosystems—dimensions often overlooked in traditional usability assessments. Further, H2 is substantiated by persistent adoption gaps that cannot be attributed solely to user-level factors but instead emerge from deeper structural misalignments such as linguistic inaccessibility, platform fragmentation, absence of funding models, and insufficient clinical integration. These systemic frictions limit not only adoption, but the continuity and legitimacy of digital health interventions, pointing to the requirement for a more ecosystem-aware approach to app development and evaluation.
Stakeholders involvementThe development of mobile applications for MS involves diverse stakeholders, each contributing distinct expertise, resources, and strategic objectives (Ertz et al., 2025). These stakeholders include pharmaceutical companies, health-tech firms, patient associations, research institutions, and collaborative initiatives between technology developers and the pharmaceutical industry experts (Table 5). Understanding their roles provides insight into the value creation mechanisms underlying these digital health solutions (Table 5). The multiplicity of actors reflects the systemic complexity discussed in prior literature (Cennamo & Santaló, 2019), where alignment among stakeholder objectives is key to platform success.
Pharmaceutical companies have developed various digital health applications to enhance patient adherence to treatment protocols. Notable examples include EMControl by Novartis, Floodlight MS by Roche, Cleo by Biogen, and MS Lifer, funded by Merck KGaA. Additionally, MSCopilot® Detect, developed in collaboration between Ad Scientiam and Sanofi, goes beyond self-management by actively contributing to medical research as a certified medical device for symptom evaluation in multiple sclerosis patients. These applications not only support patient engagement but also enable pharmaceutical companies to integrate digital health solutions into clinical practice. Beyond development, they play a crucial role in promoting uptake among healthcare providers and patients, thereby shaping the ecosystem in which these applications operate (Gawer & Cusumano, 2014). In line with H1, the initiatives demonstrate how pharmaceutical-led applications partially support patient engagement and cognitive participation. However, our findings suggest that coordination with other actors, such as clinicians and caregivers, is often limited, thereby constraining the broader value co-creation potential expected in service-dominant logic ecosystems.
Health-technology firms bring advanced technological capabilities to the development of MS applications. Belong.life, an American company specializing in AI and big data solutions, applies these technologies to create personalized digital health services. Other key contributors include Evidenze, the developer of HugoEM; Teracat, responsible for miEsclerosis; BeCare Link, which created BeCare MS, a remote assessment tool for MS patients; and icometrix, which developed icompanion, a clinical monitoring application. Although not all of these companies focus explicitly on AI, they integrate data-driven technologies to enhance predictive analytics, symptom tracking, and patient engagement, aligning with broader trends in AI-enabled healthcare business models. Furthermore, they foster collaboration with other stakeholders (Warner & Wäger, 2019). Compared to earlier studies, such as Warner and Wäger (2019), the analysis in this study reveals that although these firms enhance personalization and data intelligence, their integration with institutional healthcare systems remains limited. This finding supports the emphasis of H2 on systemic misalignments as critical barriers to adoption. Furthermore, the results align with the observations of Heesen et al. (2023), who report fragmented adoption and weak ecosystem coordination despite strong user interest.
Beyond corporate-driven initiatives, non-profit organizations and research institutions play a crucial role in app development. The American MS association has developed MSAA-My MS Manager, positioning itself as a key technology in promoting awareness and patient support. Another notable example is Live Well Hub by Overcoming MS, an application developed by the Overcoming MS organization, which provides a comprehensive wellness program for multiple sclerosis patients, promoting healthy habits and disease education. Additionally, EM Navarra, developed by the Asociación EM Navarra in Spain, aims to improve the quality of life for patients with MS through digital support and resources. MS Tim, created by MS TIM CROATIA, is another significant initiative, designed to enhance communication and support within the MS patient community. These findings support the ecosystem perspective highlighted in H1, showing that applications originating in non-profit or academic contexts tend to adopt more holistic approaches aligned with diverse stakeholder needs. However, they often lack the technological scalability or adoption reach typical of pharma- or tech-driven platforms.
Associations serve as essential dissemination channels, advocating the use of digital tools within patient communities. Meanwhile, research institutions such as the Institut d’Investigació Biomèdica de Girona have developed EM Seguiment, with a primary focus on data collection for research. These applications enable large-scale patient data aggregation, supporting biometrics-driven research on disease progression, treatment efficacy, and lifestyle impact. The inclusion of research-driven applications within the broader digital ecosystem reinforces the concept of healthcare meta-ecosystems, where interconnected stakeholders collaborate to create collective value rather than competing for the same user base (Cennamo & Santaló, 2019; Triantafyllidis et al., 2023).
