Cancer can be extremely disruptive, triggering high levels of distress, and at the same time transformative, promoting perceptions of positive life changes and growth. This study aims to analyze the psychometric proprieties of the Stress-Related Growth Scale Short-Form (SRGS-SF) in cancer patients.
Method209 Cancer patients heterogeneous in disease stage and diagnosis completed: clinical and sociodemographic information, Distress Thermometer, Positive and Negative Affect Schedule, Visual-analogue Scale of Perceived Positive Life Changes, and Stress-Related Growth Scale-Short Form.
ResultsThe analysis of internal structure pointed to an one-dimensional scale, with high reliability (.92) measured through the McDonald`s omega coefficient. Validity was also evidenced through significant correlations with other variables.
ConclusionsThe Portuguese version of the SRGS-SF seems to present the necessary psychometric proprieties to be considered a valid and reliable short tool, to assess perceptions of growth following cancer and contribute to targeted and integrative psycho-oncological interventions.
El cáncer puede ser extremadamente disruptivo y transformador al mismo tiempo, provocando altos niveles de angustia que pueden promover la percepción de cambios positivos en la vida y crecimiento. Este estudio tiene como objetivo analizar las propiedades psicométricas de la Stress-Related Growth Scale-Short Form (SRGS-SF) en pacientes con cáncer.
Método209 pacientes con cáncer heterogéneo en estadio de la enfermedad y diagnóstico han completado información clínica y sociodemográfica, Distress Thermometer, Positive and Negative Affect Schedule, Escala visual-analógica de los cambios de vida positivos percibidos y Stress-Related Growth Scale-Short Form.
ResultadosEl análisis de la estructura interna apuntó una estructura unifactorial con índices de ajuste adecuados y una alta fiabilidad (.92) evaluada a través del coeficiente omega de McDonald. La validez fue proporcionada a través de la evidencia de correlaciones significativas con otras variables.
ConclusionesLa versión portuguesa del SRGS-SF parece presentar las propiedades psicométricas necesarias para ser considerada una herramienta corta válida y confiable, para evaluar las percepciones de crecimiento después del cáncer y contribuir para intervenciones psico-oncológicas específicas e integradoras.
Human beings are often faced with challenges that can inflict different degrees of instability, suffering, uncertainty and incomprehension. For triggering a cascade of physical, psychosocial, practical and existential demands (Denlinger et al., 2020; McCarter et al., 2020; Riba et al., 2019), the diagnosis of a cancer and the anticancer multimodal treatments, can constitute one of these disruptive stressful life events, sometimes even traumatic (Cordova et al., 2017; Kaster et al., 2019; Marziliano et al., 2020; Ochoa et al., 2017). Therefore, cancer diagnosis and treatment are associated with increased risk for emotional distress and mental comorbidity (Alarcón et al., 2020; Gil-Moncayo et al., 2020; Götz et al., 2019; Kuba et al., 2019; Mehnert et al., 2018; Zebrack et al., 2017). Studies show that approximately 40% of the cancer patients had a psychiatric disorder (Derogatis et al., 1983; Mitchell et al., 2011; Reilly et al., 2013). However, for its nature, cancer can be simultaneously conceptualized as a major chronic stressor that can be a seismic event, threatening balance, and an end of life awareness trigger, and an event with the potential to capitalize the imminent ability of human beings to self-actualize and grow in a suffering circumstance (Casellas et al., 2017; Cordova et al., 2017; Marziliano et al., 2020; Ord et al., 2020; Rzeszutek et al., 2020; Tremolada et al., 2018).
The emergence of these positive transformations in a suffering scenario shows that distress and growth are not antagonistic realities – they coexist (Carver et al., 2009; Casellas et al., 2017; Marziliano et al., 2020; Ord et al., 2020; Park, 2009). For Ochoa and colleagues (2019) stress and growth are not independent or dichotomic responses to cancer. They reflect, instead, a dynamic continuum that fluctuates between these two extremes of human adjustment to cancer. According to growth models, perceived growth is not a direct outcome of trauma and distress, but results from the person's struggle with the new and painful reality triggered by the confrontation with a life-threatening disease (Casellas et al., 2017; Li et al., 2020; Rzeszutek et al., 2020). In cancer patients, both processes, post-traumatic stress and growth, have as a common basis, the threat to one's physical or psychological integrity. Both begin with a common precursor, that is the perception of vulnerability, which triggers the stress-growth response (and the inherent cognitive and emotional mechanisms) associated with the psychological adjustment to cancer (Ochoa et al., 2019). However, while it is clear that greater levels of threat and cancer-related distress are precursors to growth, the association between distress and growth during cancer trajectory is still unclear (Carver et al., 2009; Holtmaat et al., 2017; Lelorain et al., 2010).