In summary, the analysis of stakeholder roles confirms both H1 and H2. H1 is validated from the evidence that value in MS mobile applications is co-created across a network of actors—ranging from pharmaceutical firms and tech companies to non-profits and research institutions—each contributing distinct yet complementary resources. However, the realization of this value depends on the degree of alignment and coordination among these actors. Conversely, H2 is supported by the limited integration of health-tech innovations with institutional systems and clinical workflows, which undermines adoption despite high user interest and technical potential. These systemic misalignments, whether organizational, infrastructural, or regulatory, highlight the need for ecosystem-level governance to unlock the full value creation potential of MS digital health platforms.
DevelopmentThe development of mobile applications tailored for MS management requires a comprehensive approach encompassing various stages, methodologies, and stakeholder contributions. Therefore, an effective development process should prioritize patient-centric design, ensuring usability relevance and alignment with the preferences of individuals with MS (Salimzadeh et al., 2019). Given that digital health solutions should integrate with broader healthcare ecosystems, ensuring interoperability and compliance with clinical standards is essential for maximizing uptake and long-term impact (Ribaut et al., 2024). Furthermore, collaboration between healthcare professionals, researchers, and technology developers plays a crucial role in optimizing app functionalities and enhancing their clinical utility (Giunti et al., 2018b). This multi-actor coordination reflects the logic of H1, where the perceived value for patients is consistent with how well apps align with the roles and expectations of other ecosystem actors.
Accordingly, the inclusion of end-users in the design process is a fundamental factor in the success of healthcare applications. Co-creation and user-centric design methodologies ensure that applications align with patient requirements, clinical workflows, and evolving treatment paradigms. This approach aligns with previous findings emphasizing the lack of patient-centered design and the limited involvement of healthcare professionals in most MS apps (Giunti et al., 2018a). While some applications are developed with a clear focus on patient engagement and self-management (Salimzadeh et al., 2019), others are designed as data collection tools, requiring high levels of usability and interoperability with healthcare systems (Giunti et al., 2018b). For instance, Floodlight MS (Roche) and EM Seguiment (Institut d’Investigació Biomèdica de Girona) are explicitly designed to gather data for clinical research, facilitating the integration of real-world evidence into multiple sclerosis studies. Similarly, icompanion (icometrix) and Hugo EM 2.0 (Evidenze) contribute to medical research by collecting patient-reported outcomes and other health indicators. However, not all research-oriented applications are consistently categorized under Medicine or Medical in app stores. While Floodlight MS and icompanion appear under medical categories in both iOS and Android, other apps, including Hugo EM 2.0 and Belong MS Multiple Sclerosis, are listed under broader categories such as Health & Fitness in iOS, which may impact their visibility and perceived credibility among users seeking clinical-grade applications. As highlighted by Gromisch et al. (2021), the usability and accessibility of MS apps are frequently undermined by design decisions and categorization issues that do not account for patients’ cognitive or motor limitations. Such inconsistencies in classification and access potentially reinforce H2, illustrating how systemic frictions, beyond usability, may hinder effective adoption.
These distinctions highlight the necessity of tailoring app functionalities to specific use cases, ensuring that MS applications effectively balance patient usability with the requirements of clinical research and healthcare integration (Ribaut et al., 2024). This challenge is particularly acute in the Spanish context, where digital literacy barriers and opaque system integration further exacerbate the low adoption levels described in H2. Moreover, while some applications clearly state their data-sharing policies, either by explicitly mentioning that they do not share data with third parties or by detailing how data is used for research, others provide ambiguous or insufficient information, raising concerns about transparency in data privacy and patient consent. Although some applications provide transparency regarding their data management practices, others lack clarity on whether and how AI-generated insights are stored and utilized, further complicating regulatory compliance and patient trust. For example, Pre-Meet: MS states that all data are voluntarily entered by users but does not specify its further use or whether AI-driven analytics are employed. Similarly, Turnto Daily Breakthroughs claims that it does not share data with third parties, but its data storage and AI usage policies remain unclear. Additionally, publicly available information regarding update frequency and version history for numerous applications is limited, making it difficult to assess their long-term maintenance and reliability, which are crucial factors for both clinical uptake and patient trust. These systemic limitations not only diminish perceived value but also represent structural barriers to co-creation and adoption, reinforcing the mechanisms outlined in H2.