For Casellas and colleagues (2017), the study of growth in psycho-oncology is particularly relevant, once cancer is the medical condition where growth is most addressed, and that better mirrors the complex interface between the physical and psychological factors.
According to Park (2009), there has been many terminologies to define the positive life changes and emergence of growth, featuring the concepts of Stress-Related Growth (SRG), Posttraumatic Growth (PTG), and Benefit Finding (BF). Although, globally, all of them reveal a similar psychological phenomenon, the Stress-Related Growth seems to provide a more comprehensive view on the adjustment process to adversity and illness compared to the others (Park & Fenster, 2004). At the same time, it holds a more balanced position regarding the nature of changes, not considering them as a mere illusion or short‐term benefits (BF) nor veridical, deep and with a radical character (PTG) (Casellas et al., 2017; Frazier et al., 2009; Park, 2009; Park et al., 2010).
Considering this distinction, SRG seems to be the most suitable to identify the perception of positive changes liable to be experienced and intervened in a larger cohort of cancer patients. For this reason, and considering the symptoms inherent to disease and treatments (e.g., fatigue, apathy, dyspnea, concentration problems), the Stress-Related Growth Scale–Short Form (SRGS-SF), for being a brief measure, is seen as a proper and pertinent measure to assess and develop broader interventions with this population. In regard to this, the evidence alerts that it is important that psycho-oncological interventions incorporate the combination of stress and growth responses in order to achieve a constructive and adaptive balance of both stress-growth adjustment responses (Ochoa et al., 2017, 2019). In addition, in Portugal there is only one validated measure to assess growth, the Posttraumatic Growth Inventory (Tedeschi & Calhoun, 1996), that is validated for different samples: breast cancer (Silva et al., 2009; 21 items; alpha coefficient: .94), cancer caregivers (Teixeira & Pereira, 2013; 21 items; alpha coefficient: .94), divorced adults (Lamela et al., 2014; 10 items; alpha coefficient: .88), and subjects with at least one traumatic event during their lifetime (Resende et al., 2008; 21 items; alpha coefficient: .95).
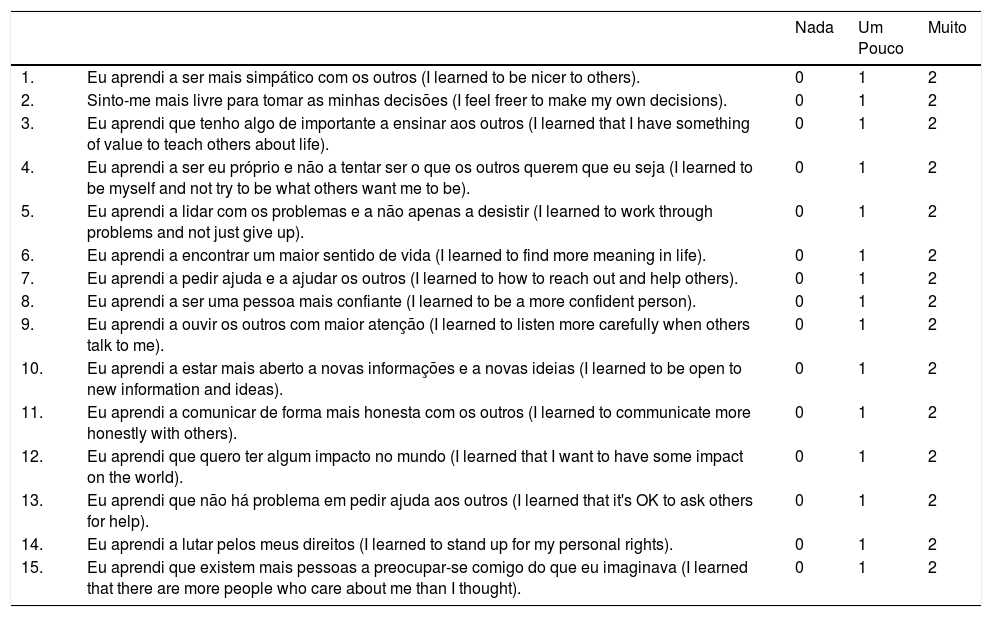
The Stress-Related Growth Scale (SRGS), originally developed by Park et al. (1996), emerged as the first attempt to quantify self-reported positive outcomes following a stressful event. It comprises 50 items that aim to evaluate how much a person perceived positive changes in personal resources, social relationships, life philosophy and/or coping skills, as a result of the past year`s most stressful encounter (Park et al., 1996; Park & Lechner, 2006). Evidence supported good psychometric proprieties (α coefficient .94; test-retest reliability .81) in this original measure (Park et al., 1996), as well as in the studies where it was administered (see Linley & Joseph, 2004). Based on this original formulation, a shorter version with 15 items was developed through the highest item-total score correlations comparison between two samples (college students and adult church members), which revealed a good agreement, leading to the formulation of the final 15-items version (Cohen et al., 1998). The investigations that used