The integration of AI-driven functionalities in MS applications is emerging as a transformative factor in digital health innovation. AI not only enhances user experience through predictive insights but also enables automated data analysis, facilitating more efficient symptom monitoring and personalized recommendations (Breidbach & Maglio, 2020; Colther & Doussoulin, 2024). Some applications, such as Pre-Meet: MS (developed by ARDIREO) and Turn to Daily Breakthroughs (a healthtech startup based in Australia), have incorporated AI-driven features to enhance patient engagement and clinical insights. However, such advancements require robust infrastructure for data storage, processing, and security. This technological advancement, although promising in terms of value generation, requires ecosystem-wide alignment to ensure interoperability, trust, and sustainability, as key dimensions highlighted in H1. The high costs associated with installing, maintaining, and adapting complex data storage systems remain a key challenge in digital health uptake (Lu & Taghipour Atour, 2025; Wamba-Taguimdje et al., 2020). These economic and technical barriers are particularly pronounced in under-resourced contexts, potentially limiting adoption despite user interest, as posited in H2.
Conversely, the development of MS-related applications reflects the evolving nature of healthcare ecosystems, where technological innovation, cross-sector collaboration, and patient-centered design converge to create value for multiple stakeholders. The diversity of developers—from pharmaceutical companies and tech firms to research institutions and patient associations—illustrates the dynamic interplay of business and non-business actors in shaping digital health solutions. This convergence exemplifies the systemic logic of H1, wherein the value perceived by patients arises from coordinated interactions across the entire ecosystem, rather than from isolated app features. Beyond individual applications, the integration of MS-related digital tools within broader healthcare ecosystems is becoming increasingly relevant. Rather than operating in isolation or competing for the same user base, these applications are progressively aligning under a meta-ecosystem framework, where interoperability between clinical data repositories, research platforms, and digital health solutions fosters a shared value chain. This shift towards platform envelopment allows for a more seamless exchange of information across pharmaceutical firms, patient associations, and tech providers, enhancing both research potential and patient outcomes. For instance, icompanion (developed by icometrix) is designed for patient self-monitoring and to contribute real-world data to clinical research, bridging the gap between patient-reported outcomes and clinical practice. Similarly, Pre-Meet: MS (developed by ARDIREO) aims to enhance the engagement of patients with MS while integrating relevant health data into broader research initiatives. Similar dynamics have been observed in systems such as MSdialog, which improve communication between patients and healthcare professionals by integrating patient-reported outcomes into clinical workflows (Greiner et al., 2015). These applications exemplify how digital health solutions are evolving beyond standalone tools to become interconnected components within the larger healthcare ecosystem.
Recent studies have highlighted the transformative potential of AI-driven advancements, enhanced data integration strategies, and expanded cross-sector collaborations in the development of MS applications (De Brouwer et al., 2024; Eshaghi et al., 2021). MSBase registry exemplifies successful cross-sector collaboration, collecting data from multiple institutions worldwide to enhance research and patient care in MS. These examples illustrate the critical importance of co-creation, usability, and adaptability to emerging technologies in ensuring the long-term impact of MS applications within the healthcare landscape.
Considering the findings of this study, both H1 and H2 are supported. H1 is validated through the demonstrated importance of ecosystem alignment and stakeholder integration in shaping perceived value, while H2 is corroborated by persistent gaps in usability, transparency, and infrastructural readiness that continue to limit adoption despite growing interest. This dual validation is consistent with the gaps and future directions identified across the literature, including calls for co-designed, validated, and interoperable applications that address real-world adoption barriers (Heesen et al., 2023; Marziniak et al., 2018)
Features and requirementsFirst, although there are numerous MS-focused apps available, the actual usage is concentrated on a limited number of applications. Moreover, the average time spent on such apps per week suggests generally low levels of engagement. Hence, despite their availability, several apps may not satisfy patient requirements or align with their preferences. As Gromisch et al. (2021) emphasized, digital tools for MS often fail to accommodate patients' cognitive, motor, and sensory challenges, which can be attributed to low engagement rates despite initial interest. The findings align with established literature, with the average age of MS diagnosis (M = 35.9 years) consistent with the disease’s typical onset in early to middle adulthood. This underscores that MS predominantly affects younger and middle-aged adults rather than the elderly population. Concerning the feasibility of performing regular mobile assessments, patients have expressed a preference for minimal disruption. The responses vary, with 48 % willing to perform assessments more than once a week, 25 % opting for a monthly frequency, and 18 % unsure. This variability suggests that, while frequent monitoring is acceptable for some, others require flexibility due to lifestyle constraints or concerns about the burden of engagement. Apps such as HugoEM and Icompanion, which offer options for event-based logging rather than daily tracking, may cater better to these diverse requirements. This supports H2, illustrating how adoption depends not only on technical functionality but also on the adaptability of apps to heterogeneous user contexts. Another insight concerns the value proposition and coverage of key functionalities. The preference for monitoring MS progression highlights the growing interest in wearable technologies, such as sensor-equipped smart socks, which can deliver crucial data on mobility. This finding is echoed by Alexander et al. (2021), who identified the lack of validated tools for fatigue and cognitive monitoring, despite patient demand for multi-domain tracking. Similarly, apps such as Floodlight provide digital assessments of hand dexterity and gait disorders, ensuring objective tracking beyond subjective self-reports. Conversely, Icompanion integrates standardized neurological tests such as EDSS and Neuro-QoL, reducing subjectivity in patient-reported data. The survey results indicate that core functionalities related to health records are the most valued (34 %); however, substantial interest lies in educational resources (24 %), highlighting the opportunity to enhance patient engagement through well-structured informational tools. For instance, BelongMS offers access to clinical trial publications, while MSAA-My MS Manager incorporates motivational content and lifestyle advice. The preference for information delivery formats can be a critical issue; for example, MSAA-My MS Manager includes audiovisual materials, which can be particularly beneficial for patients with vision impairments. These insights reinforce H1 by demonstrating that value is co-created not only through clinical functionalities, but also through features that align with diverse user needs and limitations. However, while AI has the potential to further personalize these resources and improve accessibility, its lack of transparency raises concerns among patients. Algorithmic bias and the complexity of AI-driven insights may lead to unequal recommendations and reduced trust in data usage (Santa Soriano & Valdés, 2021). Clear oversight is essential to prevent AI from reinforcing biases in symptom tracking and treatment guidance, ensuring it enhances rather than complicates patient engagement (Wirtz & Müller, 2019).
Beyond the gap in educational resources, a similar misalignment exists in data-sharing functionalities, which are crucial for real-time monitoring and patient-provider communication. "Health helping resources" represent only 4 % of perceived value, whereas general "resources" constitute 6 %, highlighting a gap in tools that facilitate patient-provider communication and real-time health monitoring. This gap underscores the importance of data-sharing functionalities, which remain underdeveloped despite strong patient interest. The findings align with those reported by Giunti et al. (2018) and Gromisch et al. (2021). The study confirmed limited development of interoperable features and weak integration with clinical systems in most MS-related apps. Over 90 % of respondents expressed a willingness to share wearable data with healthcare teams, demonstrating high trust in medical professionals and an openness to collaborative disease management. Apps such as Cleo, which provide direct access to MS-specialized nurses, align well with this trend. The finding supports H1 by illustrating that perceived value is contingent upon how well app features, such as data sharing, are integrated into broader healthcare coordination mechanisms.
Nevertheless, effective data-sharing requires clear governance frameworks to address privacy, cybersecurity, and regulatory compliance. Although some applications explicitly state their data-sharing policies, others remain ambiguous, raising concerns about transparency in patient consent and AI-driven data usage (McGraw & Mandl, 2021). For example, Cleo collects personal information from users, including email, country of residence, and topics of interest related to MS. However, its privacy policy does not explicitly state whether user data are shared with third parties or if AI-driven analytics are employed in personalizing content and recommendations. Similarly, Pre-Meet: MS states that all data are voluntarily entered by users but does not specify its further use or whether AI-generated insights are applied to patient information. This lack of clarity raises concerns about data governance and how patient information is managed within these apps. These deficiencies reinforce H2, as they reflect systemic misalignments between user expectations for ethical transparency and the actual data practices of MS apps—undermining trust and reducing adoption potential. Strict regulatory standards often limit providers from sharing protected health information without explicit consent, making governance models crucial for balancing innovation with ethical and legal responsibilities (Yu et al., 2018).
In addition to medical tracking, engagement strategies play a critical role in user retention. Apps such as Cleo and EM Seguiment implement goal-setting mechanisms that reward adherence, encouraging continued participation. The inclusion of gamified cognitive and motor exercises, as seen in Floodlight, can further enhance engagement. These strategies are consistent with the study by Giunti et al. (2018), who advocated for features that sustain motivation—such as gamification—to better align with patient needs and support long-term use. They reinforce H1 by illustrating how value is co-created when app features integrate motivational frameworks that resonate with patient preferences and disease experience.
Finally, reminder functionalities for medication and appointments are universally present across MS-focused apps. However, some patients prefer to limit constant reminders of their condition, emphasizing the need for customizable notification settings. This supports H2, as rigid or intrusive functionalities may lead to disengagement, particularly when they fail to consider emotional and psychological dimensions of chronic illness, as noted by Gromisch et al. (2021).