this version found good alpha coefficients: .88 (Park & Blumberg, 2002), .93 (Frazier et al., 2004), .92 (Park, 2005), .91 (Caserta et al., 2009), and .95 (Steger et al., 2015). Although this scale proves to be an asset, capable to evaluate the same dimensions, to the best of our knowledge only one validation study was performed (Li et al., 2018), in a sample of Chinese undergraduate nursing students. Two factors were found, interpersonal and intrapersonal growth, with alpha coefficients of .92 and .87, respectively, and .90 for the overall scale.
Taking into consideration, the potential importance of perceived growth in the dynamic stress-growth adjustment to cancer and interventions effectiveness; the fact that in Portugal there is a single validated measure, which assesses a different construct, it is longer and it has been validated in a cancer sample only with women and with a single diagnosis, therefore we sought to validate in Portuguese the short-form of SRGS (Park et al., 1996).
MethodParticipantsThis is a convenience sample that comprised a total of 209 cancer patients selected in an Oncology Day Care (ODC) unit of a Portuguese north cancer center. All the participants were assessed in an ODC clinical setting by a Psychologist. Eligibility criteria consisted of: age range between 18 and 80 years; receiving treatment in an Oncology Day Care unit; ability to speak and read Portuguese; absence of major neurological and psychiatric disabilities; willingness to complete the screening questionnaire.
The sample comprised 162 female (77.5%) and 47 male (22.5%) receiving anticancer treatment. The mean age was 52.17 years, ranging from 26 to 79 years (SD = 10.84). Most were married (81.8%) and the rest were single (2.9%), divorced (6.7%), widowed (3.8%) and lived in a civil partnership (4.8%). In regard to academic training, the majority is represented by 27.3% with university education, 24.9% with primary school and 22.5% with high school. 40.2% of the participants had a non-qualified job (of 209 participants, 74.6% were not working at the moment: on a sick leave or retirement). Participants were distributed to cancer site as follows: breast (57.9%), digestive tract (18.7%), lung (7.7%), blood (5.7%), gyneco-urological (5.3%), head and neck (3.3%) and bones, skin and tissues (1.4%). 59.4% were receiving primary treatment, 31.1% were being treated after a recurrence and 9.6% were undergoing palliative treatment. The mean time since diagnosis was 26.89 months, ranging from 2 to 168 months (SD = 32.25). The majority of participants (83.7%) will receive or had already received at least two treatments during the disease course.
MeasuresSociodemographic and clinical data sheet. This questionnaire evaluates demographic (gender, age, marital status, educational level, professional and employment status) and medical data (cancer site and stage, time since diagnosis, treatment protocol).
Stress-Related Growth Scale–Short-Form (SRGS-SF; Park et al., 1996). This measure aims to evaluate the perception of positive changes in personal resources, social relationships, life philosophy and coping skills following a disruptive or traumatic event (Park et al., 1996; Park & Lechner, 2006), in a Likert scale scored on 3 points: 0 = not at all; 1 = somewhat; 2 = a great deal. Higher scores indicate a greater perception of personal growth in the aftermath of a highly stressful situation.