These findings highlight the importance of designing adaptable, patient-centered digital health solutions that balance structured medical tracking with personalized engagement tools. Future app development should prioritize flexibility in monitoring frequency, improved data-sharing capabilities, and diversified educational content, ensuring that the evolving needs of patients with MS are met effectively. Simultaneously, AI integration should be approached cautiously, ensuring that its ethical, legal, and regulatory challenges are adequately addressed to prevent unintended risks while maximizing its potential benefits. As emphasized by Wirtz and Müller (2019) and Heesen et al. (2023), AI deployment in clinical contexts must be transparent and aligned with ethical principles to maintain user trust and system integrity.
In summary, the evidence presented in this section supports both H1 and H2. H1 is validated through the demonstration that value in MS applications emerges from the alignment of clinical, motivational, and informational features with the expectations of a broader healthcare ecosystem. Functionalities such as data sharing, educational customization, and engagement mechanisms gain relevance when they are interoperable and ethically governed. Furthermore, H2 is confirmed, as persistent barriers to adoption, including usability constraints, insufficient personalization, and lack of transparency in data governance, reflect deeper systemic misalignments that limit the effectiveness of otherwise well-intentioned tools. These findings underscore the need for MS apps to evolve beyond isolated digital products toward integrated, adaptable platforms embedded in coordinated care pathways. These insights are drawn from survey and interview data collected among MS patients, non-users, and stakeholders in Spain, reflecting the perspectives and priorities of a predominantly Spanish-speaking healthcare context.
Managerial contributionThe findings of this study offer key managerial insights into the uptake, usability, and engagement patterns of mobile health applications for patients with MS. By contrasting user and non-user perspectives, this research identifies functionalities with strong cross-group demand, such as educational content, cognitive training, and guided physical exercises, and highlights where alignment between desired and actual usage is lacking. Understanding both user and non-user perspectives provides a roadmap for developers, healthcare professionals, and policymakers to optimize these digital solutions for improved patient outcomes. Survey results confirm that the functionalities most frequently used by current MS app users closely align with the features desired by non-users (Fig. 6).
However, non-users still perceive these functionalities as unmet needs, suggesting that accessibility, communication, and onboarding strategies require significant improvements. For example, medication tracking and clinical appointment reminders are widely used by nearly half of current users but are prioritized by less than one-third of non-users. Thus, some functionalities gain perceived value only after adoption and may not serve as strong initial motivators. The demand for educational resources, cognitive training tools, and guided physical exercises remains consistent across both groups, emphasizing their pivotal role in patient self-management. The most frequently used functionalities among current app users include:
• Reading articles on scientific advancements and understanding MS (71.76 %)
• Applications for cognitive training and memory enhancement (51.76 %)
• Guided physical exercises (42.35 %)
• News and tips on living with MS (55.29 %)
Similarly, non-users identify their most desired features as:
• Guided physical exercises (64.46 %)
• Reading articles on scientific advancements and understanding MS (56.76 %)
• Applications for cognitive training and memory enhancement (56.76 %)
This strong alignment reinforces the importance of these functionalities in patient self-management. However, despite this consistency, some features exhibit significant gaps between expected and actual uptake. For example:
• Biosensor-based diagnostic applications (e.g., wearables including smart socks and bracelets) have been considered useful by 42.97 % of non-users, yet only 10.59 % of current users report active usage. This indicates that while technology holds promise, real-world uptake remains limited, attributed to usability barriers or a lack of awareness regarding its benefits.
• Medication tracking and clinical appointment reminders were widely used by 49.41 % of app users, yet only 28.12 % of non-users prioritized them. This suggests that while these functionalities become valuable post-uptake, they may not serve as strong initial motivators for new users.
The findings further indicate that MS app usage is highly concentrated among a small number of applications, with Cleo being the dominant platform among surveyed users. While this demonstrates strong user loyalty, it also highlights limited market diversity, which may restrict innovation and personalized solutions. Policymakers and funding bodies could encourage competition through innovation grants, pilot programs in hospitals, and open standards that lower barriers for new entrants. Expanding the reach of alternative applications and promoting competition in the MS digital health space could foster the development of more adaptable and patient-centric tools such as the Hugo app.
Given that most MS-specific applications remain free, their long-term sustainability is a critical concern. Developers and stakeholders must explore alternative business models, such as partnerships with healthcare institutions, integration into clinical trials, or subscription-based premium features, to ensure continuous improvement and maintenance of these digital health tools (Kohtamäki et al., 2019).
From a design perspective, developers should:
− Integrate core patient priorities early in the development process, ensuring that the most demanded functionalities are embedded in intuitive, accessible interfaces.
− Employ progressive onboarding with tutorials, gamification, and AI-driven personalization to maintain engagement beyond initial adoption.
− Enhance clinical interoperability to allow seamless data exchange with electronic health records, facilitating physician recommendations and integration into routine care.
From a healthcare provider perspective, clinicians can leverage these insights to guide patients toward applications that address self-management needs, recommending tools that combine medical reliability with features patients find motivating. Structured implementation programs, supported by training sessions, patient workshops, and inclusion in rehabilitation plans, can improve uptake and sustained use. Moreover, insights from clinician interviews (Table 5), particularly the case of Floodlight MS, underline that even clinically robust tools can face adoption barriers when hospital-level approval and data governance issues are not addressed, reinforcing the need for early stakeholder engagement and alignment with institutional requirements.
From a policy perspective, findings suggest the need for:
• National or regional quality certification frameworks to ensure app safety, data protection, and evidence-based content.
• Public–private partnerships to sustain free or low-cost access, balancing economic viability with inclusivity.
• Incentive schemes for integrating validated MS applications into healthcare delivery, potentially linking usage data to performance-based reimbursement or research initiatives.
In Spain, all identified MS-specific applications are free to patients. However, strengthening clinical and economic evaluation to demonstrate cost-effectiveness can increase the likelihood of these tools being eligible for public healthcare funding, ensuring their integration and long-term availability within the ecosystem. Such mechanisms can prevent situations such as Floodlight MS, where a clinically promising tool has been discontinued despite its potential benefits, or Cleo, the most widely used app among patients, which has been withdrawn from the market, both cases illustrating the risks of relying on tools without a secure funding and implementation pathway.
Therefore, the successful development and uptake of MS applications depend on a multidisciplinary collaboration involving healthcare professionals, UX/UI designers, data scientists, AI specialists, regulatory experts, and technology providers (Hafeez et al., 2025; Warner & Wäger, 2019). This collective effort ensures clinical relevance, enhances usability, integrates predictive analytics, and assures compliance with data privacy laws while facilitating interoperability within the broader healthcare ecosystem (Chen et al., 2024). Such platforms can enhance patient self-management, feed into real-world data collection for clinical research, and foster collaboration among developers, clinicians, researchers, and regulators, maximizing both clinical impact and system-wide value. In Spain, this collaboration can be extended to regional health authorities and regulatory bodies to ensure that new applications meet the criteria for public healthcare funding and linguistic accessibility, facilitating their broader adoption within the decentralized system. To maximize uptake and long-term impact, key strategies include simplifying onboarding through intuitive design, leveraging AI-driven personalization, and strengthening integration with healthcare providers via direct communication and data interoperability (Gromisch et al., 2021). Additionally, raising awareness through targeted education campaigns and patient advocacy can drive engagement, while securing sustainability through public-private partnerships and hybrid monetization models will ensure continued innovation and accessibility (Santa Soriano & Valdés, 2021). This ecosystem-driven approach enables MS applications to evolve from standalone tools into integrated digital health platforms that enhance patient self-management and contribute to real-world data collection for improved care outcomes (Palmié et al., 2022).
By addressing these strategic areas, MS applications can evolve from passive tracking tools into comprehensive digital health solutions that empower patients, improve disease management, and foster greater collaboration between stakeholders in the MS healthcare ecosystem.
Underlying barriers to patient adoptionWhile the potential of MS-specific mHealth applications is generally recognized, our findings indicate that their restricted use arises from a set of concrete, practical barriers directly affecting patients' willingness and ability to embrace them. Most prominent among the listed issues is that of usability and accessibility. A majority of the systems do not sufficiently cater to the cognitive, motor, or visual impairments common in MS, resulting in interfaces that are difficult to use, reminders that are poorly flexible or poorly adjustable, and functionality that does not adapt to shifting patient demands. These disabilities stifle extended use, even when initial zeal is high (Gromisch et al., 2021; Salimzadeh et al., 2019).
Second, digital literacy remains a barrier to adoption. Although survey respondents indicated a strong interest in more advanced functionalities such as cognitive training or IoT-based monitoring, usage is low. This disparity is an indicator that patients may not have the digital skills, comfort level, or technical support required to use these tools as a standard part of their routine lives (Grijalvo et al., 2024; Ribaut et al., 2024; Shatila et al., 2025).
Third, cultural and language accessibility are relevant barriers within the Spanish context. The option for Spanish is provided in only 45 % of analyzed applications, which severely restricts access for non-English speakers. Not only does this constrain adoption, but it also continues to reinforce injustices of who can benefit from these technologies (Salimzadeh et al., 2019; Yang et al., 2025).