Perceived Positive Life Changes (PPLC). The PPLC is a one-item visual analogue self-report scale that authors created in order to obtain a direct evaluation of the perception of positive life changes resulting from the cancer experience and its emotional impact. It consists of an 11-point continuum ranging from 0 (Didn't experience any positive life change) to 10 (I experienced intense positive life changes) in order to respond the question: “Following your cancer diagnosis and everything that it has involved in your life so far, what is the perception of experiencing positive life changes in yourself and/or your life?”. The higher the score obtained, the greater the perception of positive life changes in current daily life.
Positive and Negative Affect Schedule (PANAS; Watson et al., 1998; Portuguese version Galinha & Pais-Ribeiro, 2005). This assessment tool emerged from the need to develop a brief and simple measure to evaluate positive and negative affect in different clinical and nonclinical populations (Watson et al., 1998). PANAS comprises two subscales (Positive and Negative affect), each with 10 items (Galinha & Pais-Ribeiro, 2005; Watson et al., 1998). Items are rated on a five-point Likert-type scale that ranges from 1 (nothing or very slightly) to 5 (extremely). Higher scores on each of the subscales indicate a higher level of positive and negative affect, respectively. Positive affect scale presented an α coefficient of .88 on the original version and of .86 on the Portuguese version. For the negative affect scale, α coefficient was .87 in the original tool and .89 in the Portuguese one (Galinha & Pais-Ribeiro, 2005; Watson et al., 1998).
Distress Thermometer (DT; Roth et al., 1998; Portuguese version Gil et al., 2005). The DT is a gold standard assessment composed by: a single-item visual-analogue self-report measure of psychological distress, presented in an 11-point scale that measures psychological distress in the last week on a continuum ranging from 0 (no distress) to 10 (extreme distress); and, by a standardized Problem List containing 34 potential causes of distress where respondents should indicate if they experienced the symptoms (yes or no) in the last week (Gil et al., 2005; Jacobsen et al., 2005; Roth et al., 1998). Higher scores are indicative of greater levels of emotional distress.
ProceduresStudy data came from a sample collected in a northern Portuguese cancer center that covers a large geographical region. A convenience sample was collected in the waiting areas of the ODC Unit. After receiving information and providing informed consent, participants completed a set of questionnaires that included a sociodemographic and medical data form, the SRGS-SF, the PPLC, the DT, and the PANAS.
For the SRGS-SF adaptation process, guidelines and stages recommended by Beaton and colleagues (2000) for cross-cultural adaptations of self-report measures were followed: translation, synthesis, back translation, expert committee review and pretesting.
The study method, procedures, materials and documents were previously approved by the institutional Ethics Committee (Ref. CES.77/015) and by the ODC unit director.
Statistical methodsStatistical analyses were performed using IBM SPSS v.26. Analysis were conducted in different stages. First, study variables were described through descriptive statistics. Second, item analysis was performed using descriptive statistics, and inter-items and corrected item-total correlations estimated through Pearson product-moment coefficients. Associations were interpreted according to Cohen`s (1988) values. No missing data were found and data distribution was in accordance with the distribution by the normal curve (Kline, 2005). Third, the internal structure was analyzed using Exploratory Factor Analysis (EFA). To ensure the suitability and factorability of data, the ratio of observations per item was verified (higher than 10:1), inter-item correlations were inspected, and Bartlett`s test of sphericity, and Kaiser-Meyer-Olkin (KMO) index were determined. Considering the ordinal nature of the data, the Unweighted Least Squares extraction method was chosen. To determine the number of factors to retain, a parallel analysis procedure was used (Goretzko et al., 2019). Final decision regarding the number of factors to retain combined conceptual considerations attended in the original measure and in the previous studies with the SRGS-SF (Goretzko et al., 2019). Fourth, considering the ordinal nature of the data, reliability was estimated using the McDonald`s omega coefficient (Gadermann et al., 2012). Fifth, validity evidence based on relationships with other variables was obtained by Pearson's correlations between scores on the SRGS-SF and scores on the following measures: DT, PPLC and PANAS. Results were interpreted according to the Cohen`s criteria (Cohen, 1988). Finally, after having verified that scores on the SRGS-SF indicated adequate psychometric proprieties, descriptive statistics for their interpretation were presented.
ResultsDescriptive from study variablesThis sample constituted by 209 cancer patients presented the following results for the variables under analysis: Distress [M = 4.53, SD = 2.50; range 0-10]; PPLC [M = 4.33, SD = 3.20; range 0-10]; PANAS negative affect subscale [M = 17.38, SD = 6.75; range 10-50]; PANAS positive affect subscale [M = 26.48, SD = 8.76; range 10-50].