Fourth, privacy and trust concerns diminish patients' trust. Interviews reveal that a lack of transparency in the way data are being used, shared, or stored, particularly in apps linked with commercial or research purposes, undermines patient participation willingness. Unclear data governance communication further diminishes feelings of safety and reliability (Bernardo et al., 2024; Ribaut et al., 2024).
Fifth, adoption is constrained by the absence of integration into clinical practice. Although apps with informative surveillance features have been designed, a limited number of apps have been incorporated into routine healthcare practice or advocated by healthcare professionals. Without support and integration into care processes, patients consider these tools to be marginal or discretionary, not core to disease management (Zayas-García & Cano-de-la-Cuerda, 2018; Jiao et al., 2025).
Finally, sustainability challenges in the ecosystem come into consideration. The majority of the applications are free, have volatile funding, or are seldom updated. Patients notice if an app is poorly maintained or has little community engagement, and this discourages prolonged use and undermines trust in the app marketplace in general (Grijalvo et al., 2024; Salimzadeh et al., 2019).
Cumulatively, the discussed challenges indicate that low adoption is not a matter of patient motivation or technology availability. Rather, it is a complex interplay of usability, literacy, trust, accessibility, and integration issues at the systemic level. By making these issues transparent, the current debate underscores that greater uptake requires immediate, pragmatic action at multiple levels, ranging from inclusive design and language support to data governance transparency and greater clinical support, to mention just the broader ecosystem alignment emphasized in our conceptual framework (Jiao et al., 2025.
ConclusionThis study presents an in-depth analysis of digital apps available in the Spanish market for MS, incorporating insights from a large population of Spanish MS patients and identifying areas requiring attention from app designers. The research is guided by two primary research questions and their corresponding hypotheses.
Drawing upon the multi-stage methodology outlined in this study, which includes a systematic review of mobile applications, ecosystem-based triangulation with patient survey data, and insights from key stakeholder interviews, the findings of this study provide a comprehensive understanding of value creation and digital adoption in the MS app ecosystem.
In addressing RQ1 and H1, our findings validate the premise that value creation in MS mobile applications is a multifaceted process embedded within a broader digital health ecosystem. The analysis of the features offered reveals a concentration on functionalities such as health records, alerts, and education. However, patient-reported preferences emphasize a stronger demand for cognitive stimulation, emotional well-being, and personalized physical activity tools, which are less comprehensively covered by existing apps. This misalignment highlights that while apps offer foundational support, the perceived value by patients is contingent upon how well these features are integrated into a coordinated value proposition that includes the perspectives and needs of clinicians, caregivers, and developers. We observe that applications originating from pharmaceutical companies and health-tech firms often focus on treatment adherence and data-driven insights, while those from non-profits and research institutions tend to adopt more holistic approaches aligned with diverse patient needs, although sometimes lacking scalability. The integration of AI-driven functionalities, while promising, underscores the need for ecosystem-wide alignment to ensure interoperability, trust, and sustainability, further reinforcing H1 (Chedrawi et al., 2025; Colther & Doussoulin, 2024).
Regarding RQ2 and H2, this study confirms that low adoption rates among Spanish MS patients persist despite high reported interest in digital health technologies. The survey data indicate a mean weekly usage of 55.5 min with high variance, suggesting limited sustained engagement for several users. Numerous factors have been identified, including significant usability challenges, a notable lack of integration with healthcare providers, and limited language support, with only 45 % of analyzed apps available in Spanish. The discrepancy between reported interest in advanced features such as IoT devices and cognitive tests, and their actual low usage, emphasizes potential digital literacy gaps that hinder effective adoption. Furthermore, our analysis reveals systemic misalignments beyond individual app functionalities, such as platform fragmentation, the absence of robust funding models for free apps, and insufficient clinical integration. These structural barriers prevent seamless embedding into clinical workflows and patient routines, thereby limiting sustained, shared value within the broader ecosystem and directly substantiating H2. The ethical concerns related to data privacy and transparency in AI-driven insights represent a significant barrier to trust and adoption.
One of the most remarkable results is a strong acceptance of both IoT devices and cognitive tests that assist clinicians in assessing the progression of a disease. In general, patients have expressed their willingness to use such tools, mainly in the cases of enhancing knowledge concerning their condition and contributing to the greater good, as it pertains to MS. However, such willingness differs from the observed low adoption rates, prompting an unplanned observation: the possible lack of digital skills among some patients. The reasons for this discrepancy remain unknown, although it forms a significant limitation not foreseen at the research design stage.