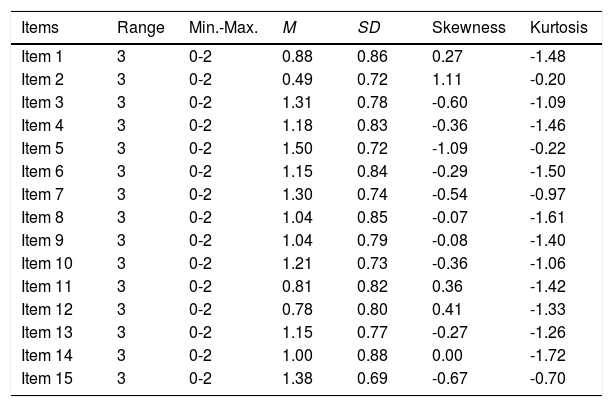
Preliminary item analysis from SRGS-SFDescriptive statistics for SRGS-SF items are introduced in Table 1. Items presented absolute values of skewness and kurtosis within the accepted limits for a normal distribution.
Descriptive statistics for SGRS-SF 15 items (raw metrics).
Note. Min. = Minimum; Max. = Maximum; M = Mean; SD = Standard Deviation.
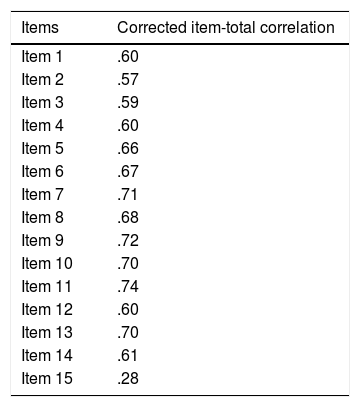
Relations between the 15 items showed that all inter-items correlations were significant and medium to large (ranging from .32 and .66), except for item 5 that presented a correlation value below .30 with item 2 (.26), and for item 15, which correlated weakly with most of the items (ranging from .19 and .31) and did not present significant correlations with items 2 and 14. Corrected item-total correlation coefficients for the 15 items were large and ranged between .57 and .74, except for item 15 that presented a small correlation (.28) (Table 2).
Validity evidence based on internal structureMost inter-item correlations showed an r greater than .30, Bartlett`s test of sphericity presented a significant value (p < .001), and Kaiser-Meyer-Olkin (KMO) index scored 0.91, reflecting sampling adequacy to fit EFA model.
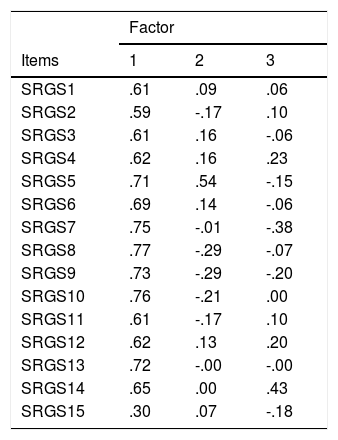
Unweighted Least Squares extraction method was used. The communalities range from .40 to .84, excepting item 15 that presented a .13 value. The first three eigenvalues (7.18; 1.06; 1.03) explain a total of 53.42% of the variance. According to parallel analysis procedure, only one factor should be retained (first three eigenvalues in Monte Carlo simulation were: 1.4816, 1.3705, 1.2873). The one-factor solution explained a total of 45.03% of the variance. This data are consistent with previous research on the original SRGS and on the 15-item version that, except in Li and colleagues (2018) study, advocate the single-dimensionality of the measure. Considering the unifactorial structure of the data, the hypothesized rotation method using the oblimin solution was not performed. The factor matrix is displayed on Table 3.
Factor matrix.
Note. The extraction method was the Unweighted Least Squares.
The McDonald`s omega coefficient was .92, which indicates an adequate reliability for scores on the Portuguese version of the SRGS-SF.
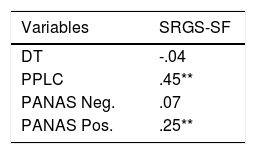
Validity evidence based on relationships with other variablesData revealed that scores on the SRGS-SF yielded positive and significant correlations with scores on positive affect and PPLC. The correlations between SRGS-SF scores and the scores on negative affect and DT did not present significant values (Table 4).