Based on these findings, we offer the following practical recommendations for key stakeholders and suggest specific directions for future research, such as prioritization of patient-centered design for app developers, moving beyond basic tracking to incorporate highly valued features such as cognitive stimulation, emotional support, and personalized physical activity tools, while ensuring intuitive usability to overcome adoption barriers. Crucially, enhancing transparency around data privacy, sharing, and AI use is essential for building trust and establishing ethical governance. Developing apps with robust interoperability for seamless integration into clinical workflows and diversifying language support, especially for Spanish-speaking populations, are vital steps.
This study presents several straightforward implications for clinicians, developers, and patients. First, the gap between patient-prioritized features (e.g., cognitive stimulation, emotional support, and individualized exercise advice) and most commonly offered functionalities (reminders, general education, or simple symptom diaries) suggests more patient-led design strategies. Developers should emphasize co-design, considering patients and clinicians as key stakeholders for the features in the app to reflect real requirements, not technically convenient ones.
Second, the shared usability, digital literacy, and accessibility problems imply imperative demands for inclusive design best practices. These include simpler interfaces, adaptive options for different physical or cognitive capabilities, and improved support for multilingualism. Solving these would directly promote adoption and reduce inequalities in digital health access.
Third, a failure to integrate with established care pathways has significant practical implications: without clinical endorsement, apps are seen as add-on or ancillary tools. Clinicians and healthcare organizations should therefore be encouraged to integrate approved apps into clinical workflows, including prescription processes and routine follow-up, as a way of endorsing these tools and building patient trust.
Fourth, the issue of trust and transparency highlights the importance of robust governance frameworks. Patients are willing to engage with digital means when data protection, ownership, and sharing protocols are well delineated. Institutional and regulatory stakeholders play a critical role in developing guidelines that balance innovation and privacy and accountability.
Finally, sustainability is a cross-cutting theme. A majority of the applications are poorly maintained and cost-limited, thereby reducing patient confidence. Financing business models that allow for long-term maintenance and clinical validation are critical to preventing premature abandonment and fragmentation of the digital health space.
Healthcare professionals are encouraged to actively co-create and evaluate MS apps, integrating validated, high-quality tools into care pathways to support self-management and data collection. Providing digital literacy support to patients can bridge the gap between interest and actual usage.
Policymakers and healthcare organizations should develop standardized frameworks fostering wider ecosystem cooperation among stakeholders and reimbursing digital health tools to ensure quality. Fostering public-private partnerships and exploring hybrid monetization models can secure long-term sustainability and continuous improvement for MS apps. Furthermore, investing in digital infrastructure and educational initiatives is critical for enhancing digital literacy among both patients and providers.
Future research should build on these insights by examining how specific design interventions (e.g., adaptive cognitive interfaces, multilingual versions, embedded clinical recommendations) affect adoption in practice. Longitudinal studies should be included to track the long-term impact of MS apps on patient outcomes and engagement, providing robust efficacy evidence. Moreover, comparative research across different cultural and health system contexts can extend the generalizability of these findings and inform globally relevant design principles. Moreover, designing and evaluating targeted interventions that improve digital literacy and technical competence among MS patients can foster greater adoption. Further investigation into multidisciplinary co-creation models involving all stakeholders across the app lifecycle, alongside exploring viable economic sustainability models beyond current free offerings, is necessary. Finally, research into the ethical implications of AI integration, focusing on patient trust, algorithmic bias, data governance, and regulatory compliance, is crucial for responsible innovation.
Equipping patients with more advanced digital skills is anticipated to reinforce their role in the app market, attracting further feature development targeted at their needs. However, elucidating the main motivators for these app developers to continue maintaining or scaling such digital tools is essential. Investigating their vision for sustainability and commitment to social contributions can be crucial for informing the next steps. These aspects are to be focused on with priority in the near future, fostering an ecosystem where digital health solutions are not only technologically advanced but also equitably accessible, highly usable, and deeply integrated into patient care pathways.
CRediT authorship contribution statementMercedes Grijalvo: Writing – review & editing, Writing – original draft, Validation, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Joaquín Ordieres-Meré: Writing – review & editing, Writing – original draft, Validation, Methodology, Funding acquisition, Formal analysis, Data curation, Conceptualization. Manuel Uche-Soria: Writing – review & editing, Methodology, Investigation, Data curation, Conceptualization. Bernardo Tabuenca: Writing – review & editing, Methodology, Investigation, Data curation, Conceptualization. Yolanda Aladro-Benito: Writing – review & editing, Methodology, Investigation, Conceptualization.
Acknowledgment
The authors would like to thank the MS patient association AEDEM-COCEMFE, Asociación Española de Esclerosis Múltiple; FEMM: Fundación Esclerosis Múltiple Madrid; and EME: Esclerosis Múltiple España for their engagement and animating the participation of patients in this research.