Pearson product-moment correlation: r value and significance (N = 209).
Note. DT = Distress Thermometer; PPLC = Perceived Positive Life Changes; PANAS Neg. = Positive and Negative Affect Schedule: negative affect subscale; PANAS Pos. = Positive and Negative Affect Schedule: positive affect subscale; SRGS-SF = Stress-Related Growth Scale–Short Form. ** p < .01.
The scale is scored by summing the item scores that range between 0 and 2. Hence, the total score range from 0 and 30. Higher scores on the SRGS-SF indicate greater perceived growth. Scores in the present sample ranged from 0 to 30, with a mean of 16.22 (SD = 8.11) and a median of 16.00. Scores of 9.25, 16.00 and 23.75 corresponded respectively to the first, second and third quartiles.
DiscussionThis study examines the internal structure and psychometric proprieties of the Portuguese version of the SRGS-SF in a cancer patient's sample. Regarding internal structure, and using the Unweighted Least Squares extraction method, results support a single factor solution. Except for item 15, inter-items correlations were significant and medium to large and corrected item-total correlations were high. This solution seems to confirm the single-factor structure reported in the original 50-item version (Park et al., 1996), and in several studies (e.g., Caserta et al., 2009; Frazier et al., 2004; Park, 2005; Park & Blumberg, 2002; Steger et al., 2015). Inversely, Li and colleagues (2018) found a two-factor structure in their validation, but reinforced that growth have specific dimensions and correlations that may be different across cultures. Although item 15 presented lower values than the remain, since it correlates significantly with almost all items and total-score and it loads with the acceptable value of .30, it was maintained.
These findings indicate that the total scale score provide a measure of the construct SRG, with higher scores corresponding to higher levels of personal growth in respondents. Scores also showed adequate reliability, similar to the 50-item original version (Park et al., 1996) and to the studies that used the 15-item version (Casserta et al., 2009; Frazier et al., 2004; Park & Blumberg, 2002).
Relationships with other variables seems to evidence the scale validity. As expected (Casellas et al., 2017; Lelorain et al., 2010; Linley & Joseph, 2004; Ochoa et al, 2019; Ord et al., 2020; Park, 2009; Park et al., 1996), a positive and significant association between SRG and positive affect and PPLC. Also, in line with literature (Carver et al., 2009; Casellas et al., 2017; Holmaat et al., 2017; Lelorain et al., 2010; Marziliano et al., 2020; Ochoa et al., 2019), revealed no correlation, or very weak, between SRG and distress levels and negative affect. This happens because, although the distress and the patient's struggle with disease are precursors of growth, both responses coexist in the cancer`s adjustment process (Carver et al., 2009; Li et al., 2020; Ochoa et al., 2019).
The mean score of the SRGS-SF in the present sample (M = 16.22) was lower than that reported with students ‘samples (Li et al., 2018; Park & Blumberg, 2002), and similar to that observed in bereaved people (Casserta et al., 2009) and, more recently, in military veterans (Steger et al., 2015).
One of the limitations of the present study is that we used convenience sampling with all participants being recruited in a ODC and undergoing chemotherapy. Another issue concerns the fact that our pilot study to test the translation was stopped after 10 patients presented no doubts. Another limitation is that item 15 does not behave as the remaining ones concerning the inter-item correlations and the factor loading. Despite these limitations, this investigation showed that the Portuguese version of the SRGS-SF have adequate psychometric proprieties.
In conclusion, the Portuguese version of the SRGS-SF (see Appendix A) showed satisfactory psychometric proprieties in the sample studied. The instrument is brief and easy to apply and may be administered in both clinical and research contexts, particularly in psycho-oncology. Considering the distress-growth adjustment continuum to cancer (Ochoa et al., 2019), this tool could contribute to a broader understanding of the dynamics established between the disease appraisals, distress levels, emerging positive life changes, and adopted coping efforts during cancer. This will facilitate the development of integrative and effective targeted interventions in cancer settings.
FundingThis work was funded by the Center for Psychology at the University of Porto, Foundation for Sciences and Technology Portugal (FCT UIDB/ 00050/2020).
Por favor, responda a cada questão com: "0" (nada), "1" (um pouco), ou "2" (muito).
Por causa deste diagnóstico/desta doença…